Table of Contents
Introduction
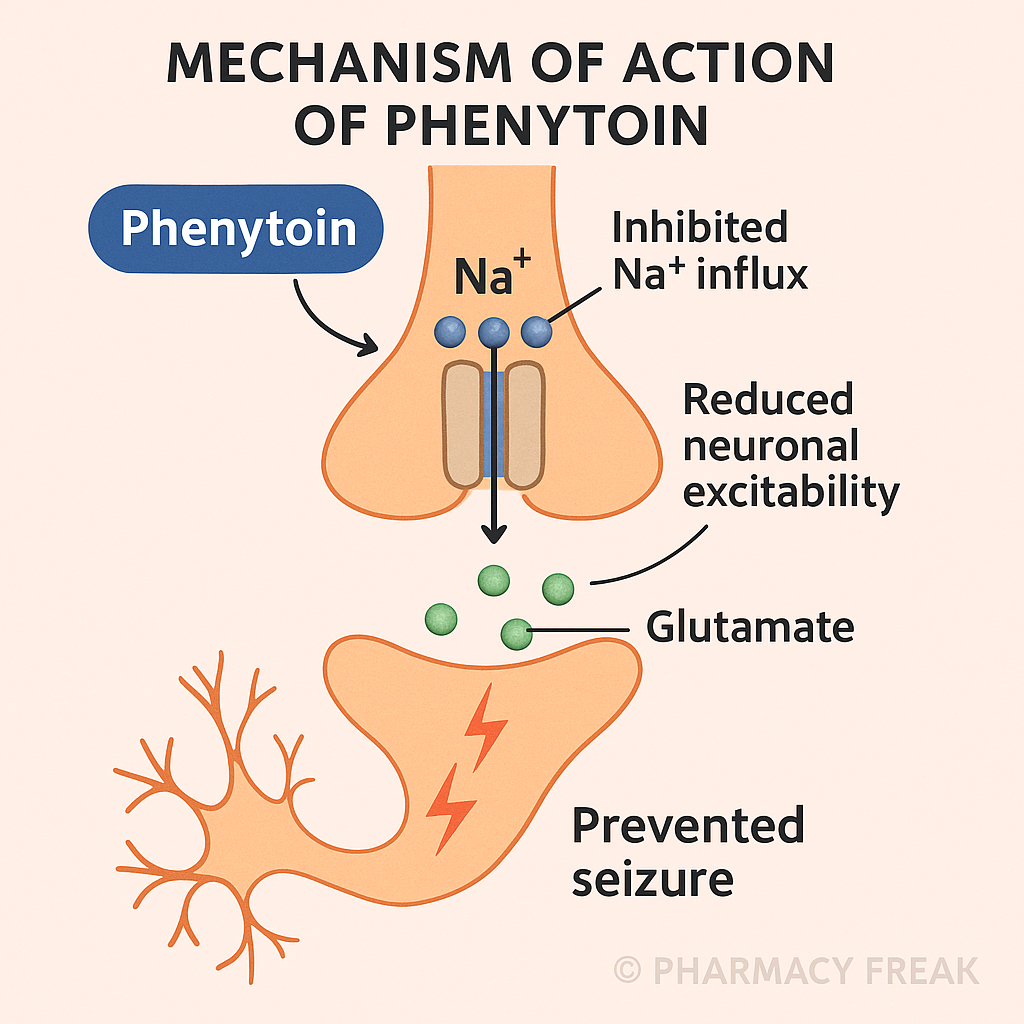
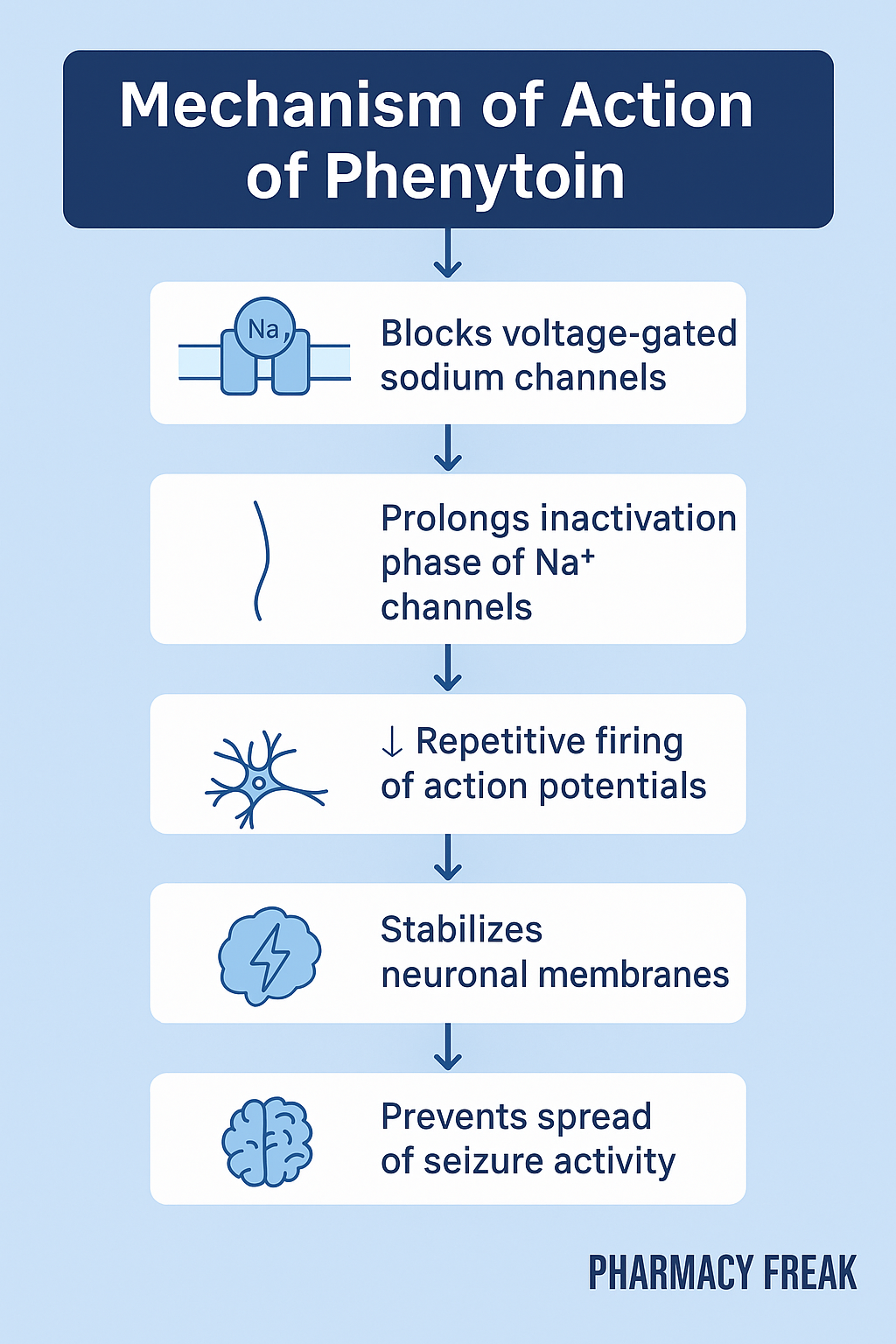
Phenytoin is one of the oldest and most widely used antiepileptic drugs (AEDs), primarily for treating focal seizures and generalized tonic-clonic seizures. It has a well-known profile, acting on voltage-gated sodium channels to reduce high-frequency neuronal firing. Despite newer alternatives, phenytoin remains important, especially in emergency settings like status epilepticus (IV use).
It’s a high-yield topic in USMLE, NCLEX, GPAT, and NEET-PG due to its pharmacokinetics, side effects, and drug interactions.
Stepwise Mechanism of Action of Phenytoin
- Voltage-gated Na⁺ channel blockade
Phenytoin binds to voltage-gated sodium channels in their inactivated state, prolonging inactivation and preventing repetitive neuronal firing. - Use-dependent (state-dependent) blockade
The drug shows use-dependence, meaning it preferentially acts on active neurons, which fire frequently, making it ideal for suppressing seizure foci. - Inhibition of sustained high-frequency action potentials
Phenytoin prevents the spread of seizure activity by stopping sustained, rapid depolarization. - Stabilization of neuronal membranes
By reducing excitability, phenytoin stabilizes neuronal membranes and lowers seizure threshold.
Pharmacokinetic Parameters of Phenytoin
| Parameter | Value |
|---|---|
| Bioavailability | 70–90% (oral) |
| Half-life | 7–42 hrs (dose-dependent kinetics) |
| Metabolism | Hepatic via CYP2C9, CYP2C19 |
| Protein binding | ~90% |
| Excretion | Renal (as inactive metabolites) |
| Therapeutic range | 10–20 μg/mL |
| Kinetics | Zero-order at high doses |
Clinical Uses of Phenytoin
- Generalized tonic-clonic seizures
- Focal (partial) seizures
- Status epilepticus (IV form, loading dose)
- Seizure prophylaxis in head trauma
- Trigeminal neuralgia (off-label)
Adverse Effects of Phenytoin
- CNS effects – Nystagmus, ataxia, confusion
- Gingival hyperplasia
- Hirsutism
- Megaloblastic anemia (↓ folate absorption)
- Peripheral neuropathy
- Drug-induced lupus
- Stevens-Johnson Syndrome (SJS)
- Osteomalacia (↓ vitamin D metabolism)
- Teratogenicity – Fetal hydantoin syndrome
- Hepatotoxicity
- Skin rash
Comparative Analysis: Phenytoin vs Levetiracetam
| Feature | Phenytoin | Levetiracetam |
|---|---|---|
| MOA | Na⁺ channel blocker | SV2A modulation |
| Drug interactions | Many (CYP inducer) | Minimal |
| Sedation | Low | Mild/moderate |
| Gingival hyperplasia | Common | Rare |
| Teratogenicity | Fetal hydantoin syndrome | Safer in pregnancy |
| Kinetics | Zero-order at high doses | Linear |
Practice MCQs
Q1. Phenytoin primarily acts on which ion channel?
a. Calcium channels
b. Potassium channels
c. Sodium channels ✅
d. Chloride channels
Q2. The kinetics of phenytoin at high doses is:
a. First-order
b. Zero-order ✅
c. Mixed
d. None
Q3. A classical side effect of phenytoin is:
a. Gingival hyperplasia ✅
b. Alopecia
c. Anemia
d. Ataxia
Q4. Phenytoin is indicated for:
a. Absence seizures
b. Myoclonic seizures
c. Status epilepticus ✅
d. Febrile seizures
Q5. Which vitamin deficiency can occur with phenytoin?
a. Vitamin A
b. Vitamin D ✅
c. Vitamin K
d. Vitamin B1
Q6. Phenytoin has high binding to:
a. Globulin
b. Plasma protein ✅
c. Albumin only
d. RBCs
Q7. What happens when phenytoin exceeds its metabolic capacity?
a. Increased absorption
b. Toxicity due to zero-order kinetics ✅
c. Rapid elimination
d. Decreased half-life
Q8. Which of the following is teratogenic with phenytoin use?
a. Spina bifida
b. Neural crest defects
c. Fetal hydantoin syndrome ✅
d. Ebstein anomaly
Q9. Phenytoin-induced anemia is due to:
a. Iron deficiency
b. B12 deficiency
c. Folate deficiency ✅
d. Hemolysis
Q10. Phenytoin is metabolized by:
a. CYP3A4
b. CYP2D6
c. CYP2C9 and CYP2C19 ✅
d. UGT
FAQs
Q1: Can phenytoin be used for absence seizures?
No. It is ineffective and may worsen absence seizures.
Q2: Why does phenytoin require careful dosing?
Because it exhibits zero-order kinetics, small dose changes can cause toxicity.
Q3: How should IV phenytoin be administered?
Slowly, not exceeding 50 mg/min, to avoid cardiac arrhythmias.
Q4: What is fetal hydantoin syndrome?
A congenital syndrome with cleft lip, growth retardation, facial anomalies, and mental retardation due to phenytoin use in pregnancy.
Q5: Why monitor liver function with phenytoin?
It is hepatically metabolized and may cause liver damage with long-term use.
References
NCBI: https://www.ncbi.nlm.nih.gov/books/NBK482370/
KD Tripathi – Essentials of Medical Pharmacology
Goodman & Gilman – The Pharmacological Basis of Therapeutics
Review of Pharmacology – Sparsh Gupta

I am pursuing MBA in pharmaceutical management from NIPER Hyderabad with a strong academic record and proven success in national-level pharmacy entrance exams. I secured AIR 61 in NIPER 2024 (MS/M.Pharm) and AIR 27 in NIPER MBA, along with AIR 147 in GPAT 2024 and AIR 907 in GPAT 2023. I also achieved AIR 6 in AIIMS CRE-2025 for Drug Store Keeper and was selected as a Pharmacist (AIR 61) for ESIC. Additionally, I was the Runner-Up in Round 2 of the EY Case Study Competition.
At PharmacyFreak.com, I aim to guide future pharmacists through expert content, exam strategies, and insightful resources based on real experience and academic excellence.
Mail- harsh@pharmacyfreak.com