Table of Contents
Introduction
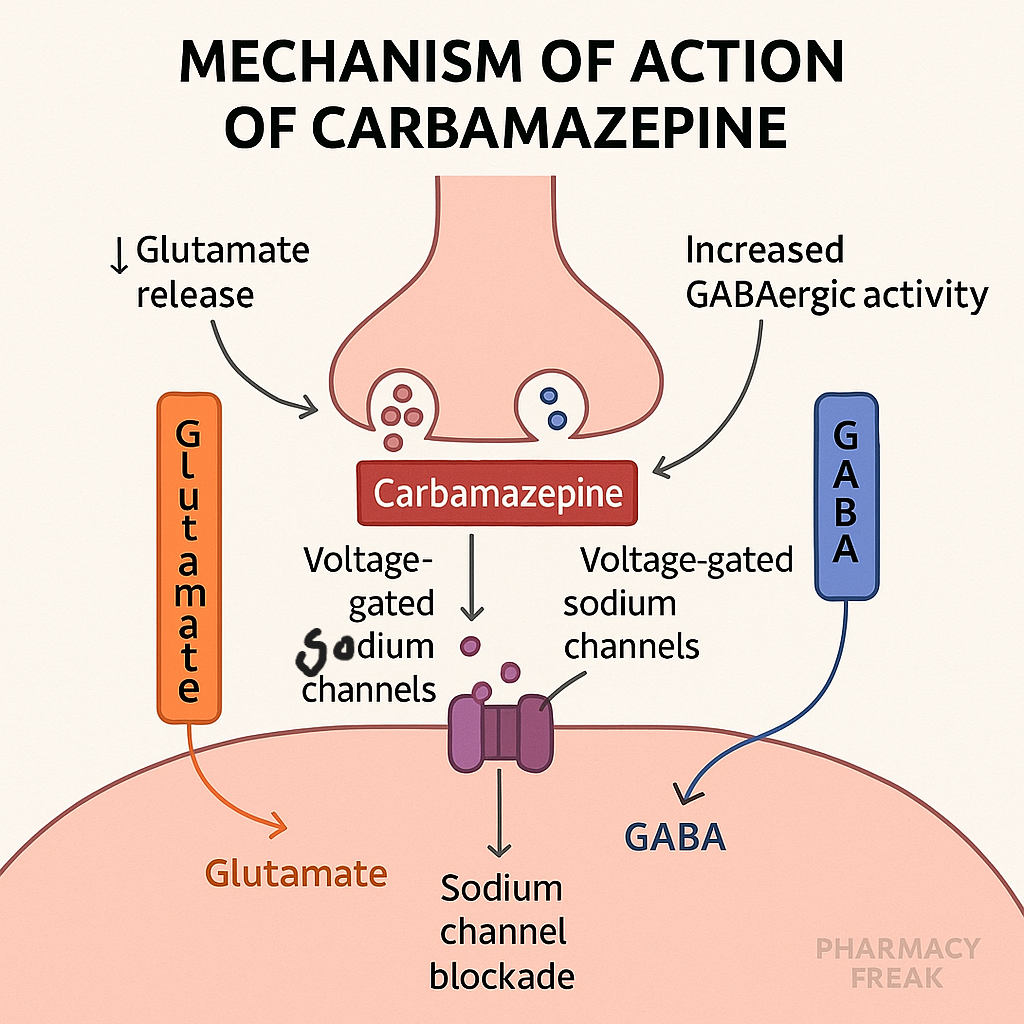
Carbamazepine is a classic antiepileptic drug (AED) and mood stabilizer. It is mainly used to treat partial and generalized tonic-clonic seizures, trigeminal neuralgia, and bipolar disorder. Its primary action involves blocking voltage-gated sodium channels, which stabilizes neuronal membranes and prevents repetitive firing.
It is frequently tested in pharmacology sections of USMLE, NCLEX, GPAT, and NEET-PG.
Stepwise Mechanism of Action of Carbamazepine
- Blockade of voltage-gated Na⁺ channels
Carbamazepine binds to the inactivated state of voltage-gated sodium channels, prolonging their inactivation and preventing repetitive neuronal firing. - Reduction of high-frequency firing
By inhibiting rapid firing of action potentials, carbamazepine reduces neuronal hyperexcitability, which is crucial in epilepsy control. - Inhibition of presynaptic neurotransmitter release
It may reduce the presynaptic release of glutamate, contributing to its anticonvulsant and mood-stabilizing effects. - Secondary GABA enhancement (minor)
Although not a primary action, it may enhance GABA-mediated inhibition indirectly in some regions.
Pharmacokinetic Parameters of Carbamazepine
| Parameter | Value |
|---|---|
| Bioavailability | 70–80% |
| Half-life | 25–65 hrs initially; 12–17 hrs (autoinduction) |
| Metabolism | Hepatic via CYP3A4 |
| Autoinduction | Yes – induces its own metabolism |
| Excretion | Renal (after hepatic metabolism) |
| Therapeutic range | 4–12 μg/mL |
Clinical Uses of Carbamazepine
- Partial seizures (focal onset)
- Generalized tonic-clonic seizures
- Trigeminal neuralgia (first-line)
- Bipolar disorder (alternative to lithium)
- Glossopharyngeal neuralgia
- Diabetic neuropathy (off-label)
Adverse Effects of Carbamazepine
- Diplopia and ataxia
- Sedation
- SIADH – leads to hyponatremia
- Aplastic anemia and agranulocytosis
- Hepatotoxicity
- Stevens-Johnson Syndrome (SJS), especially in HLA-B*1502 positive individuals (Asians)
- Teratogenicity – causes neural tube defects
- Autoinduction – reduced drug levels over time
Comparative Analysis: Carbamazepine vs Oxcarbazepine
| Feature | Carbamazepine | Oxcarbazepine |
|---|---|---|
| Sodium channel block | Yes | Yes |
| Autoinduction | Present | Minimal |
| Hyponatremia risk | High | Higher than carbamazepine |
| Hepatotoxicity | Yes | Lower risk |
| Active metabolites | Carbamazepine-10,11-epoxide | Less active |
Practice MCQs
Q1. Carbamazepine acts by blocking:
a. Calcium channels
b. GABA-A receptors
c. Sodium channels ✅
d. Potassium channels
Q2. What is the genetic risk factor for SJS with carbamazepine?
a. HLA-A0201
b. HLA-B1502 ✅
c. HLA-DR4
d. HLA-B*0702
Q3. Which adverse effect requires CBC monitoring?
a. Ataxia
b. Hyponatremia
c. Agranulocytosis ✅
d. Hepatitis
Q4. Which condition is treated first-line with carbamazepine?
a. Bipolar depression
b. Trigeminal neuralgia ✅
c. Status epilepticus
d. Absence seizures
Q5. What happens to carbamazepine levels over time due to autoinduction?
a. Increase
b. Remain stable
c. Decrease ✅
d. Unpredictable
Q6. Carbamazepine is contraindicated in which seizure type?
a. Tonic-clonic
b. Myoclonic
c. Absence ✅
d. Focal
Q7. What is the mechanism of hyponatremia with carbamazepine?
a. Nephrogenic DI
b. Inhibition of aldosterone
c. SIADH ✅
d. Hyperkalemia
Q8. Carbamazepine is metabolized primarily by:
a. CYP2C19
b. CYP3A4 ✅
c. CYP1A2
d. UGT
Q9. Therapeutic plasma level of carbamazepine is:
a. 2–6 μg/mL
b. 4–12 μg/mL ✅
c. 12–18 μg/mL
d. 18–25 μg/mL
Q10. Which adverse effect is associated with Asian ancestry?
a. Agranulocytosis
b. Hepatotoxicity
c. Stevens-Johnson Syndrome ✅
d. Ataxia
FAQs
Q1: Is carbamazepine used for absence seizures?
No. It can worsen absence seizures and should be avoided.
Q2: Why monitor sodium levels during therapy?
Carbamazepine can cause SIADH, leading to hyponatremia.
Q3: Can it be used in bipolar disorder?
Yes, as an alternative mood stabilizer when lithium is not tolerated.
Q4: What test should be done before starting in Asian populations?
HLA-B*1502 testing to avoid SJS/TEN.
Q5: Is it safe in pregnancy?
No. It’s teratogenic, associated with neural tube defects.
References
- KD Tripathi – Essentials of Medical Pharmacology
- Goodman & Gilman – The Pharmacological Basis of Therapeutics
- Sparsh Gupta – Review of Pharmacology
- NCBI: https://www.ncbi.nlm.nih.gov/books/NBK470284/

I am pursuing MBA in pharmaceutical management from NIPER Hyderabad with a strong academic record and proven success in national-level pharmacy entrance exams. I secured AIR 61 in NIPER 2024 (MS/M.Pharm) and AIR 27 in NIPER MBA, along with AIR 147 in GPAT 2024 and AIR 907 in GPAT 2023. I also achieved AIR 6 in AIIMS CRE-2025 for Drug Store Keeper and was selected as a Pharmacist (AIR 61) for ESIC. Additionally, I was the Runner-Up in Round 2 of the EY Case Study Competition.
At PharmacyFreak.com, I aim to guide future pharmacists through expert content, exam strategies, and insightful resources based on real experience and academic excellence.
Mail- harsh@pharmacyfreak.com