Table of Contents
Introduction
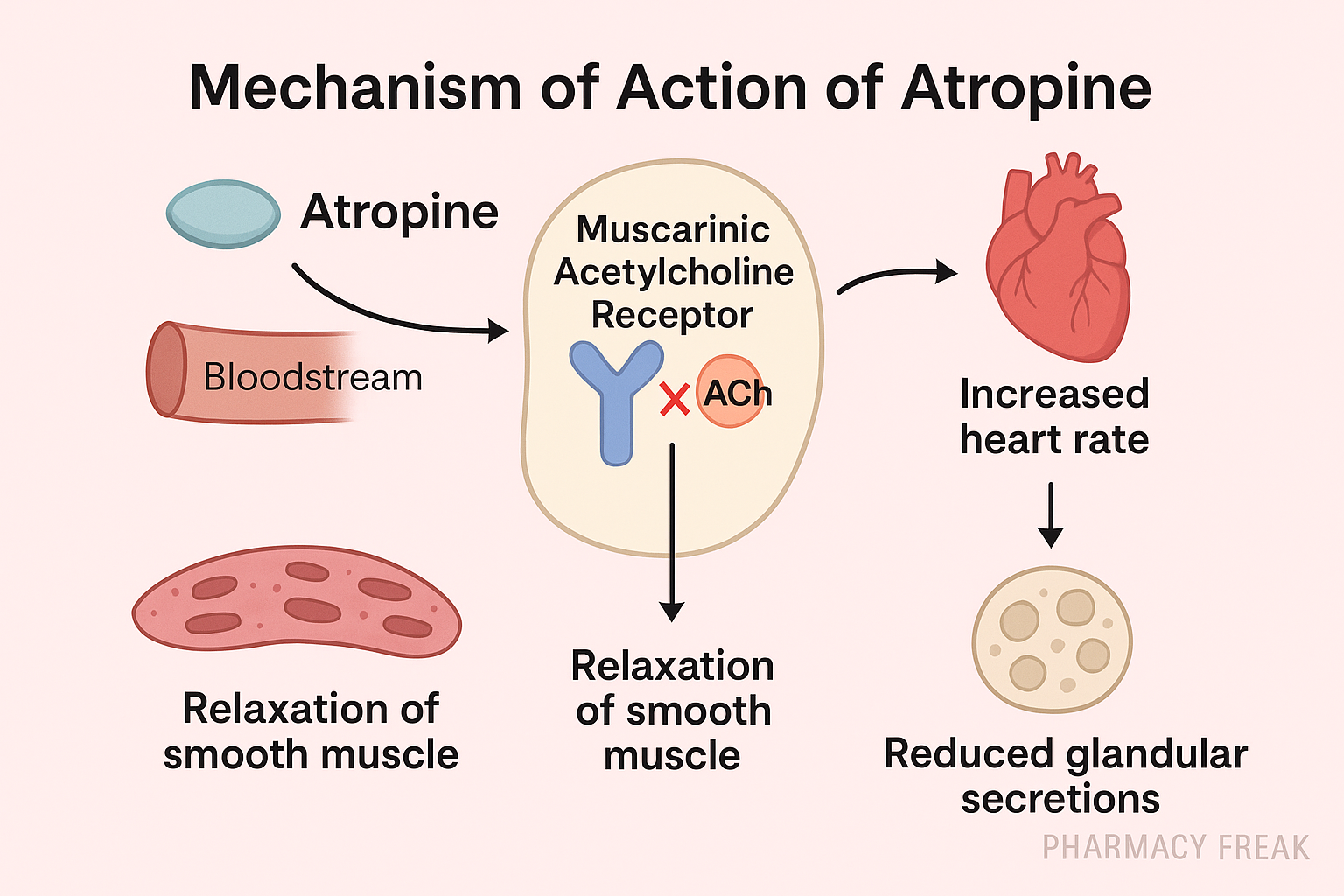
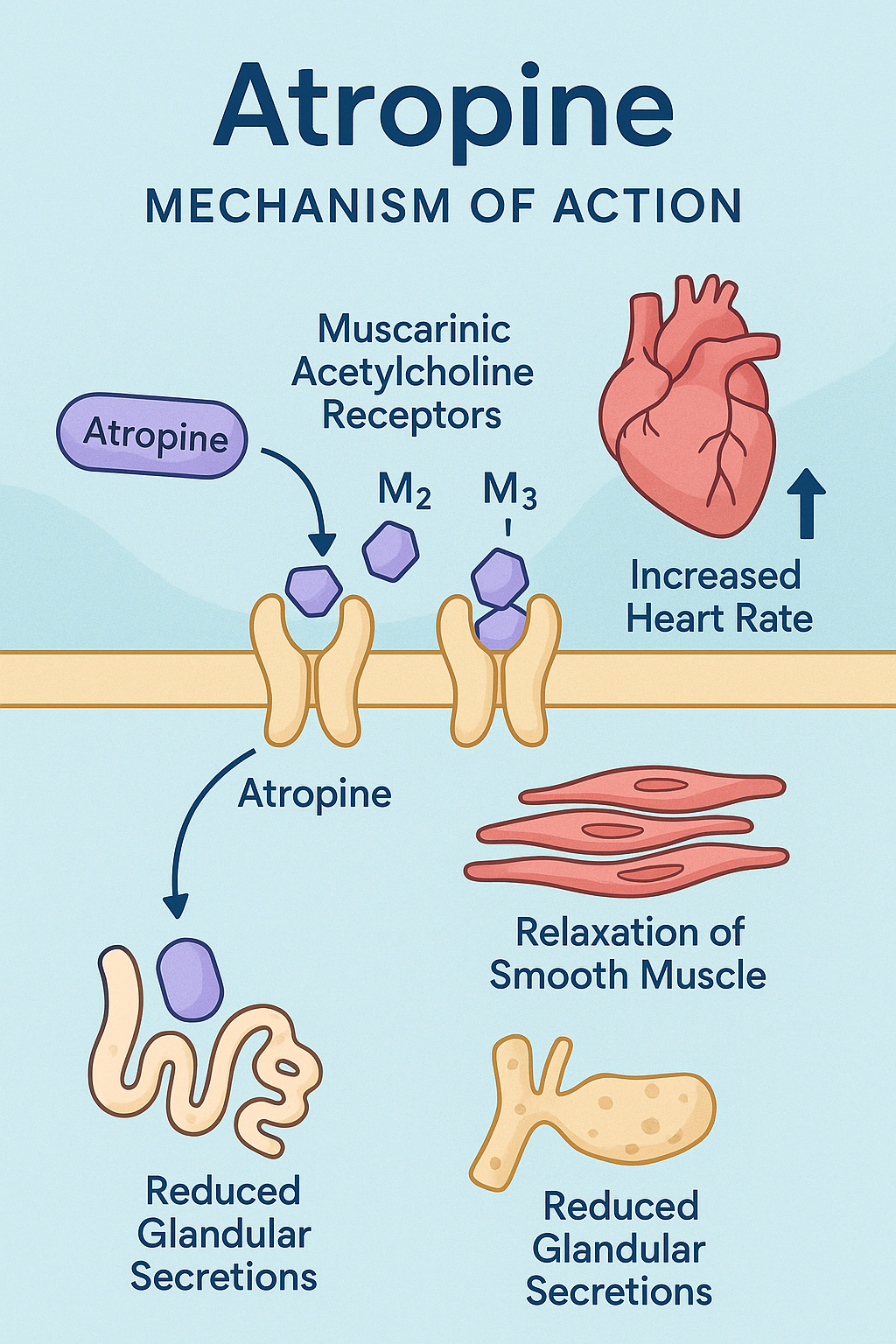
Atropine is a classic anticholinergic drug that works by competitively inhibiting muscarinic acetylcholine receptors (mAChRs). It is derived from the plant Atropa belladonna and has wide clinical use in bradycardia, organophosphate poisoning, pre-anesthetic medication, and pupil dilation.
Its importance spans autonomic pharmacology, emergency medicine, and toxicology, making it a high-yield topic for USMLE, NCLEX, GPAT, NEET-PG, and NAPLEX aspirants.
Mechanism of Action of Atropine: Step-by-Step
- Competitive antagonist at muscarinic receptors (M1–M5)
Atropine binds competitively and reversibly to all subtypes of muscarinic acetylcholine receptors (M1 to M5) without activating them. - Inhibits parasympathetic neurotransmission
By blocking acetylcholine (ACh) at these receptors, atropine effectively inhibits parasympathetic effects across various organs. - Organ-specific effects:
- Heart (M2): Inhibits vagal tone → increases heart rate
- Eyes (M3): Causes mydriasis (pupil dilation) and cycloplegia (loss of accommodation)
- GI tract & bladder (M3): Reduces motility and relieves spasms
- Respiratory (M3): Bronchodilation and reduction in secretions
- CNS (M1): Excitatory at high doses; can lead to delirium
- No effect on nicotinic receptors
It does not affect nicotinic receptors, so ganglionic and neuromuscular functions remain intact.
Pharmacokinetic Parameters of Atropine
| Parameter | Value |
|---|---|
| Bioavailability | High (oral/parenteral) |
| Onset of action | IV: 1–2 min, IM: 30 min |
| Duration of action | 4–6 hrs (ocular effect: 7–14 days) |
| Half-life | ~2–4 hours |
| Metabolism | Hepatic |
| Excretion | Renal |
| CNS penetration | Yes (lipophilic) |
Clinical Uses of Atropine
- Bradycardia (ACLS algorithm)
- Organophosphate or carbamate poisoning
- Pre-anesthetic to reduce secretions
- Ophthalmologic use (mydriasis and cycloplegia)
- Antispasmodic for GI and bladder disorders
- Antidote for muscarinic mushroom poisoning
- AV block and vagal overdrive conditions
Adverse Effects of Atropine
- Dry mouth
- Blurred vision
- Photophobia
- Tachycardia
- Constipation and urinary retention
- CNS excitation (delirium, hallucination in overdose)
- Hyperthermia (due to decreased sweating)
- Atropine poisoning: “Dry as a bone, red as a beet, blind as a bat, hot as a hare, mad as a hatter”
Comparative Analysis: Atropine vs Glycopyrrolate
| Feature | Atropine | Glycopyrrolate |
|---|---|---|
| CNS penetration | Yes (crosses BBB) | No (does not cross BBB) |
| Duration of action | Shorter | Longer |
| Use in bradycardia | Yes | Less preferred |
| Antisecretory use | Yes | Yes (especially in anesthesia) |
| Use in children | Caution (can cause hyperthermia) | Safer |
Practice MCQs
Q1. Atropine is an antagonist of:
a. Nicotinic receptors
b. Muscarinic receptors ✅
c. Dopamine receptors
d. GABA receptors
Q2. Which organ system effect is due to M2 blockade?
a. Pupil dilation
b. Bradycardia
c. Tachycardia ✅
d. Bronchoconstriction
Q3. Which of the following is NOT a typical effect of atropine?
a. Dry mouth
b. Miosis ✅
c. Tachycardia
d. Urinary retention
Q4. In organophosphate poisoning, atropine is used to counteract:
a. Nicotinic toxicity
b. Muscarinic overstimulation ✅
c. CNS depression
d. Enzyme inhibition
Q5. Atropine causes which ocular change?
a. Miosis
b. Diplopia
c. Mydriasis ✅
d. Conjunctivitis
Q6. What is the antidote for atropine overdose?
a. Naloxone
b. Physostigmine ✅
c. Flumazenil
d. Ativan
Q7. Atropine’s GI effects include:
a. Increased motility
b. Constipation ✅
c. Diarrhea
d. Ulceration
Q8. The mnemonic “Dry as a bone…” refers to toxicity of:
a. Epinephrine
b. Diazepam
c. Atropine ✅
d. Morphine
Q9. Atropine is contraindicated in:
a. Glaucoma ✅
b. AV block
c. Bradycardia
d. Asthma
Q10. Atropine blocks which neurotransmitter?
a. Noradrenaline
b. Serotonin
c. Acetylcholine ✅
d. Dopamine
FAQs
Q1: Does atropine affect sympathetic nervous system?
No. It blocks parasympathetic (muscarinic) activity only.
Q2: Can atropine be used in children?
Yes, but cautiously — especially due to risk of hyperthermia.
Q3: What’s the dose for bradycardia in ACLS?
0.5 mg IV every 3–5 minutes, max dose: 3 mg.
Q4: Does atropine increase or decrease secretions?
Decreases all secretions – saliva, bronchial, sweat.
Q5: Can atropine be used in asthma?
Rarely used, as better bronchodilators (like ipratropium) exist.
References
- KD Tripathi – Essentials of Medical Pharmacology
- Goodman & Gilman – The Pharmacological Basis of Therapeutics
- Sparsh Gupta – Review of Pharmacology
- NCBI: https://www.ncbi.nlm.nih.gov/books/NBK537221/

I am pursuing MBA in pharmaceutical management from NIPER Hyderabad with a strong academic record and proven success in national-level pharmacy entrance exams. I secured AIR 61 in NIPER 2024 (MS/M.Pharm) and AIR 27 in NIPER MBA, along with AIR 147 in GPAT 2024 and AIR 907 in GPAT 2023. I also achieved AIR 6 in AIIMS CRE-2025 for Drug Store Keeper and was selected as a Pharmacist (AIR 61) for ESIC. Additionally, I was the Runner-Up in Round 2 of the EY Case Study Competition.
At PharmacyFreak.com, I aim to guide future pharmacists through expert content, exam strategies, and insightful resources based on real experience and academic excellence.
Mail- harsh@pharmacyfreak.com