Table of Contents
Introduction
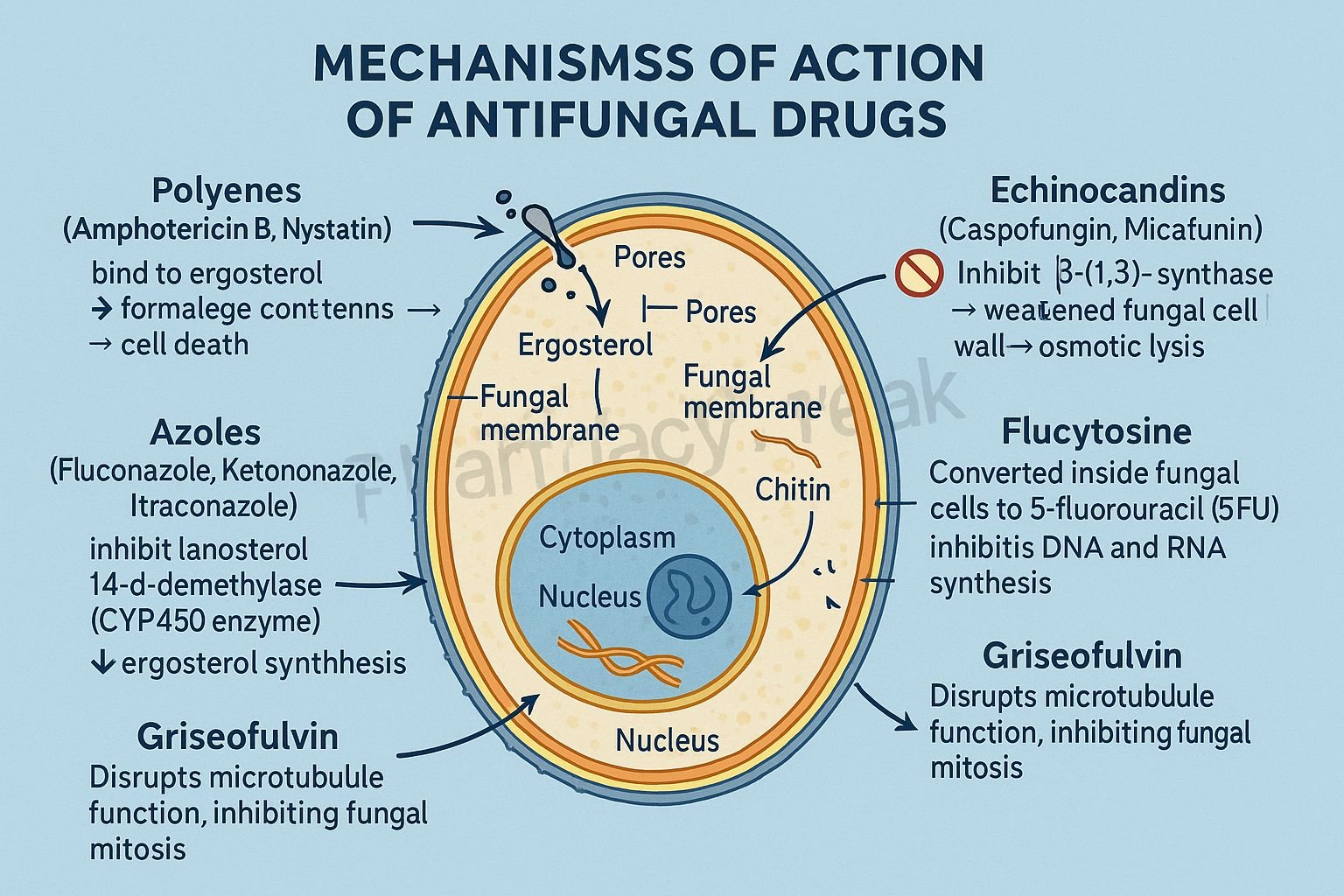
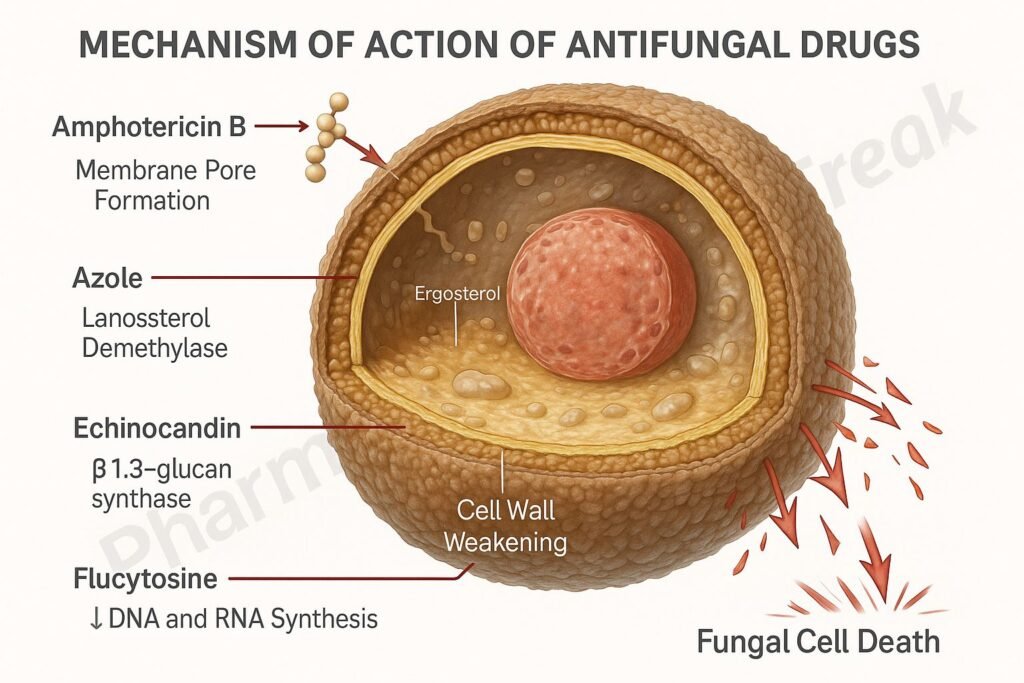
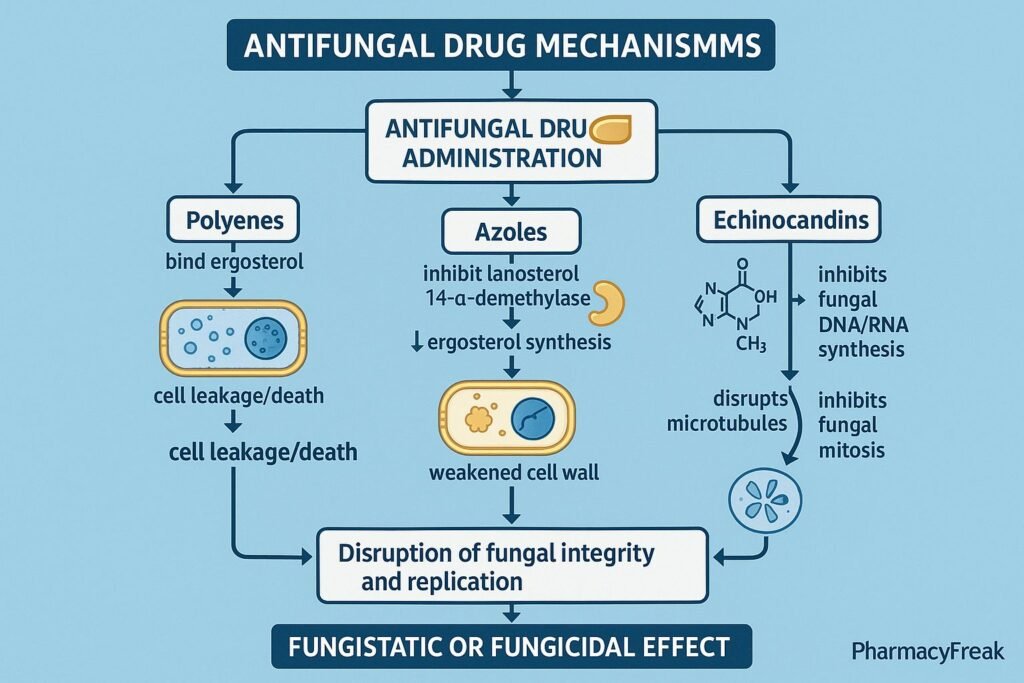
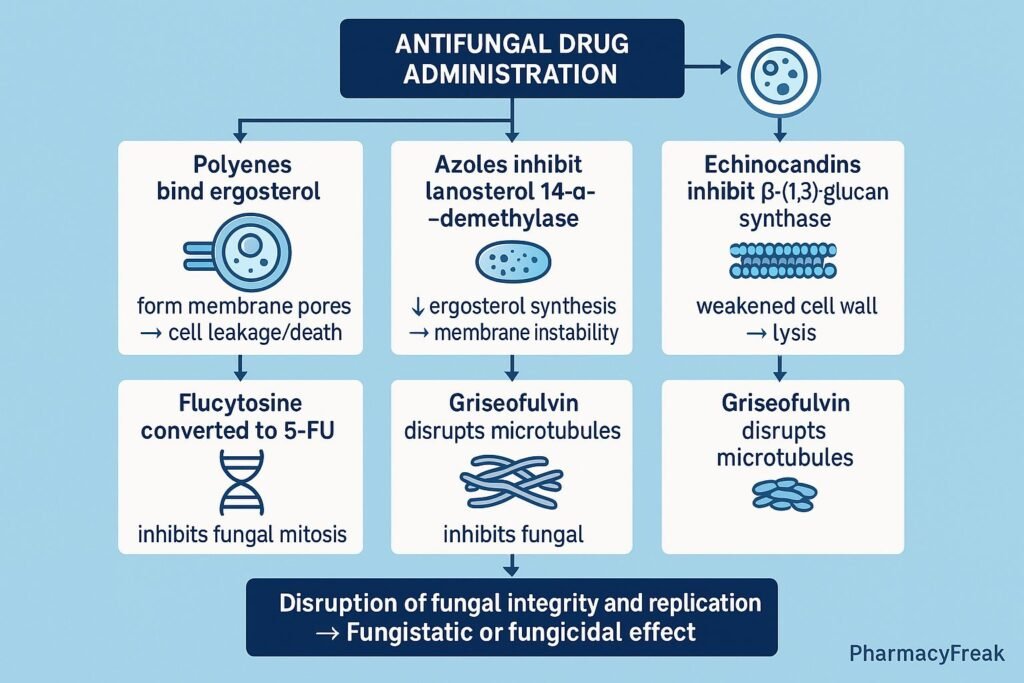
Antifungal drugs are pharmacological agents used to treat fungal infections (mycoses) affecting the skin, mucous membranes, or internal organs. Mechanism of Action of Antifungal Drugs involves disruption of fungal cell membrane integrity, cell wall synthesis, or nucleic acid function. Since fungal cells are eukaryotic and share many structural similarities with human cells, antifungal agents are designed to target fungal-specific components such as ergosterol in the cell membrane or β-glucan in the cell wall, minimizing human toxicity.
Mechanism of Action (Step-wise)
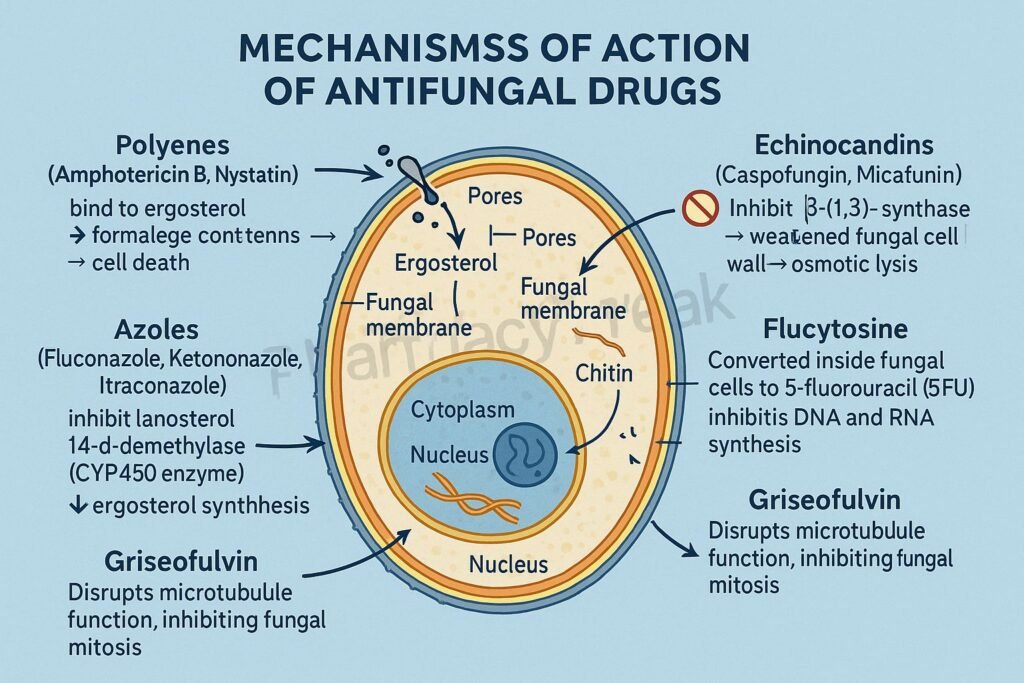
Antifungal drugs act via distinct biochemical targets depending on their drug class.
1. Inhibition of Ergosterol Synthesis (Azoles and Allylamines)
Ergosterol is a key component of fungal cell membranes, analogous to cholesterol in humans.
a) Azoles (Imidazoles and Triazoles)
- Mechanism: Inhibit the enzyme lanosterol 14-α-demethylase, a cytochrome P450–dependent enzyme that converts lanosterol to ergosterol.
- Effect:
- Depletion of ergosterol → altered membrane permeability → leakage of cellular contents → cell death.
- Examples: Ketoconazole, Fluconazole, Itraconazole, Voriconazole, Posaconazole.
b) Allylamines
- Mechanism: Inhibit squalene epoxidase, an enzyme earlier in the ergosterol synthesis pathway.
- Effect:
- Accumulation of toxic squalene and deficiency of ergosterol → disruption of cell membrane.
- Examples: Terbinafine, Naftifine.
2. Binding to Ergosterol (Polyenes)
- Mechanism: Polyene antifungals bind directly to ergosterol in the fungal membrane, creating pores or channels that cause leakage of intracellular ions and metabolites.
- Effect: Fungicidal action due to membrane disruption.
- Examples: Amphotericin B, Nystatin.
- Note: Amphotericin B is used systemically for life-threatening mycoses, while nystatin is topical for Candida infections.
3. Inhibition of Cell Wall Synthesis (Echinocandins)
- Mechanism: Inhibit β-(1,3)-D-glucan synthase, an enzyme essential for fungal cell wall synthesis.
- Effect: Weakening of the fungal cell wall → osmotic lysis → fungal death.
- Examples: Caspofungin, Micafungin, Anidulafungin.
- Note: Effective against Candida and Aspergillus species.
4. Disruption of Nucleic Acid Synthesis (Flucytosine)
- Mechanism: Flucytosine (5-FC) is converted inside fungal cells by cytosine deaminase to 5-fluorouracil (5-FU), which inhibits thymidylate synthase, blocking DNA and RNA synthesis.
- Effect: Inhibition of fungal cell replication and growth (fungistatic).
- Examples: Flucytosine (usually combined with Amphotericin B).
5. Inhibition of Microtubule Function (Griseofulvin)
- Mechanism: Interferes with fungal mitotic spindle microtubules, preventing mitosis.
- Effect: Fungistatic; inhibits growth of dermatophytes by binding to keratin in newly formed cells.
- Examples: Griseofulvin.
Summary Table of Antifungal Mechanisms
| Drug Class | Primary Target | Mechanism of Action | Examples |
|---|---|---|---|
| Polyenes | Cell membrane (ergosterol) | Binds ergosterol → pore formation → leakage | Amphotericin B, Nystatin |
| Azoles | Ergosterol synthesis | Inhibit lanosterol 14-α-demethylase | Fluconazole, Itraconazole |
| Allylamines | Ergosterol synthesis | Inhibit squalene epoxidase | Terbinafine, Naftifine |
| Echinocandins | Cell wall (β-glucan) | Inhibit β-(1,3)-D-glucan synthase | Caspofungin, Micafungin |
| Pyrimidine analogs | DNA/RNA synthesis | Converted to 5-FU → inhibits thymidylate synthase | Flucytosine |
| Other (Mitotic) | Microtubules | Interfere with spindle formation during mitosis | Griseofulvin |
MCQs
1. The primary target of azole antifungals is:
a) β-glucan synthase
b) Squalene epoxidase
c) Lanosterol 14-α-demethylase
d) Microtubules
Answer: c) Lanosterol 14-α-demethylase
2. Amphotericin B acts by:
a) Blocking DNA synthesis
b) Binding to ergosterol and forming membrane pores
c) Inhibiting β-glucan synthesis
d) Inhibiting squalene epoxidase
Answer: b) Binding to ergosterol and forming membrane pores
3. Echinocandins inhibit:
a) RNA polymerase
b) Glucan synthase
c) Thymidylate synthase
d) Ergosterol synthesis
Answer: b) Glucan synthase
4. Which antifungal blocks fungal mitosis?
a) Griseofulvin
b) Flucytosine
c) Amphotericin B
d) Terbinafine
Answer: a) Griseofulvin
5. Flucytosine is converted to 5-FU by:
a) Cytosine deaminase
b) Glucan synthase
c) Squalene epoxidase
d) Thymidylate reductase
Answer: a) Cytosine deaminase
6. The enzyme inhibited by terbinafine is:
a) Squalene epoxidase
b) Lanosterol demethylase
c) Glucan synthase
d) DNA polymerase
Answer: a) Squalene epoxidase
7. The major component of fungal cell membrane is:
a) Cholesterol
b) Ergosterol
c) Lanosterol
d) Peptidoglycan
Answer: b) Ergosterol
8. Amphotericin B is mainly used for:
a) Dermatophytosis
b) Systemic fungal infections
c) Candidiasis only
d) Tinea infections
Answer: b) Systemic fungal infections
9. A topical antifungal that binds ergosterol is:
a) Nystatin
b) Griseofulvin
c) Flucytosine
d) Caspofungin
Answer: a) Nystatin
10. Which antifungal inhibits thymidylate synthase?
a) Flucytosine
b) Terbinafine
c) Amphotericin B
d) Itraconazole
Answer: a) Flucytosine
FAQs
Q1. How do antifungal drugs differ from antibiotics?
Antifungals target eukaryotic fungal cells (ergosterol, β-glucan), whereas antibiotics target prokaryotic bacterial structures.
Q2. Why are fungal infections harder to treat than bacterial infections?
Because fungi are eukaryotes, sharing many biochemical pathways with human cells, limiting selective drug targets.
Q3. Which antifungal is safest for long-term use?
Fluconazole has excellent safety, bioavailability, and minimal hepatic toxicity.
Q4. Why is Amphotericin B called “amphoterrible”?
Due to dose-dependent nephrotoxicity and infusion-related reactions, despite its potent antifungal activity.
Q5. What is the mechanism of resistance to azoles?
Mutations in the lanosterol demethylase gene (ERG11) or increased efflux pump activity.
Q6. Can antifungals be used in immunocompromised patients?
Yes—Echinocandins and Amphotericin B are preferred for invasive fungal infections in immunocompromised hosts.
References
- Goodman & Gilman’s The Pharmacological Basis of Therapeutics
- Katzung’s Basic and Clinical Pharmacology
- Tripathi KD, Essentials of Medical Pharmacology
- Harrison’s Principles of Internal Medicine
Related Internal Links

I am pursuing MBA in pharmaceutical management from NIPER Hyderabad with a strong academic record and proven success in national-level pharmacy entrance exams. I secured AIR 61 in NIPER 2024 (MS/M.Pharm) and AIR 27 in NIPER MBA, along with AIR 147 in GPAT 2024 and AIR 907 in GPAT 2023. I also achieved AIR 6 in AIIMS CRE-2025 for Drug Store Keeper and was selected as a Pharmacist (AIR 61) for ESIC. Additionally, I was the Runner-Up in Round 2 of the EY Case Study Competition.
At PharmacyFreak.com, I aim to guide future pharmacists through expert content, exam strategies, and insightful resources based on real experience and academic excellence.
Mail- harsh@pharmacyfreak.com