Table of Contents
Introduction
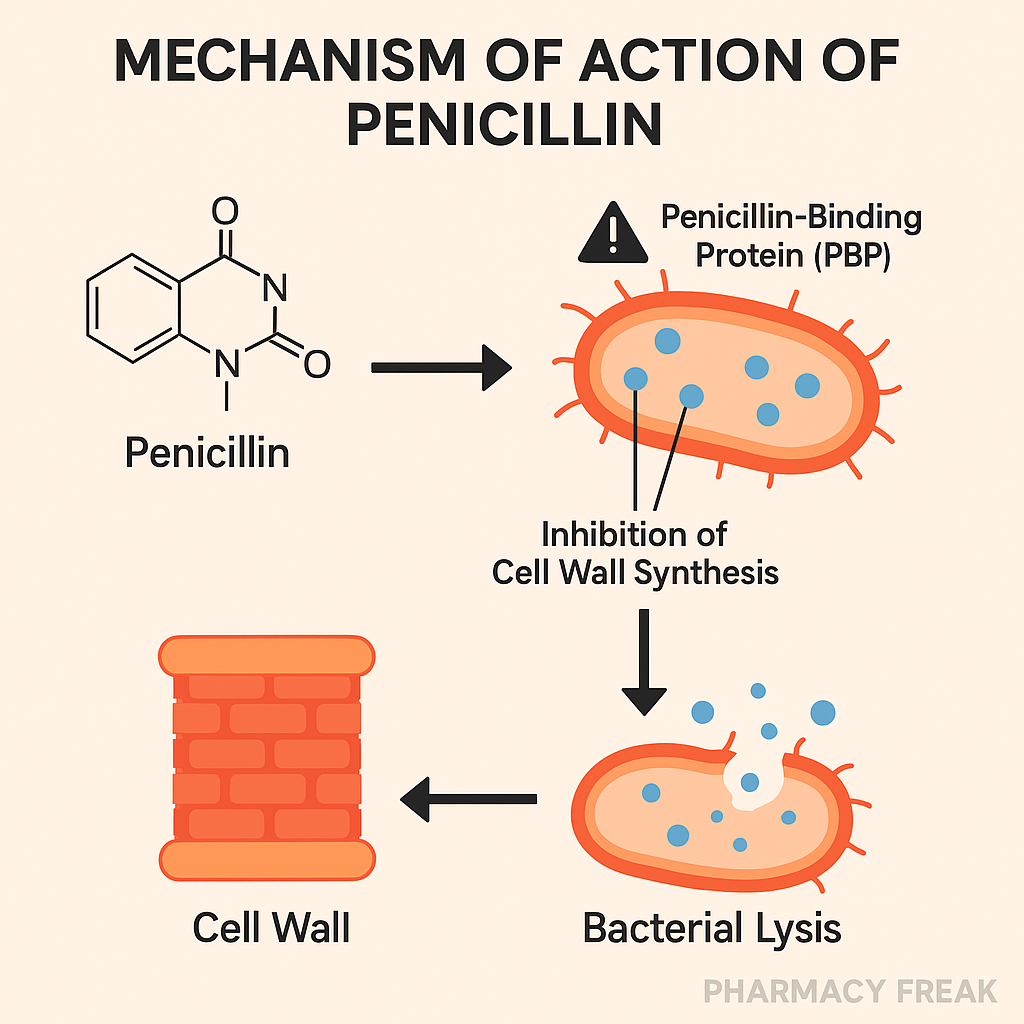
Penicillins are one of the oldest and most widely used classes of antibiotics, belonging to the β-lactam family. They’re highly effective against Gram-positive bacteria and some Gram-negatives, depending on the type. Their mechanism centers on inhibiting bacterial cell wall synthesis, which leads to bacterial lysis and death.
Penicillins remain a foundational topic for USMLE, NCLEX, GPAT, and NEET-PG aspirants — understanding their mechanism, resistance patterns, and clinical use is essential.
Stepwise Mechanism of Action of Penicillins
- Target: Penicillin-Binding Proteins (PBPs)
Penicillins bind to PBPs, enzymes involved in the final steps of peptidoglycan synthesis (e.g., transpeptidase). - Inhibition of transpeptidation
This action blocks the cross-linking of peptidoglycan chains, weakening the bacterial cell wall structure. - Disruption of cell wall integrity
The absence of cross-linking causes the cell wall to become unstable, especially in growing bacteria. - Autolysin activation
Penicillins may stimulate autolysins, bacterial enzymes that further degrade the cell wall. - Cell lysis and death
The cumulative effect leads to osmotic imbalance, cell swelling, and eventual bacterial cell lysis. Thus, penicillins are bactericidal.
Pharmacokinetic Parameters of Penicillins (e.g., Penicillin G)
| Parameter | Value |
|---|---|
| Bioavailability | Low (Penicillin G) – destroyed by acid |
| Half-life | 30 minutes to 1 hour |
| Metabolism | Minimal hepatic metabolism |
| Excretion | Renal (tubular secretion) |
| Protein binding | Moderate |
| Therapeutic range | Dose-dependent, varies by infection |
Clinical Uses of Penicillins
- Penicillin G: Syphilis, streptococcal infections, diphtheria
- Penicillin V: Pharyngitis, dental infections
- Ampicillin/Amoxicillin: UTIs, otitis media, sinusitis, H. pylori
- Cloxacillin/Oxacillin: MSSA skin infections
- Piperacillin-Tazobactam: Pseudomonas, hospital-acquired infections
Adverse Effects of Penicillins
- Hypersensitivity reactions (rash, urticaria, anaphylaxis)
- GI upset (nausea, diarrhea)
- Superinfections (e.g., C. difficile)
- Hematologic effects (neutropenia, eosinophilia)
- Seizures (high doses, renal failure)
- Electrolyte disturbances (especially IV forms)
Comparative Analysis: Penicillin G vs Amoxicillin
| Feature | Penicillin G | Amoxicillin |
|---|---|---|
| Acid stability | Destroyed in acid | Acid-stable (oral use) |
| Spectrum | Narrow (mostly Gram+) | Broad (Gram+ and Gram−) |
| Use in syphilis | First-line | Not used |
| Oral bioavailability | Poor | Excellent |
Practice MCQs
Q1. What is the primary target of penicillins?
a. DNA gyrase
b. Transpeptidase enzyme ✅
c. Ribosomal 30S subunit
d. RNA polymerase
Q2. Penicillins act by:
a. Inhibiting protein synthesis
b. Inhibiting DNA replication
c. Disrupting folic acid pathway
d. Inhibiting cell wall synthesis ✅
Q3. Penicillins are:
a. Bacteriostatic
b. Bactericidal ✅
c. Antifungal
d. Antiviral
Q4. Which side effect is most common with penicillins?
a. Liver failure
b. Seizure
c. Hypersensitivity ✅
d. Hearing loss
Q5. Autolysins contribute to:
a. Resistance
b. Penicillin metabolism
c. Cell lysis ✅
d. Enzyme activation
Q6. Which penicillin is effective against Pseudomonas?
a. Penicillin V
b. Amoxicillin
c. Piperacillin ✅
d. Cloxacillin
Q7. What is the mechanism of resistance to penicillin in MRSA?
a. β-lactamase
b. Altered PBPs (PBP2a) ✅
c. Efflux pumps
d. Porin mutations
Q8. How is penicillin primarily eliminated?
a. Liver
b. Lungs
c. Kidneys ✅
d. Skin
Q9. Which of the following is β-lactamase-resistant?
a. Penicillin G
b. Amoxicillin
c. Cloxacillin ✅
d. Ampicillin
Q10. Why is penicillin ineffective against Mycoplasma?
a. Drug resistance
b. Rapid metabolism
c. No cell wall ✅
d. Efflux pump
FAQs
Q1: Are penicillins effective against MRSA?
No, MRSA produces altered PBPs and is resistant to all β-lactams except ceftaroline.
Q2: Can penicillins cross the BBB?
Only in meningitis, when the BBB is inflamed.
Q3: Are penicillins safe in pregnancy?
Yes, they are generally safe and commonly used.
Q4: What is the role of β-lactamase inhibitors?
They inhibit β-lactamase enzymes, extending penicillin’s spectrum.
Q5: What if the patient is allergic to penicillin?
Use alternatives like macrolides or cephalosporins (with caution).
References
- KD Tripathi – Essentials of Medical Pharmacology
- Goodman & Gilman – The Pharmacological Basis of Therapeutics
- Sparsh Gupta – Review of Pharmacology
- NCBI: https://www.ncbi.nlm.nih.gov/books/NBK8160/

I am pursuing MBA in pharmaceutical management from NIPER Hyderabad with a strong academic record and proven success in national-level pharmacy entrance exams. I secured AIR 61 in NIPER 2024 (MS/M.Pharm) and AIR 27 in NIPER MBA, along with AIR 147 in GPAT 2024 and AIR 907 in GPAT 2023. I also achieved AIR 6 in AIIMS CRE-2025 for Drug Store Keeper and was selected as a Pharmacist (AIR 61) for ESIC. Additionally, I was the Runner-Up in Round 2 of the EY Case Study Competition.
At PharmacyFreak.com, I aim to guide future pharmacists through expert content, exam strategies, and insightful resources based on real experience and academic excellence.
Mail- harsh@pharmacyfreak.com