Table of Contents
Introduction
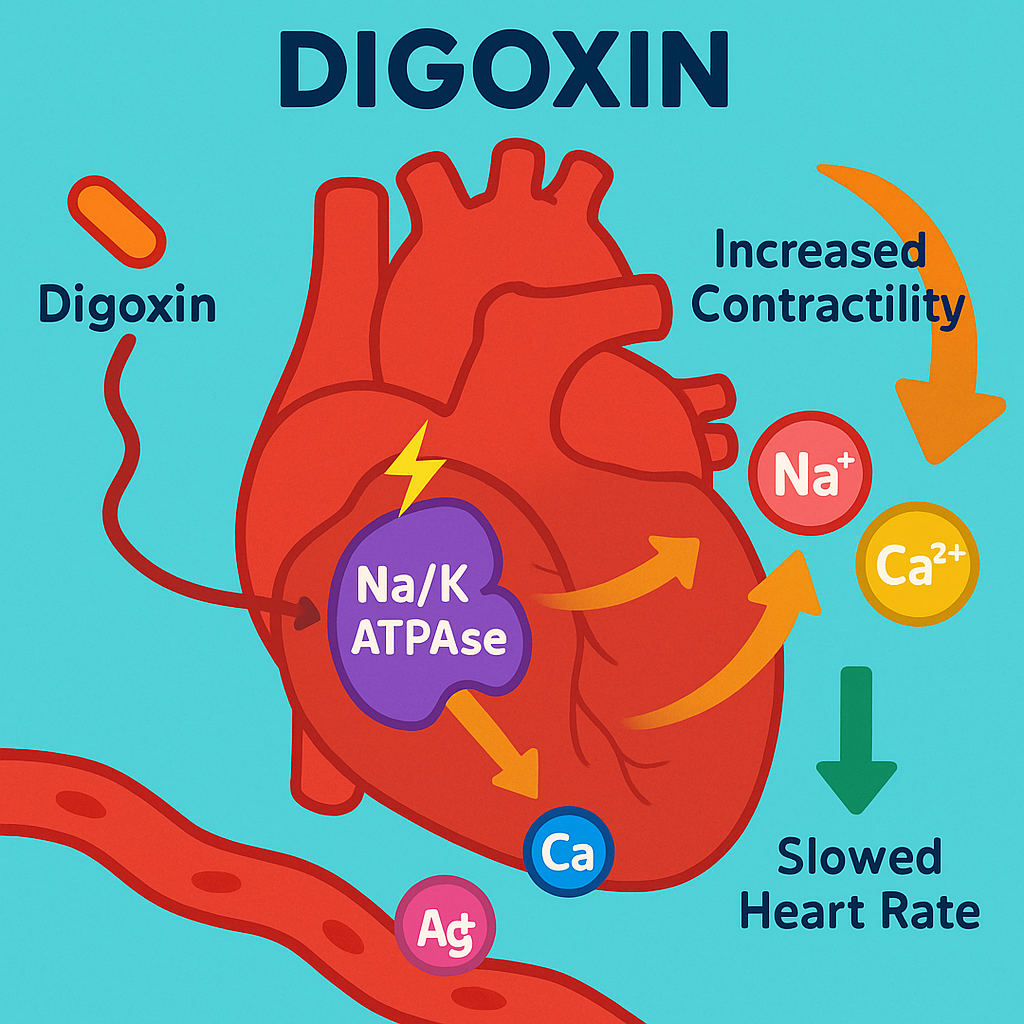
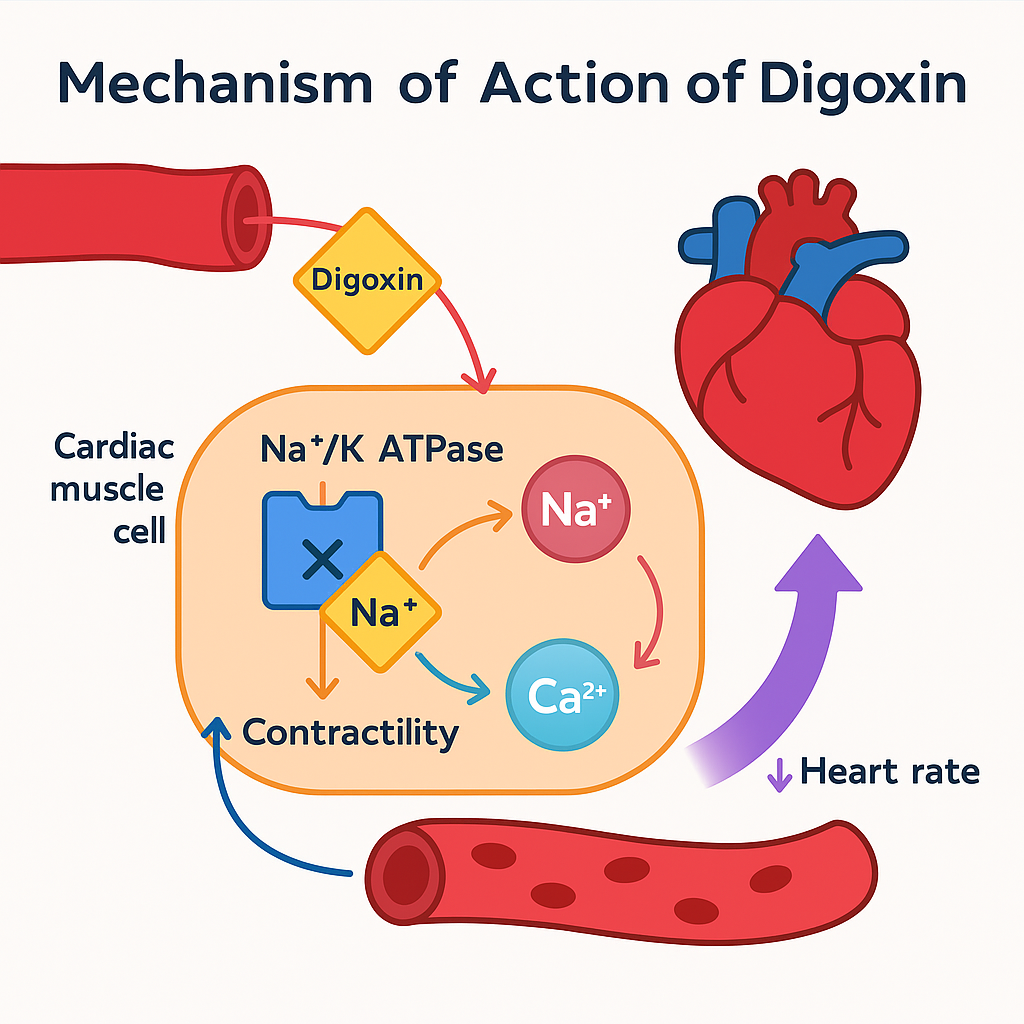
Digoxin is a well-known cardiac glycoside used in the treatment of heart failure and atrial fibrillation. Derived from Digitalis lanata, it has both positive inotropic and negative chronotropic effects. Its mechanism involves inhibition of the Na⁺/K⁺-ATPase pump, which indirectly increases intracellular calcium, enhancing myocardial contractility.
Digoxin’s unique pharmacology and toxicity profile make it a frequently tested drug in USMLE, NCLEX, GPAT, NEET-PG, and NAPLEX.
Mechanism of Action of Digoxin: Step-by-Step
- Inhibits Na⁺/K⁺-ATPase pump
Digoxin binds to and inhibits the Na⁺/K⁺-ATPase pump on cardiac cell membranes. - ↑ Intracellular Na⁺ concentration
Inhibition leads to a rise in intracellular sodium, which reduces the activity of the Na⁺/Ca²⁺ exchanger (NCX). - ↓ Na⁺/Ca²⁺ exchange → ↑ Intracellular Ca²⁺
With less sodium exchanged out, less calcium is pumped out of the cell, resulting in increased intracellular calcium. - Enhanced calcium availability in sarcoplasmic reticulum
This increase leads to greater calcium release during systole, enhancing myocardial contraction. - Increased cardiac contractility (positive inotropic effect)
Resulting in improved cardiac output, especially in heart failure patients. - Vagal stimulation
Digoxin also enhances parasympathetic (vagal) tone, leading to slowed AV nodal conduction — useful in atrial fibrillation.
Pharmacokinetic Parameters of Digoxin
| Parameter | Value |
|---|---|
| Bioavailability | 60–80% (oral) |
| Half-life | ~36–48 hours (longer in renal failure) |
| Protein binding | 20–30% |
| Volume of distribution | Large (~7 L/kg) |
| Metabolism | Minimal (liver) |
| Excretion | Renal (mostly unchanged) |
| Therapeutic index | Narrow |
Clinical Uses of Digoxin
- Chronic heart failure (systolic dysfunction)
- Rate control in atrial fibrillation
- Supraventricular tachycardia (limited use)
- Atrial flutter (with AV block)
- Cardiac output improvement in selected HF patients
Adverse Effects of Digoxin
- Arrhythmias (bradycardia, AV block, ventricular ectopics)
- GI upset (nausea, vomiting, diarrhea)
- Visual disturbances (yellow vision, halos)
- Fatigue, dizziness, confusion
- Electrolyte disturbances (hypokalemia ↑ toxicity)
- Gynecomastia (rare)
Comparative Analysis: Digoxin vs Dobutamine
| Feature | Digoxin | Dobutamine |
|---|---|---|
| Mechanism | Na⁺/K⁺-ATPase inhibition | β1-adrenergic agonist |
| Onset of action | Slow | Rapid |
| Route | Oral and IV | IV only |
| Half-life | Long (~36–48 hrs) | Short (~2 minutes) |
| Use in acute HF | Not preferred | Preferred |
| Toxicity risk | High (narrow TI) | Low |
Practice MCQs
Q1. Digoxin increases cardiac contractility by:
a. Inhibiting calcium channels
b. Stimulating β1 receptors
c. Inhibiting Na⁺/K⁺-ATPase ✅
d. Enhancing Na⁺ influx
Q2. What is the effect of digoxin on AV node?
a. Stimulation
b. Suppression ✅
c. No effect
d. Constriction
Q3. Which ion’s change leads to increased intracellular Ca²⁺ due to digoxin?
a. Na⁺ ✅
b. K⁺
c. Mg²⁺
d. Cl⁻
Q4. Digoxin toxicity is enhanced by:
a. Hyperkalemia
b. Hypokalemia ✅
c. Hypernatremia
d. Hypomagnesemia
Q5. Which of the following is a typical visual symptom of digoxin toxicity?
a. Green vision
b. Blurred vision
c. Blue vision
d. Yellow vision ✅
Q6. Which arrhythmia is most common with digoxin toxicity?
a. Ventricular fibrillation
b. AV block ✅
c. Torsades
d. Atrial flutter
Q7. Digoxin has a narrow:
a. Volume of distribution
b. Therapeutic index ✅
c. Half-life
d. Bioavailability
Q8. What is used to treat severe digoxin toxicity?
a. Sodium bicarbonate
b. Digoxin-specific antibody (Fab) ✅
c. Atropine
d. Lidocaine
Q9. What is the effect of digoxin on vagal tone?
a. None
b. Decreases
c. Increases ✅
d. Inhibits
Q10. Which of the following is a known interaction of digoxin?
a. Loop diuretics (↑ toxicity) ✅
b. ACE inhibitors (↓ effect)
c. Antacids (↑ absorption)
d. NSAIDs (↓ half-life)
FAQs
Q1: How does digoxin help in heart failure?
By increasing myocardial contractility and improving cardiac output.
Q2: Why is digoxin useful in atrial fibrillation?
It slows AV nodal conduction via vagal stimulation, controlling ventricular rate.
Q3: Is digoxin safe in renal failure?
Use with caution. It is renally excreted and requires dose adjustment.
Q4: What are signs of digoxin toxicity?
Nausea, bradycardia, arrhythmia, and yellow vision are classic signs.
Q5: What is the antidote for digoxin toxicity?
Digoxin-specific antibody fragments (Digibind or DigiFab).
References
- KD Tripathi – Essentials of Medical Pharmacology
- Goodman & Gilman – The Pharmacological Basis of Therapeutics
- Sparsh Gupta – Review of Pharmacology
- NCBI: https://www.ncbi.nlm.nih.gov/books/NBK538271/

I am pursuing MBA in pharmaceutical management from NIPER Hyderabad with a strong academic record and proven success in national-level pharmacy entrance exams. I secured AIR 61 in NIPER 2024 (MS/M.Pharm) and AIR 27 in NIPER MBA, along with AIR 147 in GPAT 2024 and AIR 907 in GPAT 2023. I also achieved AIR 6 in AIIMS CRE-2025 for Drug Store Keeper and was selected as a Pharmacist (AIR 61) for ESIC. Additionally, I was the Runner-Up in Round 2 of the EY Case Study Competition.
At PharmacyFreak.com, I aim to guide future pharmacists through expert content, exam strategies, and insightful resources based on real experience and academic excellence.
Mail- harsh@pharmacyfreak.com