Table of Contents
Introduction
Beta-blockers are a widely used class of drugs in cardiovascular medicine. They block the effects of catecholamines, particularly norepinephrine and epinephrine, on beta-adrenergic receptors. This results in decreased heart rate, myocardial contractility, and renin release, leading to lower blood pressure and decreased myocardial oxygen demand.
Common beta-blockers include:
- Metoprolol
- Atenolol
- Propranolol
- Carvedilol
- Nebivolol
Beta-blockers are used in managing hypertension, angina, arrhythmias, heart failure, and after myocardial infarction. They are frequently tested in exams like USMLE, NCLEX, NAPLEX, GPAT, and NEET-PG.
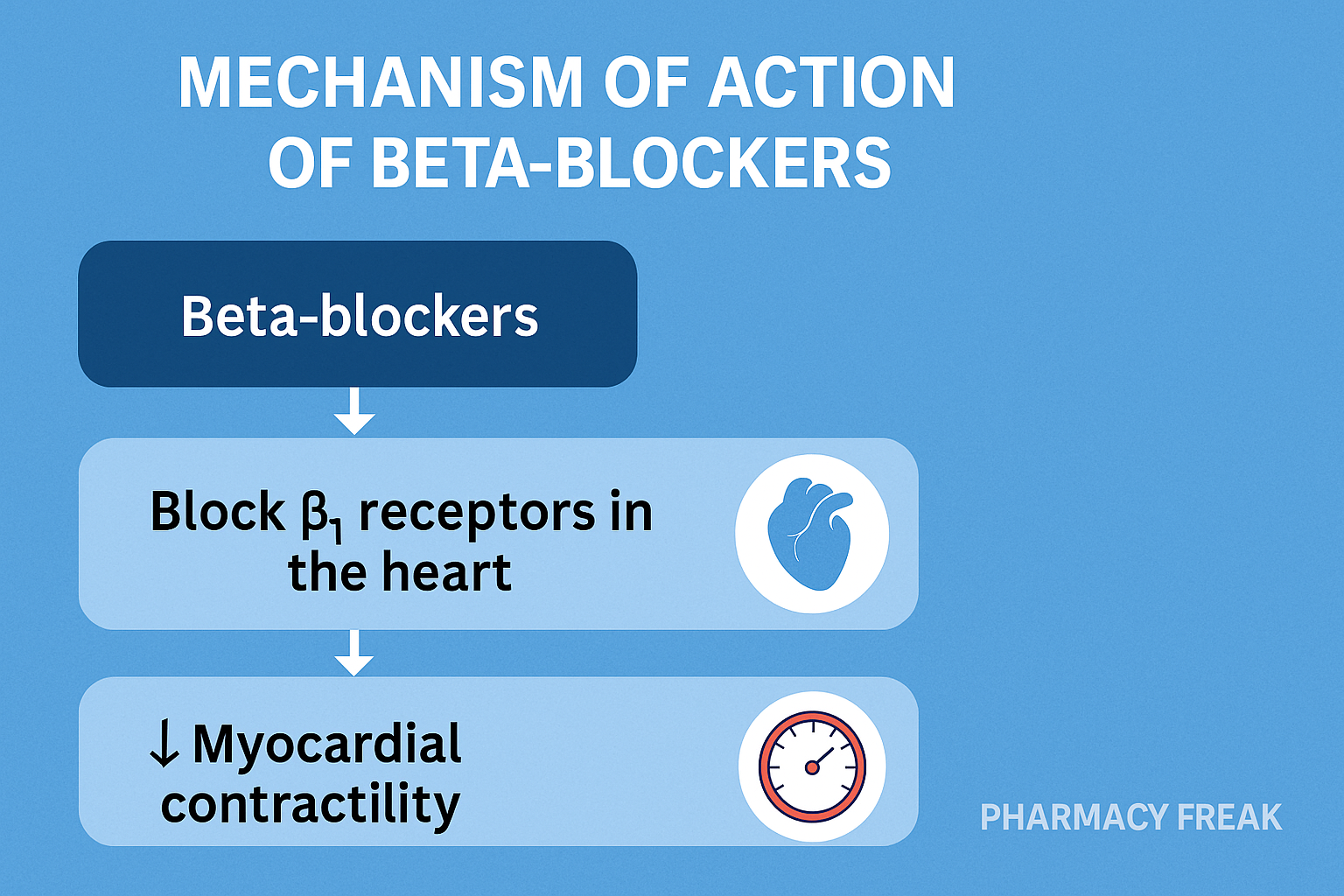
Stepwise Mechanism of Action of Beta-Blockers
- Competitive antagonism of beta-adrenergic receptors:
Beta-blockers bind to beta-1 and/or beta-2 adrenergic receptors, preventing catecholamines from activating them. - Beta-1 receptor blockade:
Primarily found in the heart and juxtaglomerular cells, beta-1 blockade results in:- Decreased heart rate (negative chronotropic effect)
- Reduced myocardial contractility (negative inotropic effect)
- Decreased renin release from the kidneys
- Beta-2 receptor blockade:
Located mainly in bronchial and vascular smooth muscle, beta-2 blockade may cause bronchoconstriction and vasoconstriction. - Net effects:
- Reduced cardiac output and blood pressure
- Reduced myocardial oxygen demand
- Inhibition of renin-angiotensin-aldosterone system (RAAS) activation





Pharmacokinetic Parameters of Beta-Blockers
| Parameter | General Values (vary by drug) |
|---|---|
| Bioavailability | Variable (15–90%) |
| Half-life | 3–12 hours (varies widely) |
| Protein Binding | 5–98% (drug-dependent) |
| Metabolism | Hepatic (most) or renal (atenolol) |
| Excretion | Renal and hepatic |
Clinical Uses of Beta-Blockers
- Hypertension
- Angina pectoris
- Heart failure with reduced ejection fraction
- Arrhythmias (supraventricular tachycardia, atrial fibrillation)
- Post-myocardial infarction
- Migraine prophylaxis
- Hyperthyroidism symptoms management
Adverse Effects of Beta-Blockers
- Bradycardia
- Fatigue and dizziness
- Bronchospasm (especially non-selective beta-blockers)
- Cold extremities
- Erectile dysfunction
- Masking of hypoglycemia symptoms
- Depression (rare)
Comparative Analysis: Selective vs Non-Selective Beta-Blockers
| Feature | Selective (e.g., Metoprolol) | Non-selective (e.g., Propranolol) |
|---|---|---|
| Beta-1 receptor affinity | High | Low |
| Beta-2 receptor affinity | Low | High |
| Bronchospasm risk | Lower | Higher |
| Use in asthma/COPD | Preferred | Usually avoided |
| CNS side effects | Less | More (lipophilic drugs) |
Practice MCQs
Q1. Beta-blockers primarily block which receptors?
a. Alpha-1 adrenergic
b. Beta-adrenergic ✅
c. Muscarinic
d. Dopaminergic
Q2. Which beta receptor subtype is mainly responsible for cardiac effects?
a. Beta-1 ✅
b. Beta-2
c. Beta-3
d. Alpha-2
Q3. Non-selective beta-blockers block which receptors?
a. Only Beta-1
b. Only Beta-2
c. Beta-1 and Beta-2 ✅
d. Alpha-1 and Beta-1
Q4. Which of the following is a contraindication for non-selective beta-blockers?
a. Hypertension
b. Asthma ✅
c. Diabetes
d. Hyperthyroidism
Q5. Beta-blockers reduce blood pressure by:
a. Increasing cardiac output
b. Blocking vasopressin
c. Reducing heart rate and renin release ✅
d. Stimulating aldosterone
Q6. Which beta-blocker is cardioselective?
a. Propranolol
b. Metoprolol ✅
c. Nadolol
d. Labetalol
Q7. Which side effect is common to beta-blockers?
a. Tachycardia
b. Bronchodilation
c. Bradycardia ✅
d. Hyperglycemia
Q8. Beta-blockers can mask symptoms of:
a. Hypoglycemia ✅
b. Hyperthyroidism
c. Hypertension
d. Hypercalcemia
Q9. Which beta-blocker also has alpha-blocking activity?
a. Atenolol
b. Carvedilol ✅
c. Metoprolol
d. Propranolol
Q10. Beta-blockers are useful in treating all EXCEPT:
a. Hypertension
b. Asthma ✅
c. Angina
d. Post-MI
FAQs
Q1: Can beta-blockers be used in asthma?
Non-selective beta-blockers are contraindicated due to risk of bronchospasm. Cardioselective beta-blockers may be used cautiously.
Q2: What are the common side effects of beta-blockers?
Bradycardia, fatigue, dizziness, cold extremities, and erectile dysfunction.
Q3: Can beta-blockers cause hypoglycemia?
They do not cause hypoglycemia but can mask its adrenergic symptoms.
Q4: How do beta-blockers help after a myocardial infarction?
By reducing myocardial oxygen demand and preventing arrhythmias.
References
- KD Tripathi – Essentials of Medical Pharmacology
- Goodman & Gilman – The Pharmacological Basis of Therapeutics
- Sparsh Gupta – Review of Pharmacology
- AHA Guidelines
- NCBI: https://www.ncbi.nlm.nih.gov/books/NBK459217/

I am pursuing MBA in pharmaceutical management from NIPER Hyderabad with a strong academic record and proven success in national-level pharmacy entrance exams. I secured AIR 61 in NIPER 2024 (MS/M.Pharm) and AIR 27 in NIPER MBA, along with AIR 147 in GPAT 2024 and AIR 907 in GPAT 2023. I also achieved AIR 6 in AIIMS CRE-2025 for Drug Store Keeper and was selected as a Pharmacist (AIR 61) for ESIC. Additionally, I was the Runner-Up in Round 2 of the EY Case Study Competition.
At PharmacyFreak.com, I aim to guide future pharmacists through expert content, exam strategies, and insightful resources based on real experience and academic excellence.
Mail- harsh@pharmacyfreak.com