Table of Contents
Introduction
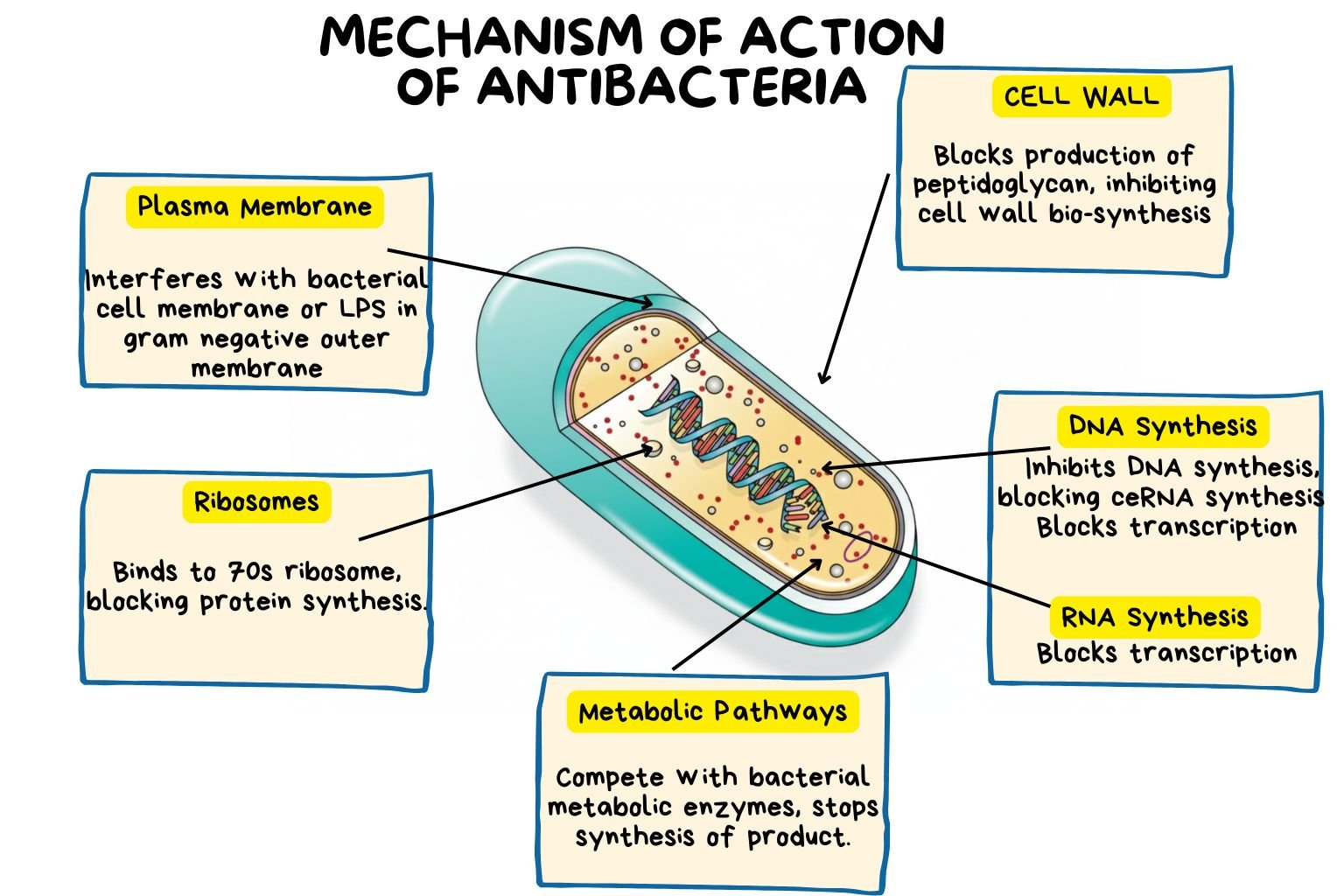
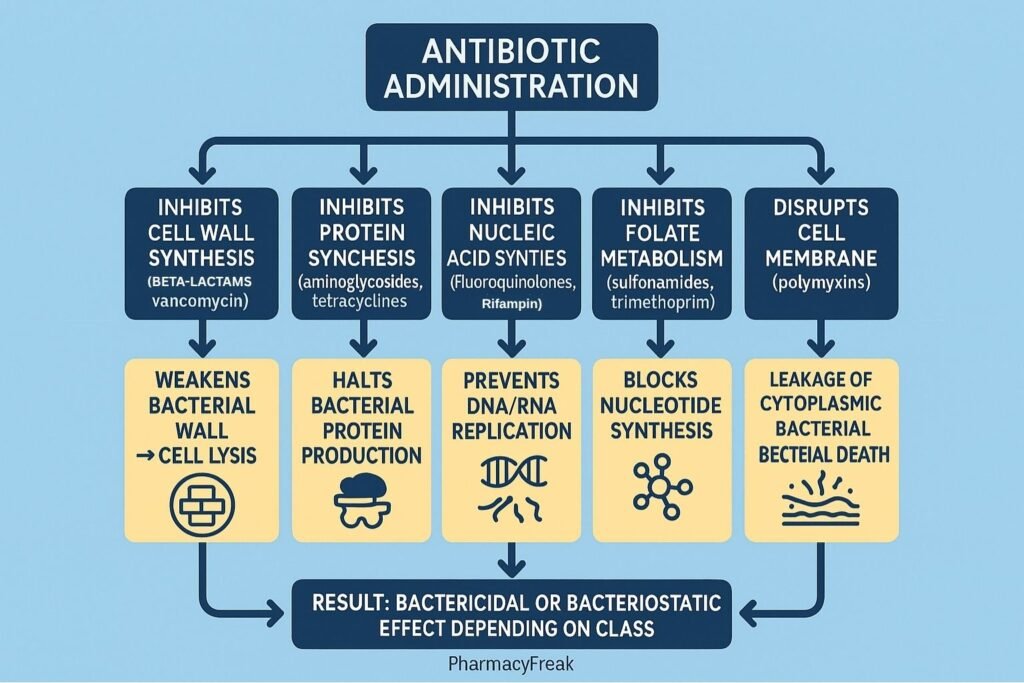
Antibacterial drugs, commonly called antibiotics, are agents that kill or inhibit the growth of bacteria by targeting essential cellular processes unique to prokaryotic organisms. Mechanism of Action of Antibacterial Drugs revolves around interference with cell wall synthesis, protein synthesis, nucleic acid replication, metabolic pathways, or cell membrane integrity. Understanding these mechanisms is essential for rational antibiotic use, prevention of resistance, and development of new antimicrobial agents.
Mechanism of Action (Step-wise)
Antibacterial drugs act through five major mechanisms, depending on their class and bacterial target.
1. Inhibition of Cell Wall Synthesis
- These drugs block the formation of the peptidoglycan layer, which provides bacterial cell wall strength.
- Mechanism: Interfere with transpeptidation or transglycosylation during peptidoglycan synthesis.
- Result: Weak cell wall → osmotic lysis → bacterial death.
- Examples:
- β-lactams (Penicillins, Cephalosporins, Carbapenems, Monobactams) — inhibit penicillin-binding proteins (PBPs).
- Glycopeptides (Vancomycin, Teicoplanin) — block peptidoglycan cross-linking by binding D-Ala-D-Ala terminus.
2. Inhibition of Protein Synthesis
- These drugs act on bacterial ribosomes (70S type) but not human ribosomes (80S), ensuring selective toxicity.
- Mechanism: Bind to 30S or 50S ribosomal subunits, interfering with translation.
- Examples:
- 30S inhibitors: Aminoglycosides (Amikacin, Gentamicin), Tetracyclines.
- 50S inhibitors: Macrolides (Erythromycin, Azithromycin), Chloramphenicol, Clindamycin, Linezolid.
- Result: Disruption of protein synthesis → inhibition of bacterial growth (bacteriostatic) or cell death (bactericidal).
3. Inhibition of Nucleic Acid Synthesis
- These agents interfere with DNA replication or RNA transcription.
- Mechanisms:
- Block DNA gyrase/topoisomerase II (prevents DNA unwinding).
- Inhibit RNA polymerase (prevents mRNA synthesis).
- Examples:
- Fluoroquinolones (Ciprofloxacin, Levofloxacin) — inhibit DNA gyrase and topoisomerase IV.
- Rifamycins (Rifampicin) — inhibit bacterial RNA polymerase.
- Metronidazole — forms toxic intermediates that damage DNA (anaerobes only).
- Result: Disruption of nucleic acid integrity → cell death.
4. Inhibition of Metabolic Pathways (Antimetabolites)
- These antibiotics act as structural analogs of bacterial metabolites, inhibiting key enzymes in folate synthesis.
- Mechanism:
- Sulfonamides inhibit dihydropteroate synthase.
- Trimethoprim inhibits dihydrofolate reductase.
- Result: Reduced synthesis of tetrahydrofolic acid → inhibition of DNA, RNA, and protein synthesis.
- Example combination: Cotrimoxazole (Trimethoprim + Sulfamethoxazole) — synergistic, sequential blockade.
5. Disruption of Cell Membrane Integrity
- These drugs directly damage the bacterial cell membrane, increasing permeability and causing leakage of essential intracellular components.
- Examples:
- Polymyxins (Polymyxin B, Colistin): Bind to lipopolysaccharides (LPS) and phospholipids in Gram-negative bacteria.
- Daptomycin: Inserts into Gram-positive membranes causing depolarization.
- Result: Membrane damage → loss of ions and metabolites → bacterial death.
Summary Table of Antibacterial Mechanisms
| Mechanism | Site of Action | Drug Class Examples | Effect |
|---|---|---|---|
| Inhibit cell wall synthesis | Peptidoglycan layer | β-lactams, Vancomycin | Bactericidal |
| Inhibit protein synthesis (30S/50S) | Ribosome | Aminoglycosides, Tetracyclines, Macrolides | Mostly bacteriostatic |
| Inhibit nucleic acid synthesis | DNA/RNA enzymes | Fluoroquinolones, Rifampicin, Metronidazole | Bactericidal |
| Inhibit folate synthesis | Metabolic enzymes | Sulfonamides, Trimethoprim | Bacteriostatic |
| Damage cell membrane | Cytoplasmic membrane | Polymyxins, Daptomycin | Bactericidal |
MCQs
1. Which of the following inhibits bacterial cell wall synthesis?
a) Ciprofloxacin
b) Penicillin
c) Erythromycin
d) Tetracycline
Answer: b) Penicillin
2. Aminoglycosides act on which ribosomal subunit?
a) 30S
b) 50S
c) 70S
d) 80S
Answer: a) 30S
3. Sulfonamides inhibit which enzyme?
a) DNA gyrase
b) Dihydropteroate synthase
c) RNA polymerase
d) Topoisomerase IV
Answer: b) Dihydropteroate synthase
4. Which drug inhibits bacterial RNA polymerase?
a) Rifampicin
b) Levofloxacin
c) Gentamicin
d) Chloramphenicol
Answer: a) Rifampicin
5. Fluoroquinolones inhibit:
a) Cell wall synthesis
b) DNA gyrase and topoisomerase IV
c) Folate synthesis
d) Protein synthesis
Answer: b) DNA gyrase and topoisomerase IV
6. Which of the following disrupts bacterial cell membranes?
a) Vancomycin
b) Daptomycin
c) Clindamycin
d) Trimethoprim
Answer: b) Daptomycin
7. Trimethoprim acts by:
a) Inhibiting DNA replication
b) Inhibiting dihydrofolate reductase
c) Blocking ribosomal activity
d) Disrupting the cell membrane
Answer: b) Inhibiting dihydrofolate reductase
8. Which mechanism is responsible for bactericidal activity of β-lactams?
a) Protein synthesis inhibition
b) Peptidoglycan cross-link inhibition
c) RNA polymerase inhibition
d) DNA synthesis inhibition
Answer: b) Peptidoglycan cross-link inhibition
9. The bacterial ribosome targeted by antibiotics is:
a) 70S
b) 80S
c) 60S
d) 50S
Answer: a) 70S
10. Metronidazole acts by:
a) Inhibiting folate synthesis
b) Generating free radicals that damage DNA
c) Blocking 30S ribosome
d) Inhibiting H+ secretion
Answer: b) Generating free radicals that damage DNA
FAQs
Q1. How do antibiotics differ from antiseptics?
Antibiotics are used internally to target bacterial processes, while antiseptics are used externally to kill or inhibit microorganisms on surfaces or skin.
Q2. What is the difference between bactericidal and bacteriostatic drugs?
Bactericidal drugs kill bacteria, whereas bacteriostatic drugs inhibit growth and rely on host immunity for bacterial clearance.
Q3. Why don’t antibiotics affect human cells?
They target structures (e.g., peptidoglycan cell wall, 70S ribosomes) unique to bacteria and absent in human cells.
Q4. Can antibiotics be combined?
Yes, combination therapy can be synergistic (e.g., β-lactam + aminoglycoside) but must be rational to avoid antagonism.
Q5. How does antibiotic resistance develop?
Through mutations, efflux pumps, enzyme production (e.g., β-lactamases), or altered drug targets.
Q6. Which antibiotics act fastest?
Bactericidal drugs like β-lactams and aminoglycosides produce rapid killing effects compared to bacteriostatic agents.
References
- Goodman & Gilman’s The Pharmacological Basis of Therapeutics
- Katzung’s Basic and Clinical Pharmacology
- Harrison’s Principles of Internal Medicine
- Mandell, Douglas, and Bennett’s Principles and Practice of Infectious Diseases
Related Internal Links

I am pursuing MBA in pharmaceutical management from NIPER Hyderabad with a strong academic record and proven success in national-level pharmacy entrance exams. I secured AIR 61 in NIPER 2024 (MS/M.Pharm) and AIR 27 in NIPER MBA, along with AIR 147 in GPAT 2024 and AIR 907 in GPAT 2023. I also achieved AIR 6 in AIIMS CRE-2025 for Drug Store Keeper and was selected as a Pharmacist (AIR 61) for ESIC. Additionally, I was the Runner-Up in Round 2 of the EY Case Study Competition.
At PharmacyFreak.com, I aim to guide future pharmacists through expert content, exam strategies, and insightful resources based on real experience and academic excellence.
Mail- harsh@pharmacyfreak.com