Table of Contents
Introduction
Aspirin, also known as acetylsalicylic acid, is a widely used Non-Steroidal Anti-Inflammatory Drug (NSAID). It’s primarily known for its analgesic (pain-relieving), antipyretic (fever-reducing), anti-inflammatory, and antiplatelet actions.
Belonging to the salicylate class, Aspirin is often prescribed for:
- Mild to moderate pain
- Inflammatory conditions like arthritis
- Cardiovascular protection (to prevent clot formation)
Due to its clinical importance and frequent exam presence, understanding its mechanism of action is essential for students preparing for GPAT, NEET-PG, NIPER, MBBS, and NCLEX.
Stepwise Mechanism of Action of Aspirin
- Aspirin is administered (usually orally).
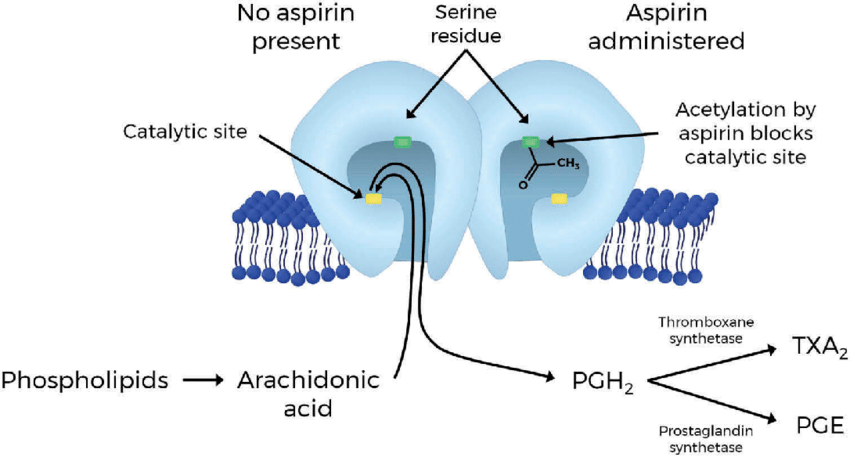
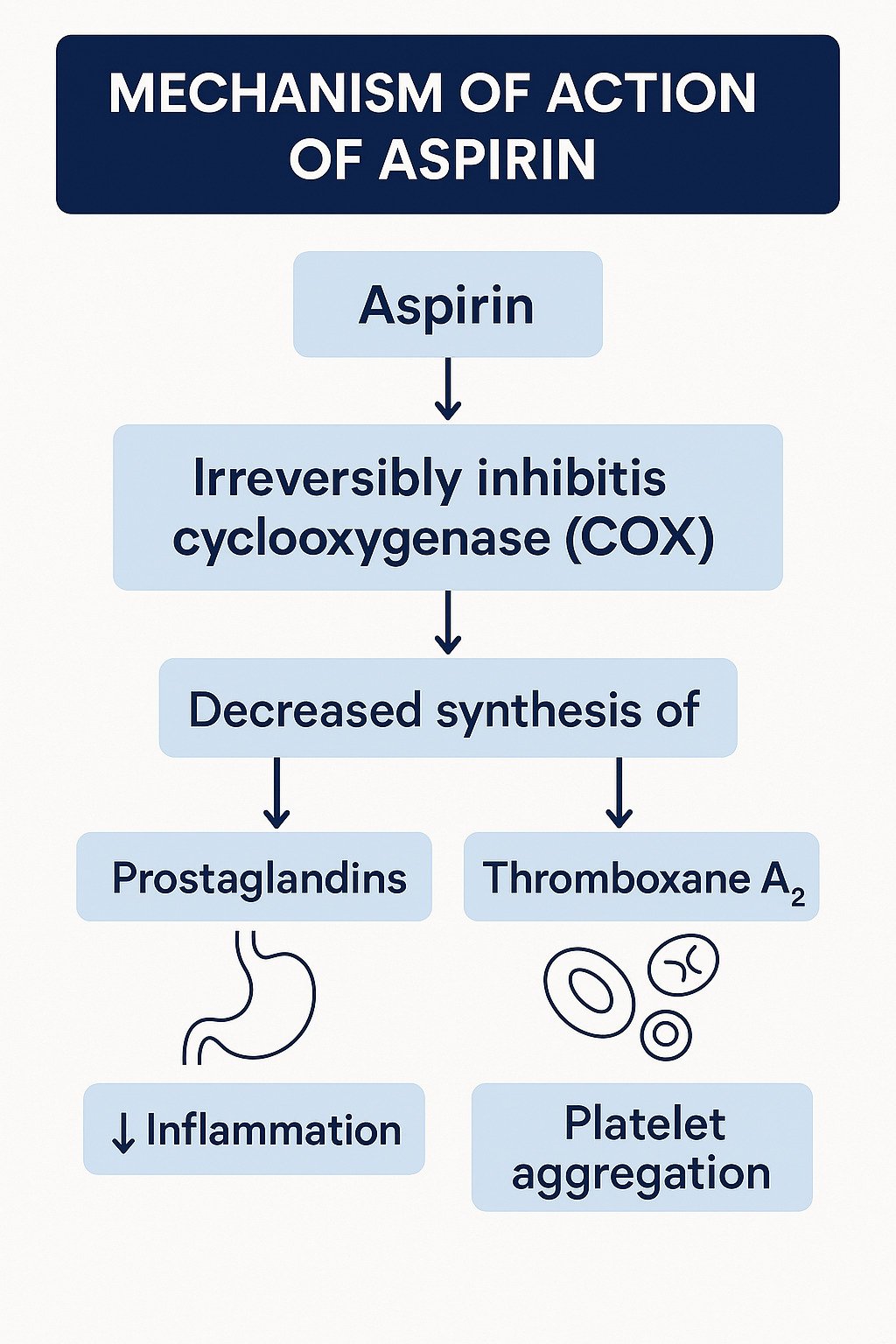
- It gets absorbed and irreversibly inhibits the cyclooxygenase enzymes – COX-1 and COX-2 by acetylating serine residues in the active site.
- This blocks the conversion of arachidonic acid to prostaglandin H₂ (PGH₂), the precursor of prostaglandins and thromboxanes.
- As a result:
- Prostaglandin synthesis is reduced, leading to reduced inflammation, fever, and pain.
- Thromboxane A₂ synthesis is inhibited, which reduces platelet aggregation and provides an antiplatelet effect.
Clinical Applications of Aspirin
- Analgesic: Relief in headache, myalgia, arthralgia, and other mild to moderate pain
- Antipyretic: Reduces fever by acting on the hypothalamic heat-regulating center
- Anti-inflammatory: Used in rheumatoid arthritis and other inflammatory conditions
- Antiplatelet Agent: Low-dose aspirin is used in myocardial infarction, stroke prevention, and other thrombotic conditions
Adverse Effects
- Gastric irritation, peptic ulcers, and GI bleeding (due to COX-1 inhibition)
- Tinnitus (especially at high doses)
- Hypersensitivity reactions
- Reye’s syndrome (in children with viral infections – hence contraindicated)
Aspirin vs. Other NSAIDs (e.g., Ibuprofen):
| Feature | Aspirin | Ibuprofen |
|---|---|---|
| COX Inhibition | Irreversible (COX-1 >> COX-2) | Reversible (COX-1 and COX-2) |
| Antiplatelet Effect | Strong and long-lasting | Minimal and reversible |
| Use in CV protection | Preferred (low dose) | Not used |
| GI Irritation | Higher (COX-1 inhibition) | Lower |
| Duration of Action | Longer for antiplatelet (~7–10 days) | Short (~4–6 hours) |
MCQs for Practice
Q1. Aspirin acts by inhibiting:
A. Thromboxane synthase
B. Lipoxygenase
C. Cyclooxygenase (COX) enzymes ✅
D. Prostaglandin E synthase
Q2. Which effect of aspirin is due to inhibition of thromboxane A₂?
A. Analgesic
B. Antipyretic
C. Antiplatelet ✅
D. Anti-inflammatory
Q3. Which enzyme is irreversibly inhibited by aspirin?
A. Phospholipase A2
B. Cyclooxygenase ✅
C. Lipoxygenase
D. Thromboxane synthase
Q4. Which of the following is NOT a use of low-dose aspirin?
A. Fever
B. Stroke prophylaxis
C. Myocardial infarction prevention
D. Pain relief ✅
Q5. Which adverse effect is uniquely associated with aspirin use in children?
A. Hepatitis
B. Reye’s Syndrome ✅
C. Gastritis
D. Asthma
Q6. Which of the following explains the prolonged antiplatelet effect of aspirin?
A. It reversibly inhibits thromboxane A₂
B. It irreversibly inhibits COX-2 in liver
C. It irreversibly inhibits COX-1 in platelets ✅
D. It enhances prostacyclin synthesis
Q7. Aspirin is contraindicated in children with viral infections because of the risk of:
A. Guillain-Barré Syndrome
B. Reye’s Syndrome ✅
C. Steven-Johnson Syndrome
D. Toxic epidermal necrolysis
Q8. The antipyretic effect of aspirin is mainly due to:
A. Decreased platelet aggregation
B. Central inhibition of PGE₂ synthesis ✅
C. Blocking leukotriene formation
D. Vasoconstriction in skin vessels
Q9. The analgesic action of aspirin is primarily mediated by:
A. Direct stimulation of opioid receptors
B. Activation of adrenergic pathways
C. Inhibition of peripheral nociceptor sensitization ✅
D. CNS dopamine enhancement
Q10. Which of the following statements is TRUE regarding aspirin’s pharmacokinetics?
A. It is rapidly absorbed but poorly protein-bound
B. It has a long half-life as aspirin itself
C. It undergoes hepatic metabolism to salicylate ✅
D. It is excreted unchanged in feces
FAQs
Q1: Why is aspirin used in heart attack prevention?
A: It inhibits thromboxane A₂, reducing platelet aggregation and preventing clot formation.
Q2: Why should aspirin not be given to children with viral fever?
A: Due to the risk of Reye’s syndrome, a rare but serious condition.
Q3: Is aspirin a selective COX-2 inhibitor?
A: No, it is a non-selective, irreversible COX-1 and COX-2 inhibitor.
References
- KD Tripathi – Essentials of Medical Pharmacology
- Sparsh Gupta – Review of Pharmacology
- Goodman & Gilman – The Pharmacological Basis of Therapeutics
- PubMed & NCBI articles on aspirin pharmacodynamics and antiplatelet effects

I am pursuing MBA in pharmaceutical management from NIPER Hyderabad with a strong academic record and proven success in national-level pharmacy entrance exams. I secured AIR 61 in NIPER 2024 (MS/M.Pharm) and AIR 27 in NIPER MBA, along with AIR 147 in GPAT 2024 and AIR 907 in GPAT 2023. I also achieved AIR 6 in AIIMS CRE-2025 for Drug Store Keeper and was selected as a Pharmacist (AIR 61) for ESIC. Additionally, I was the Runner-Up in Round 2 of the EY Case Study Competition.
At PharmacyFreak.com, I aim to guide future pharmacists through expert content, exam strategies, and insightful resources based on real experience and academic excellence.
Mail- harsh@pharmacyfreak.com

many many thanks for your solid information 👍👍
Welcome! This encourage us to create more such valuable content.