Table of Contents
Introduction
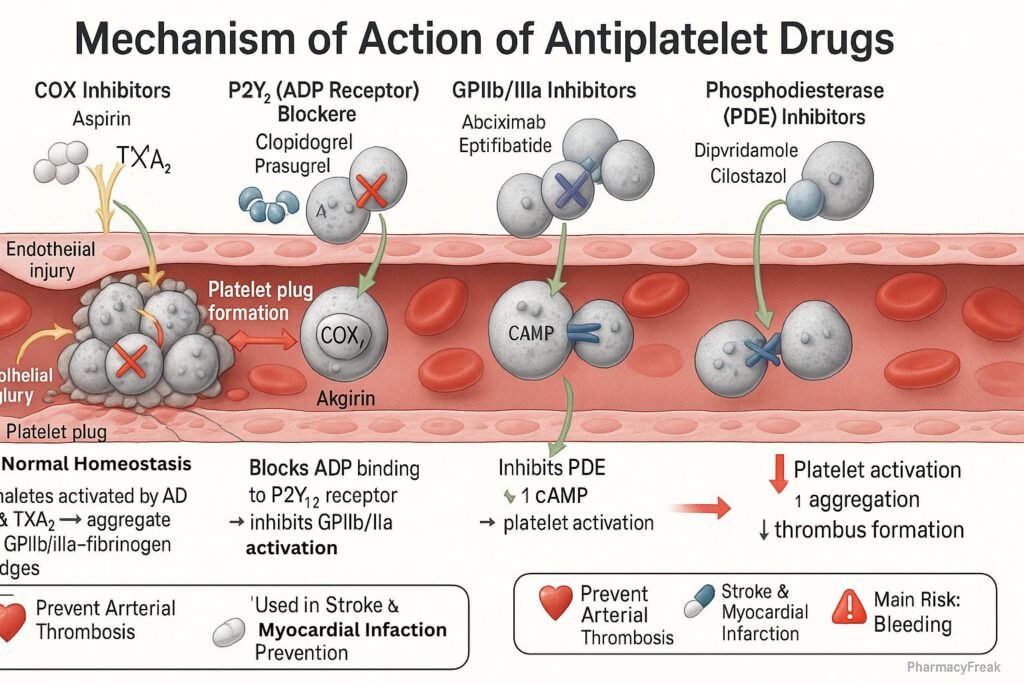
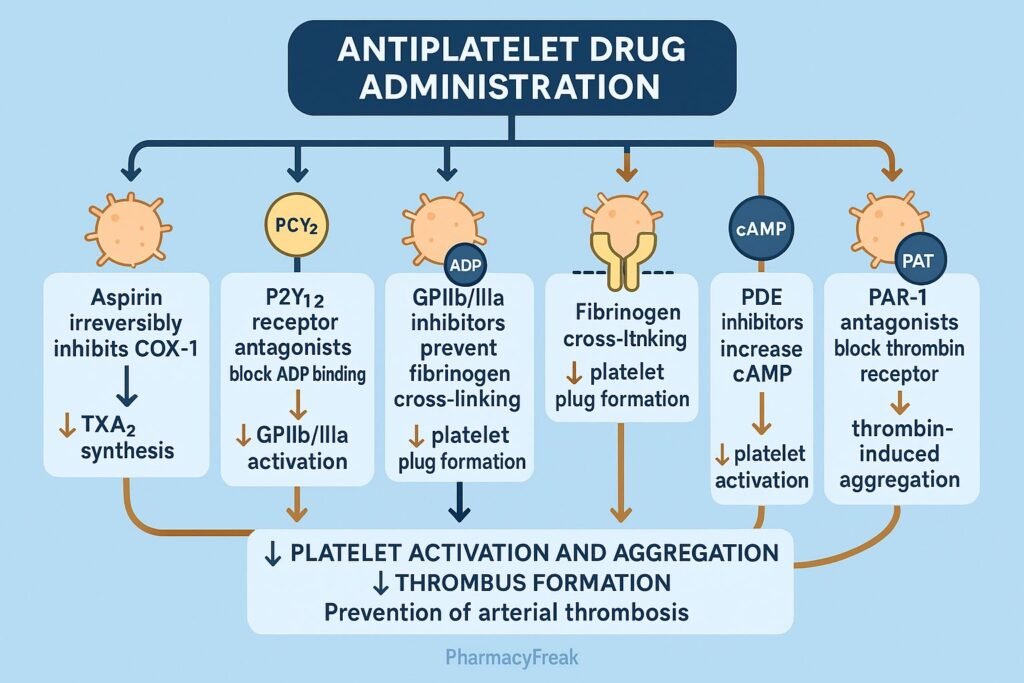
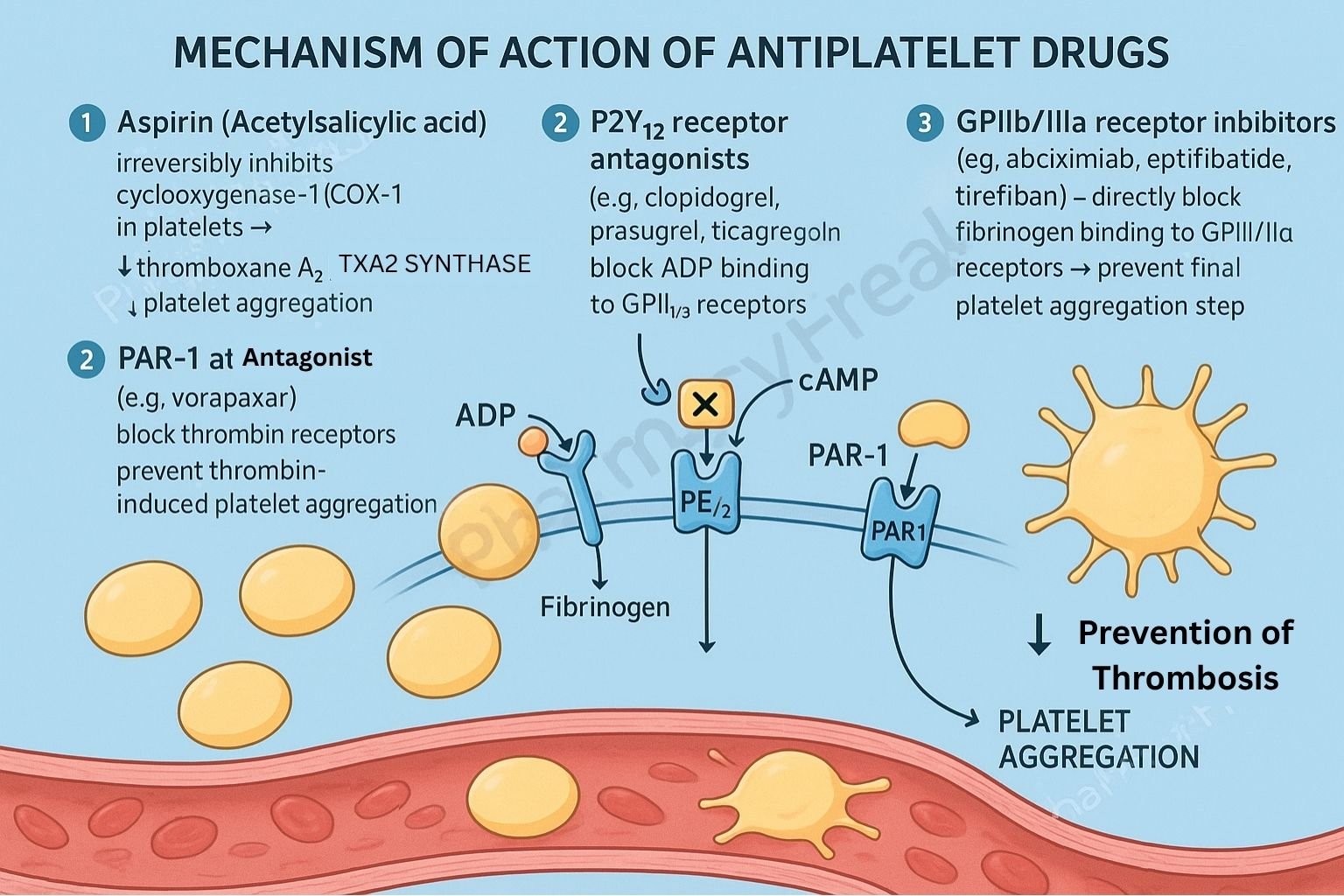
Antiplatelet drugs are pharmacological agents that inhibit platelet aggregation, thereby preventing arterial thrombosis — a key contributor to myocardial infarction, ischemic stroke, and peripheral artery disease. Mechanism of Action of Antiplatelet Drugs involves blocking platelet activation pathways mediated by cyclooxygenase (COX-1), ADP receptors (P2Y₁₂), glycoprotein IIb/IIIa receptors, and thromboxane A₂ synthesis. Unlike anticoagulants, which affect the coagulation cascade, antiplatelet drugs target primary hemostasis to prevent clot formation at sites of vascular injury.
Mechanism of Action (Step-wise)
Antiplatelet drugs inhibit platelet activation and aggregation through different molecular mechanisms depending on their drug class.
1. Cyclooxygenase (COX-1) Inhibitors
- Mechanism:
- Inhibit cyclooxygenase-1 (COX-1) irreversibly in platelets, preventing the synthesis of thromboxane A₂ (TXA₂) — a potent vasoconstrictor and platelet aggregator.
- As platelets lack nuclei, the effect persists for their lifespan (~7–10 days).
- Example: Aspirin (Acetylsalicylic acid).
- Effect: ↓ TXA₂ → ↓ Platelet aggregation and vasoconstriction.
- Clinical Use: Myocardial infarction prophylaxis, ischemic stroke prevention, post-stent therapy.
2. ADP Receptor (P2Y₁₂) Inhibitors
- Mechanism:
- Block P2Y₁₂ ADP receptors on platelet membranes → inhibit activation of glycoprotein IIb/IIIa complex → prevent platelet aggregation.
- Effects are irreversible for thienopyridines and reversible for newer agents.
- Examples:
- Irreversible: Clopidogrel, Prasugrel, Ticlopidine.
- Reversible: Ticagrelor, Cangrelor.
- Effect: ↓ ADP-mediated platelet activation → ↓ thrombus formation.
- Clinical Use: Dual antiplatelet therapy (DAPT) with aspirin after PCI, acute coronary syndrome (ACS).
3. Glycoprotein IIb/IIIa Receptor Antagonists
- Mechanism:
- Block GPIIb/IIIa receptors, the final common pathway for platelet aggregation by preventing fibrinogen binding between activated platelets.
- Examples: Abciximab, Eptifibatide, Tirofiban.
- Effect: ↓ Platelet cross-linking → ↓ Thrombus formation.
- Clinical Use: During percutaneous coronary intervention (PCI), unstable angina, non-STEMI.
4. Phosphodiesterase (PDE) Inhibitors
- Mechanism:
- Inhibit phosphodiesterase (PDE3) enzyme → increase intracellular cyclic AMP (cAMP) → inhibit platelet aggregation and cause vasodilation.
- Examples: Dipyridamole, Cilostazol.
- Effect: ↑ cAMP → ↓ Platelet activation and improved microcirculation.
- Clinical Use: Intermittent claudication, stroke prevention (with aspirin).
5. Thromboxane A₂ Synthesis Inhibitors
- Mechanism:
- Directly inhibit TXA₂ synthase, decreasing platelet aggregation and vasoconstriction.
- Example: Picotamide.
- Effect: ↓ TXA₂ production → ↓ Platelet aggregation.
6. Protease-Activated Receptor-1 (PAR-1) Antagonists
- Mechanism:
- Inhibit thrombin-mediated platelet activation by blocking PAR-1 receptors.
- Example: Vorapaxar.
- Effect: ↓ Thrombin-induced platelet aggregation.
- Clinical Use: Secondary prevention of atherothrombotic events (post-MI, PAD).
Comparative Summary Table
| Drug Class | Primary Target | Mechanism | Examples | Key Use |
|---|---|---|---|---|
| COX-1 Inhibitors | COX-1 enzyme | ↓ TXA₂ synthesis | Aspirin | MI, Stroke prevention |
| P2Y₁₂ Inhibitors | ADP receptor | ↓ ADP-mediated activation | Clopidogrel, Prasugrel, Ticagrelor | DAPT, ACS |
| GPIIb/IIIa Blockers | GPIIb/IIIa receptor | ↓ Fibrinogen binding | Abciximab, Eptifibatide | PCI, Unstable angina |
| PDE Inhibitors | PDE enzyme | ↑ cAMP → ↓ aggregation | Dipyridamole, Cilostazol | Stroke prevention |
| TXA₂ Synthase Inhibitors | TXA₂ synthase | ↓ TXA₂ formation | Picotamide | Arterial thrombosis |
| PAR-1 Antagonists | PAR-1 receptor | ↓ Thrombin activation | Vorapaxar | Secondary MI prevention |
Pharmacokinetics
- Aspirin: Rapid oral absorption; hepatic metabolism; irreversible platelet inhibition.
- Clopidogrel: Prodrug activated by CYP2C19; onset within hours; irreversible P2Y₁₂ inhibition.
- Ticagrelor: Direct-acting; faster onset and offset.
- Abciximab: IV administration; rapid effect; short plasma half-life but prolonged receptor blockade.
- Cilostazol: Oral; metabolized via CYP3A4; contraindicated in heart failure.
Adverse Effects
- Aspirin: Gastric irritation, bleeding, hypersensitivity, tinnitus (high dose).
- Clopidogrel/Prasugrel: Bleeding, rare thrombotic thrombocytopenic purpura (TTP).
- Ticagrelor: Dyspnea, bradycardia.
- GPIIb/IIIa Inhibitors: Bleeding, thrombocytopenia.
- Cilostazol: Headache, palpitations, contraindicated in heart failure.
MCQs
1. Aspirin inhibits platelet aggregation by blocking:
a) ADP receptors
b) COX-1 enzyme
c) GPIIb/IIIa receptors
d) PDE enzyme
Answer: b) COX-1 enzyme
2. Which drug irreversibly inhibits the P2Y₁₂ receptor?
a) Ticagrelor
b) Clopidogrel
c) Cilostazol
d) Dipyridamole
Answer: b) Clopidogrel
3. The final common pathway of platelet aggregation involves:
a) P2Y₁₂ receptor
b) GPIIb/IIIa receptor
c) PDE enzyme
d) COX-1 enzyme
Answer: b) GPIIb/IIIa receptor
4. Vorapaxar acts by blocking:
a) PAR-1 receptor
b) ADP receptor
c) COX-1
d) TXA₂ synthase
Answer: a) PAR-1 receptor
5. Dipyridamole increases platelet cAMP by inhibiting:
a) PDE3 enzyme
b) COX-1
c) ADP receptor
d) TXA₂ synthase
Answer: a) PDE3 enzyme
6. Which drug combination forms dual antiplatelet therapy (DAPT)?
a) Aspirin + Clopidogrel
b) Clopidogrel + Cilostazol
c) Aspirin + Heparin
d) Aspirin + Warfarin
Answer: a) Aspirin + Clopidogrel
7. The duration of aspirin’s antiplatelet effect lasts:
a) 12 hours
b) 24 hours
c) 3–5 days
d) 7–10 days
Answer: d) 7–10 days
8. Which antiplatelet drug is contraindicated in heart failure?
a) Cilostazol
b) Clopidogrel
c) Ticagrelor
d) Aspirin
Answer: a) Cilostazol
9. Which enzyme activates clopidogrel?
a) CYP3A4
b) CYP2C19
c) MAO-A
d) CYP1A2
Answer: b) CYP2C19
10. The major adverse effect of antiplatelet therapy is:
a) Bleeding
b) Hypertension
c) Bradycardia
d) Hypoglycemia
Answer: a) Bleeding
FAQs
Q1. How do antiplatelet drugs differ from anticoagulants?
Antiplatelet drugs inhibit platelet aggregation, while anticoagulants inhibit fibrin formation in the coagulation cascade.
Q2. Why is dual antiplatelet therapy (DAPT) used?
To enhance efficacy — Aspirin inhibits COX-1 and Clopidogrel blocks ADP receptors, providing additive inhibition.
Q3. Can aspirin and clopidogrel be taken together long-term?
Yes, in patients with stents or coronary artery disease, but duration depends on bleeding risk.
Q4. What is the role of GPIIb/IIIa inhibitors in therapy?
Used in acute coronary syndromes and PCI for rapid, potent platelet inhibition.
Q5. Which genetic factor affects clopidogrel efficacy?
CYP2C19 polymorphisms can reduce clopidogrel activation and antiplatelet effect.
References

I am pursuing MBA in pharmaceutical management from NIPER Hyderabad with a strong academic record and proven success in national-level pharmacy entrance exams. I secured AIR 61 in NIPER 2024 (MS/M.Pharm) and AIR 27 in NIPER MBA, along with AIR 147 in GPAT 2024 and AIR 907 in GPAT 2023. I also achieved AIR 6 in AIIMS CRE-2025 for Drug Store Keeper and was selected as a Pharmacist (AIR 61) for ESIC. Additionally, I was the Runner-Up in Round 2 of the EY Case Study Competition.
At PharmacyFreak.com, I aim to guide future pharmacists through expert content, exam strategies, and insightful resources based on real experience and academic excellence.
Mail- harsh@pharmacyfreak.com

amazing