Table of Contents
Introduction
Tranexamic acid (TXA) is an antifibrinolytic agent commonly used to control or prevent excessive bleeding in trauma, surgery, heavy menstrual bleeding, and in hemophilia patients undergoing dental procedures. It stabilizes clots by inhibiting the breakdown of fibrin, thus reducing blood loss and improving hemostasis.
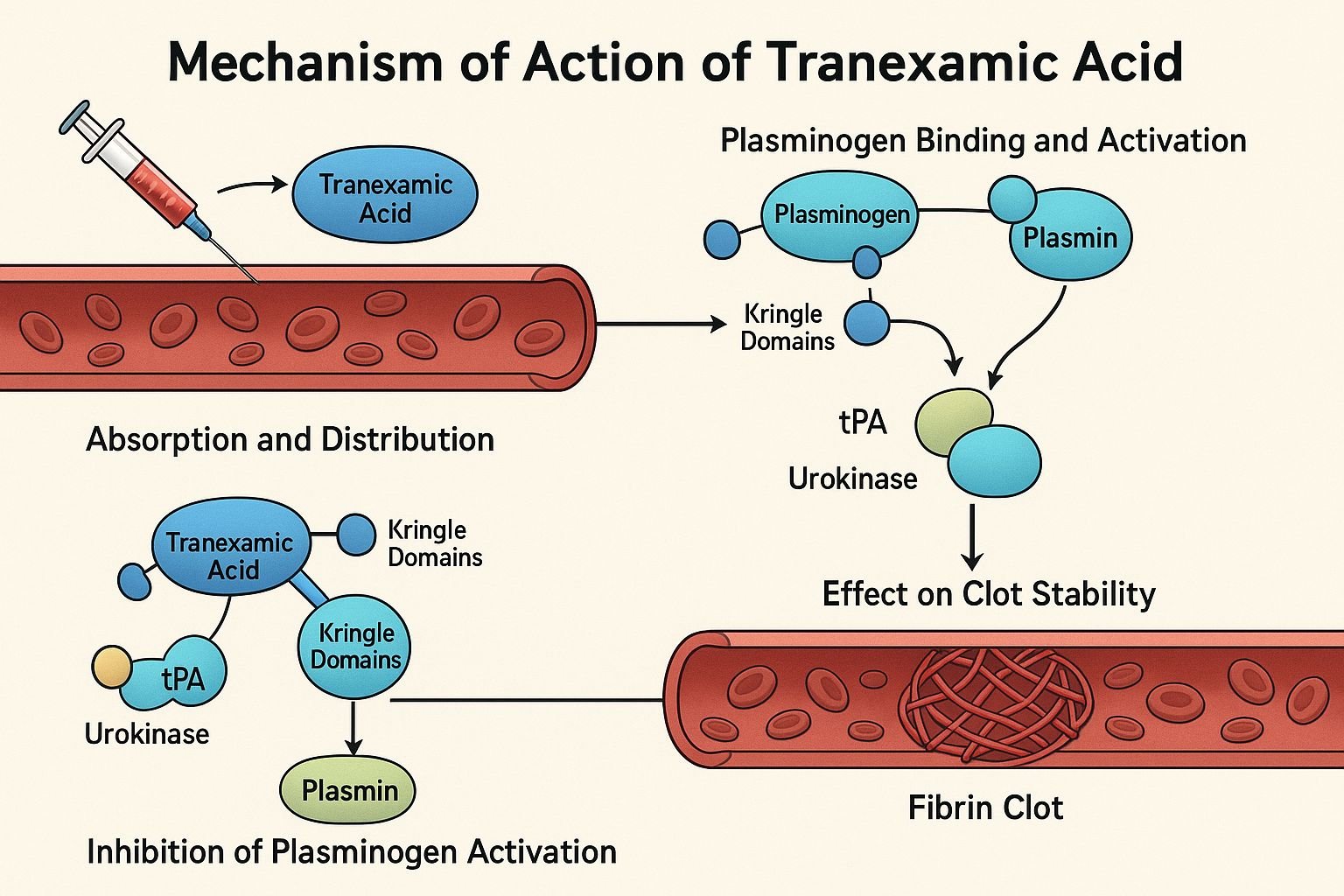
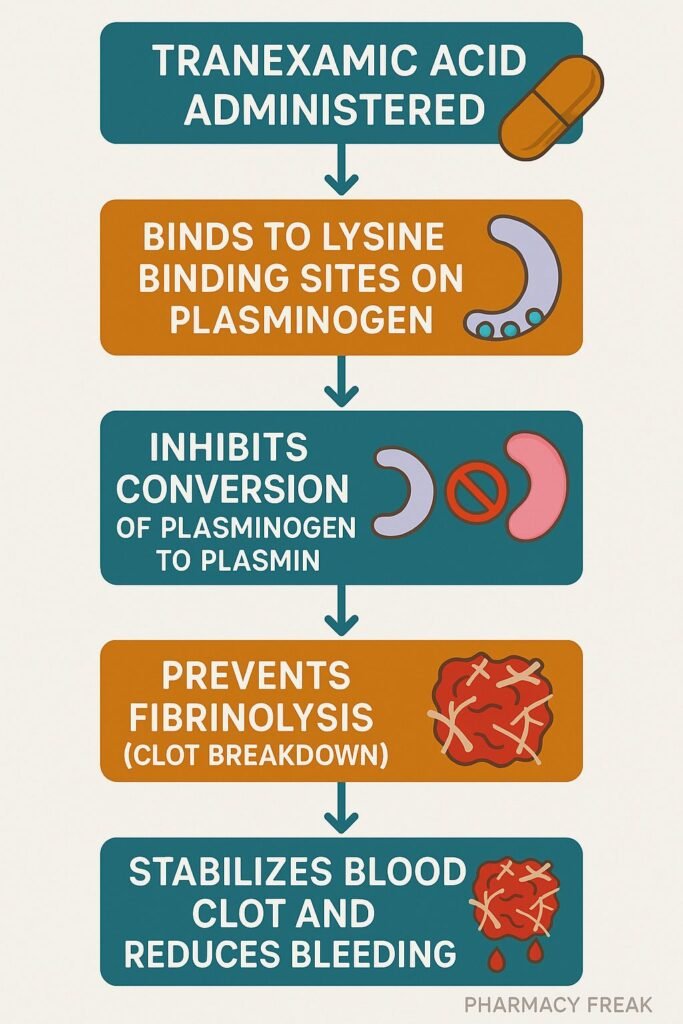
Step-by-Step Mechanism of Action
- Competitive inhibition of plasminogen activation
TXA is a synthetic lysine analog that binds to lysine-binding sites on plasminogen, preventing its conversion to plasmin and subsequent binding to fibrin. - Inhibition of plasmin activity
At higher concentrations, TXA directly inhibits plasmin’s proteolytic activity, further slowing fibrin degradation. - Stabilization of fibrin clot architecture
By reducing plasmin activity, the fibrin matrix remains intact longer, enhancing clot stability and reducing bleeding. - Anti-inflammatory properties (Additional benefit)
TXA has been shown to reduce inflammatory mediator release post-trauma and protect endothelial integrity.
Pharmacokinetic Parameters
| Parameter | Value |
|---|---|
| Bioavailability | ~30–50% (oral) |
| Peak plasma | ~2–3 hours (oral) |
| Volume of distribution | 9–12 L; crosses placenta & CSF |
| Metabolism | Minimal (~5%) |
| Elimination | Renal (95% unchanged) |
| Half-life | ~2–11 hours (depending on route) |
Clinical Uses
- Trauma-related hemorrhage (e.g., in trauma protocols)
- Postpartum hemorrhage
- Heavy menstrual bleeding
- Perioperative bleeding in cardiac, orthopedic, dental, and urologic surgeries
- Hemoptysis, epistaxis
Adverse Effects
- Common: nausea, diarrhea, vomiting, allergic reactions
- Rare but serious: seizures, visual disturbances, venous thromboembolism (in predisposed individuals)
- Caution in renal impairment due to renal excretion
Comparative Analysis
Tranexamic Acid vs ε‑Aminocaproic Acid:
- TXA is approximately 8 times more potent
- Both act via lysine-binding site inhibition
- TXA is preferred in acute bleeding scenarios due to stronger efficacy and better tissue penetration
MCQs
1. Tranexamic acid primarily prevents bleeding by:
a) Activating antithrombin III
b) Inhibiting plasminogen activation
c) Boosting platelet aggregation
d) Blocking vitamin K epoxide reductase
Answer: b) Inhibiting plasminogen activation
2. TXA’s action can best be described as:
a) Fibrinolytic
b) Antiplatelet
c) Antifibrinolytic
d) Thrombolytic
Answer: c) Antifibrinolytic
3. The critical time window for TXA use in trauma is:
a) 1 hour
b) 3 hours
c) 6 hours
d) 12 hours
Answer: b) 3 hours
4. Which route of TXA administration achieves ~50% bioavailability?
a) IV
b) Oral
c) Topical
d) Intramuscular
Answer: b) Oral
5. An uncommon serious adverse effect associated with TXA is:
a) Renal failure
b) Seizures
c) Bone marrow suppression
d) Hypertension
Answer: b) Seizures
FAQs
1. Can TXA be used orally?
Yes—very effective for heavy menstrual bleeding with oral bioavailability around 30–50%.
2. Does TXA require routine lab monitoring?
No routine labs are needed, but renal function should be monitored in at-risk patients.
3. Can TXA increase thrombosis risk?
Most studies show no significant increase, but caution is advised in patients with known thrombophilia.
4. Is TXA safe during pregnancy?
Yes, it is used for postpartum hemorrhage and is WHO-approved for such indications.
5. How soon after trauma must TXA be given?
Ideally within 3 hours to significantly reduce mortality from bleeding.
References
- Goodman & Gilman’s The Pharmacological Basis of Therapeutics, 13th Edition.
- KD Tripathi. Essentials of Medical Pharmacology, 8th Edition.
- https://www.ncbi.nlm.nih.gov/books/NBK532909/
- https://pubmed.ncbi.nlm.nih.gov/35834488/
- https://pmc.ncbi.nlm.nih.gov/articles/PMC4277654/
- https://pubmed.ncbi.nlm.nih.gov/30422504/

I am pursuing MBA in pharmaceutical management from NIPER Hyderabad with a strong academic record and proven success in national-level pharmacy entrance exams. I secured AIR 61 in NIPER 2024 (MS/M.Pharm) and AIR 27 in NIPER MBA, along with AIR 147 in GPAT 2024 and AIR 907 in GPAT 2023. I also achieved AIR 6 in AIIMS CRE-2025 for Drug Store Keeper and was selected as a Pharmacist (AIR 61) for ESIC. Additionally, I was the Runner-Up in Round 2 of the EY Case Study Competition.
At PharmacyFreak.com, I aim to guide future pharmacists through expert content, exam strategies, and insightful resources based on real experience and academic excellence.
Mail- harsh@pharmacyfreak.com