Introduction
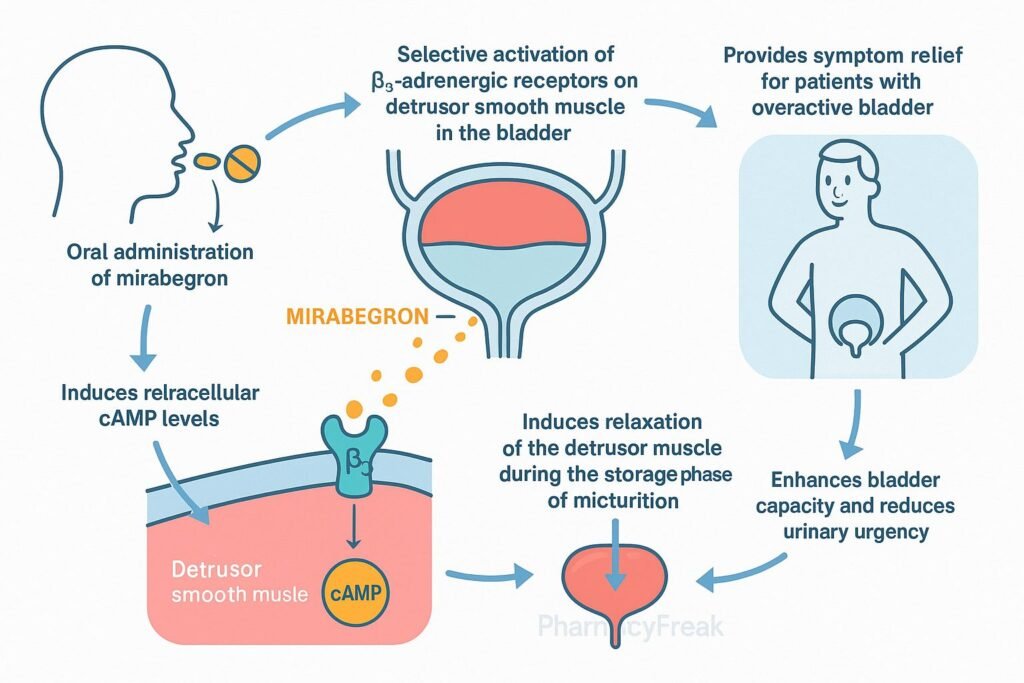
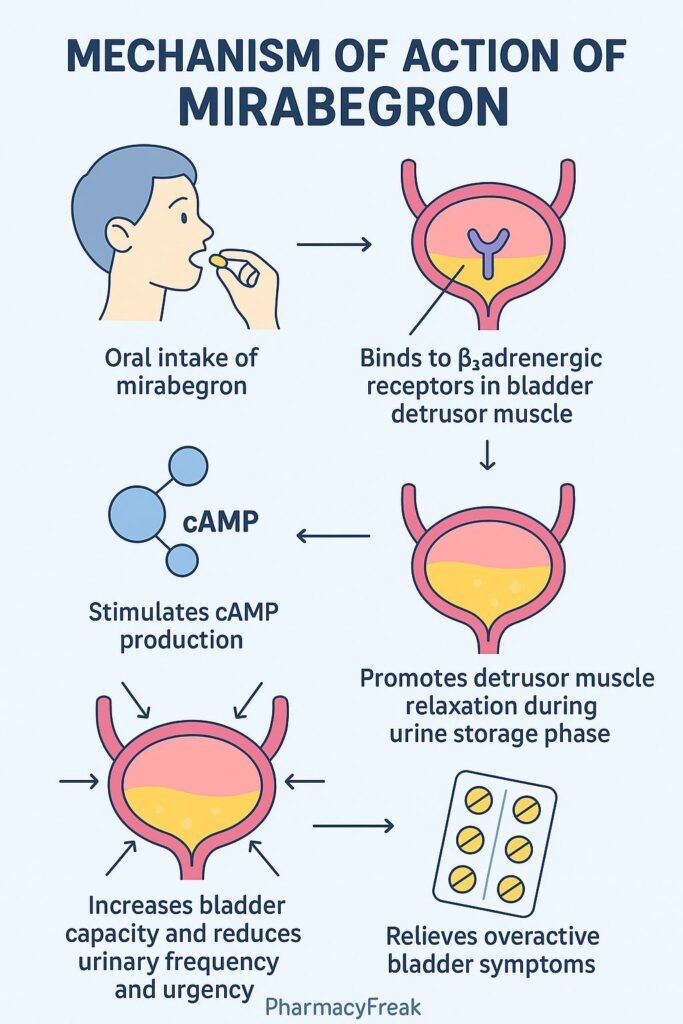
Mirabegron is a β₃‑adrenergic receptor agonist used to treat overactive bladder (OAB). By selectively activating β₃‑receptors in the detrusor muscle of the bladder, it enhances urine storage and reduces urinary urgency and frequency without significantly affecting cardiovascular β₁ or β₂ receptors.
Step-by-Step Mechanism of Action
- Selective β₃‑Agonism
Mirabegron binds to β₃‑adrenergic receptors in the bladder detrusor muscle. - Activation of Adenylyl Cyclase
Receptor activation triggers Gs-protein pathways, increasing cAMP production. - Detrusor Muscle Relaxation
Elevated cAMP leads to relaxation of the detrusor muscle during bladder filling. - Improved Bladder Sensitivity
Relaxation increases bladder capacity and delays the activation threshold of stretch receptors. - Urinary Symptom Relief
The result is reduced urgency episodes, decreased frequency, and fewer incontinence events.
Pharmacokinetic Parameters
| Parameter | Value |
|---|---|
| Bioavailability | ~29% (fasting) |
| Peak Plasma Time (Tₘₐₓ) | ~3.5 hours |
| Half-Life | ~50 hours |
| Protein Binding | ~71% |
| Metabolism | Hepatic via CYP3A4 and CYP2D6 |
| Excretion | ~55% fecal, ~45% renal |
Clinical Uses
- Treatment of overactive bladder with symptoms of urgency, frequency, or incontinence
Adverse Effects
- Hypertension
- Headache
- Nasopharyngitis
- Urinary tract infection
- Constipation
- Rare: tachycardia, dizziness
Comparative Analysis
| Feature | Mirabegron | Antimuscarinics (e.g., oxybutynin) |
|---|---|---|
| Mechanism | β₃‑agonist | Muscarinic receptor antagonist |
| Bladder Relaxation | Via cAMP-mediated detrusor relaxation | Blocks M₃ receptors inhibiting contraction |
| Dry Mouth Risk | Low | High |
| Constipation Risk | Low–moderate | Moderate–high |
| Cardiovascular Effects | Mild BP/HR increase possible | Minimal |
MCQs
1. Mirabegron primarily targets which receptor?
A. β₁‑adrenergic
B. β₂‑adrenergic
C. β₃‑adrenergic
D. M₃‑muscarinic
Answer: C
2. Activation of β₃-receptors in the bladder increases:
A. Intracellular Ca²⁺
B. cAMP
C. IP₃
D. DAG
Answer: B
3. The therapeutic effect of mirabegron is:
A. Increased urination frequency
B. Detrusor muscle contraction
C. Detrusor muscle relaxation
D. Alpha receptor blockade
Answer: C
4. Common side effect of mirabegron includes:
A. Severe dry mouth
B. Hypertension
C. Mydriasis
D. Urinary retention
Answer: B
5. Its half-life is approximately:
A. 10 hours
B. 24 hours
C. 50 hours
D. 72 hours
Answer: C
6. Mirabegron is metabolized by:
A. CYP1A2 only
B. CYP2E1 only
C. CYP3A4 and CYP2D6
D. Renal excretion without metabolism
Answer: C
7. Compared to antimuscarinics, it has:
A. Higher dry mouth risk
B. Lower dry mouth risk
C. Same side effect profile
D. More anticholinergic effects
Answer: B
8. Mirabegron helps relieve:
A. Stress urinary incontinence
B. Overflow incontinence only
C. Overactive bladder symptoms
D. Neuropathic bladder
Answer: C
9. Which is not a common ADR?
A. Headache
B. Hypotension
C. Constipation
D. Nasopharyngitis
Answer: B
10. Urinary effects result from:
A. Calcium channel blockade
B. Sodium channel inhibition
C. β₃‑mediated detrusor relaxation
D. Muscarinic receptor stimulation
Answer: C
FAQs
1. Is mirabegron anticholinergic?
No, it works via β₃‑adrenergic receptors, not by blocking cholinergic receptors.
2. Can it raise blood pressure?
Yes, mild to moderate increases in BP may occur.
3. Can it be used in men with BPH?
Yes, it’s approved for overactive bladder in both men and women, including those with BPH.
4. When should it be taken?
Once daily, with or without food.
5. Are there drug interactions?
Yes—especially with CYP3A4 or CYP2D6 inhibitors or inducers; dosage adjustments may be needed.
References
- DrugBank – Mirabegron Pharmacology & MOA
- FDA Prescribing Information – Mirabegron
- Goodman & Gilman’s: The Pharmacological Basis of Therapeutics
- Review Article – β₃-Adrenoceptor Agonists in Overactive Bladder Therapy
Related Links

I am pursuing MBA in pharmaceutical management from NIPER Hyderabad with a strong academic record and proven success in national-level pharmacy entrance exams. I secured AIR 61 in NIPER 2024 (MS/M.Pharm) and AIR 27 in NIPER MBA, along with AIR 147 in GPAT 2024 and AIR 907 in GPAT 2023. I also achieved AIR 6 in AIIMS CRE-2025 for Drug Store Keeper and was selected as a Pharmacist (AIR 61) for ESIC. Additionally, I was the Runner-Up in Round 2 of the EY Case Study Competition.
At PharmacyFreak.com, I aim to guide future pharmacists through expert content, exam strategies, and insightful resources based on real experience and academic excellence.
Mail- harsh@pharmacyfreak.com

