Table of Contents
Introduction
Erythromycin is a macrolide antibiotic widely used in the treatment of infections caused by gram-positive cocci, atypical pathogens, and certain gram-negative organisms. It is a bacteriostatic agent that inhibits bacterial protein synthesis and serves as an important alternative in patients allergic to penicillin. From an exam perspective, erythromycin is high-yield due to its ribosomal binding site, drug interactions, and characteristic adverse effects.
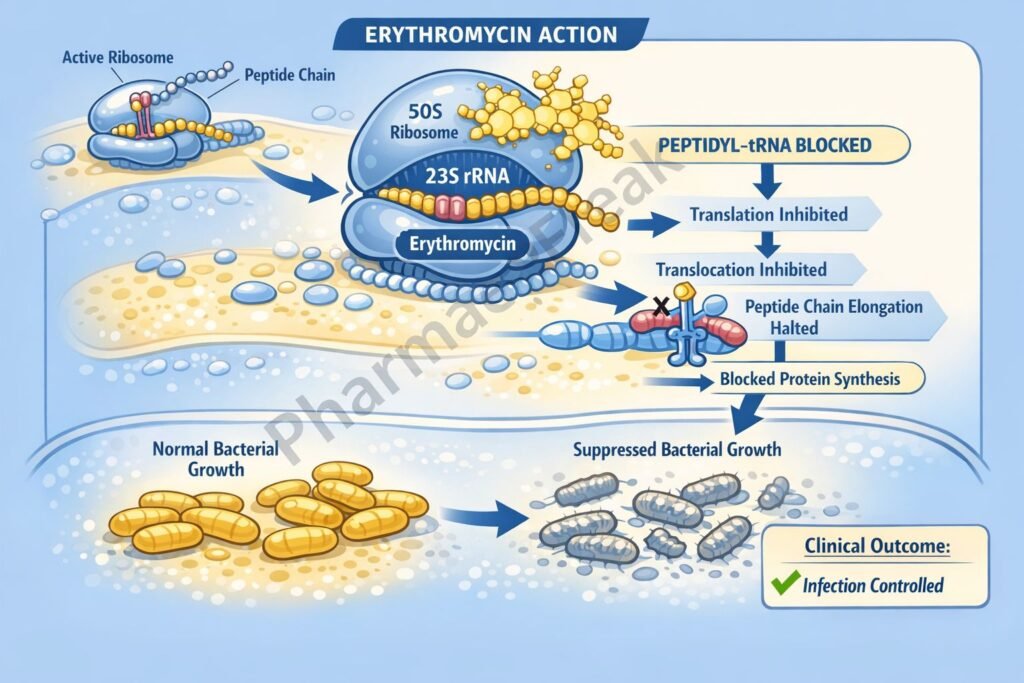
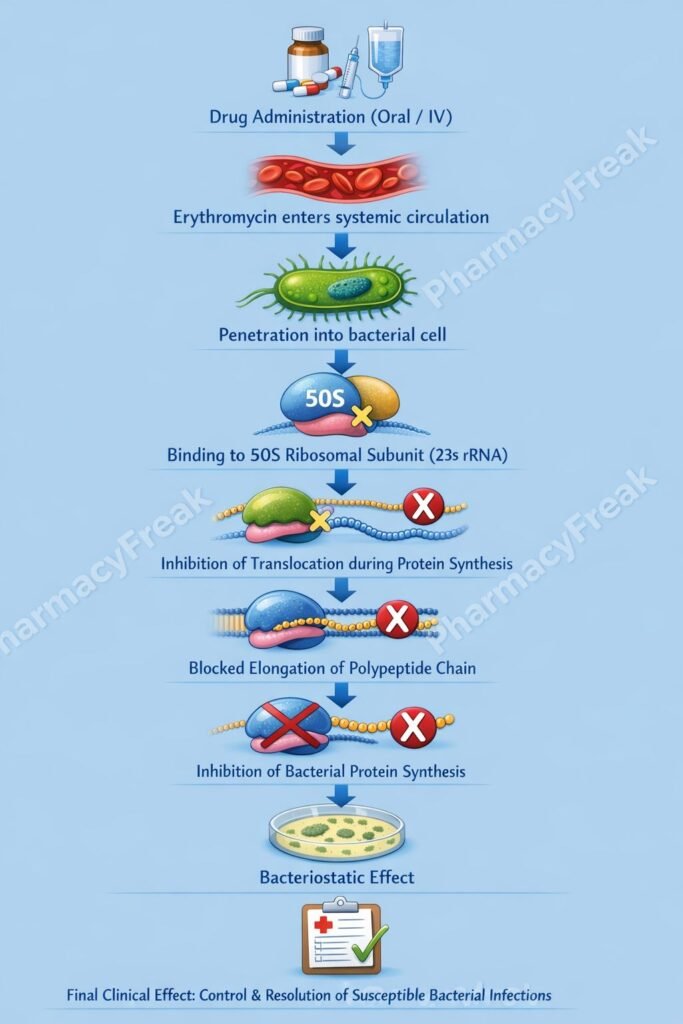
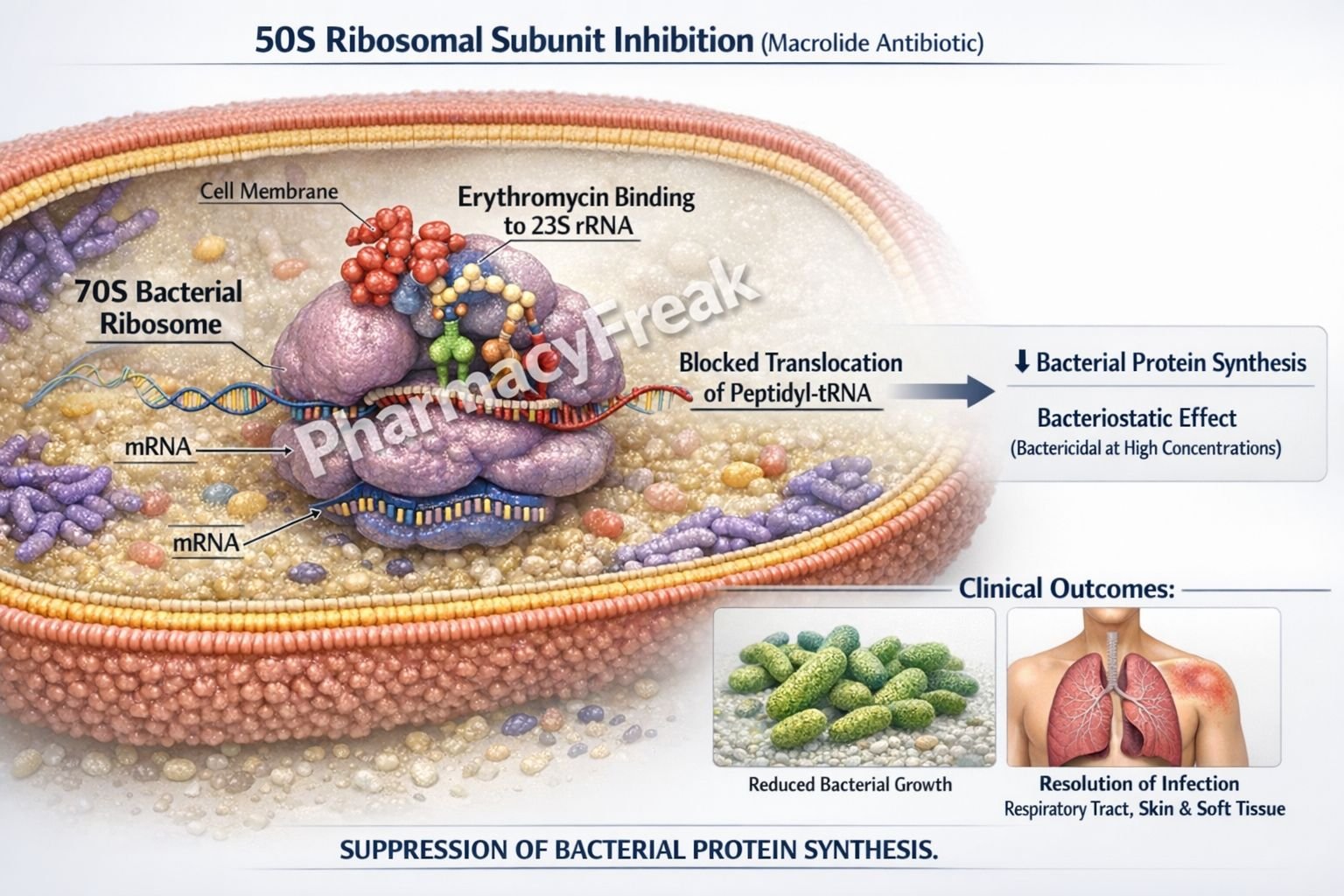
Mechanism of Action (Step-wise)
Erythromycin inhibits bacterial protein synthesis by acting at the ribosomal level.
Step 1: Entry into bacterial cell
Erythromycin penetrates susceptible bacteria and reaches the ribosomal machinery.
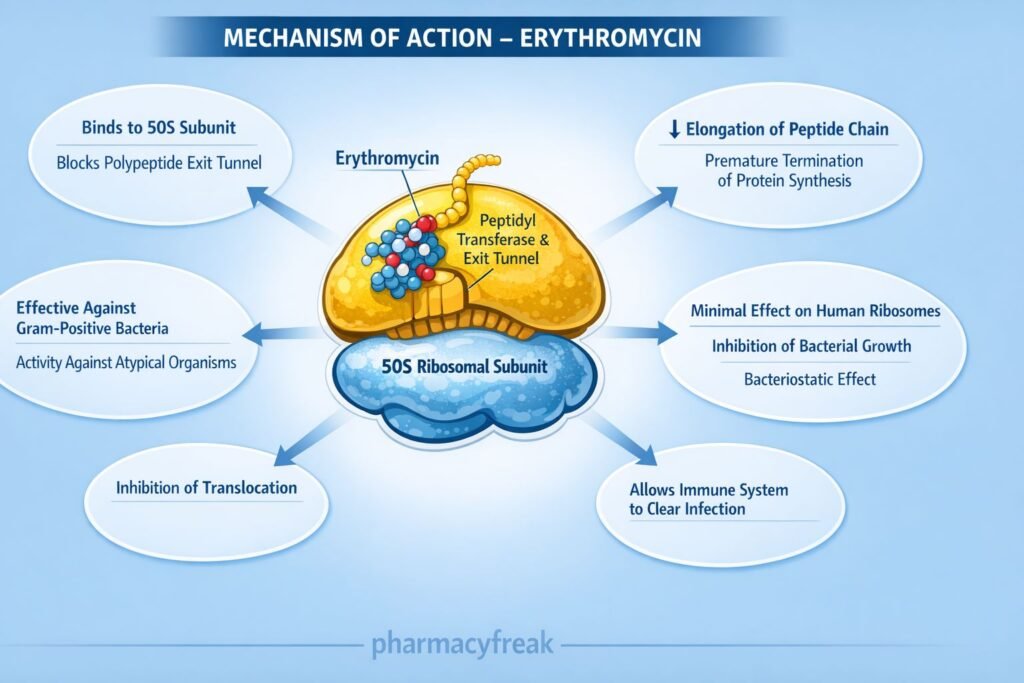
Step 2: Binding to 50S ribosomal subunit
It binds reversibly to the 23S rRNA of the 50S ribosomal subunit.
Step 3: Inhibition of translocation
Erythromycin blocks the translocation step during protein elongation, preventing movement of the growing peptide chain from the A site to the P site.
Step 4: Suppression of protein synthesis
Inhibition of translocation halts bacterial protein synthesis, leading to impaired bacterial growth.
Step 5: Bacteriostatic effect
At usual therapeutic concentrations, erythromycin is bacteriostatic, though it may be bactericidal against highly sensitive organisms at high concentrations.
Pharmacokinetics
- Route of administration: Oral, IV, topical
- Oral absorption: Acid-labile (enteric-coated or ester forms used)
- Distribution: Widely distributed; poor CNS penetration
- Protein binding: High
- Metabolism: Hepatic (potent CYP3A4 inhibitor)
- Half-life: ~1.5–2 hours
- Excretion: Mainly via bile; small amount in urine
Clinical Uses
- Respiratory tract infections (Streptococcus pneumoniae, Mycoplasma pneumoniae)
- Atypical pneumonia (Mycoplasma, Chlamydia, Legionella)
- Diphtheria (alternative to penicillin)
- Pertussis
- Chlamydial infections
- Acne vulgaris (topical use)
- Gastroparesis (prokinetic action via motilin receptor stimulation)
Adverse Effects
Gastrointestinal:
- Nausea, vomiting
- Abdominal cramps
- Diarrhea (motilin receptor stimulation)
Hepatic:
- Cholestatic hepatitis (especially with estolate form)
Cardiac:
- QT interval prolongation
- Risk of torsades de pointes
Drug interactions:
- Increased levels of theophylline, warfarin, carbamazepine, statins (CYP3A4 inhibition)
Comparative Analysis
Erythromycin vs Azithromycin vs Clarithromycin
| Feature | Erythromycin | Azithromycin | Clarithromycin |
|---|---|---|---|
| Ribosomal binding | 50S | 50S | 50S |
| Half-life | Short | Very long | Intermediate |
| CYP3A4 inhibition | Strong | Minimal | Moderate |
| GI intolerance | High | Low | Moderate |
| Drug interactions | Common | Rare | Moderate |
Explanation:
Erythromycin is associated with significant gastrointestinal intolerance and drug interactions due to strong CYP3A4 inhibition. Newer macrolides such as azithromycin offer improved tolerability and longer half-lives, making them preferable in many clinical situations.
MCQs
- Erythromycin inhibits bacterial protein synthesis by binding to:
a) 30S ribosomal subunit
b) 40S ribosomal subunit
c) 50S ribosomal subunit
d) DNA gyrase
Answer: c) 50S ribosomal subunit
- The specific step inhibited by erythromycin is:
a) Initiation
b) Peptide bond formation
c) Translocation
d) Termination
Answer: c) Translocation
- Erythromycin is primarily bacteriostatic because it:
a) Disrupts cell wall synthesis
b) Inhibits folate metabolism
c) Inhibits protein synthesis
d) Causes DNA damage
Answer: c) Inhibits protein synthesis
- Which enzyme system is inhibited by erythromycin?
a) CYP2C9
b) CYP1A2
c) CYP3A4
d) MAO
Answer: c) CYP3A4
- Prokinetic action of erythromycin is due to stimulation of:
a) Dopamine receptors
b) Serotonin receptors
c) Motilin receptors
d) Histamine receptors
Answer: c) Motilin receptors
- Which adverse effect is characteristic of erythromycin?
a) Nephrotoxicity
b) Ototoxicity
c) QT prolongation
d) Bone marrow suppression
Answer: c) QT prolongation
- Erythromycin estolate is associated with:
a) Renal failure
b) Cholestatic hepatitis
c) Hemolysis
d) Photosensitivity
Answer: b) Cholestatic hepatitis
- Compared to azithromycin, erythromycin has:
a) Longer half-life
b) Less GI intolerance
c) More drug interactions
d) Better gram-negative coverage
Answer: c) More drug interactions
- Which organism is classically treated with erythromycin?
a) Pseudomonas aeruginosa
b) Mycoplasma pneumoniae
c) Mycobacterium tuberculosis
d) Proteus mirabilis
Answer: b) Mycoplasma pneumoniae
- Erythromycin resistance most commonly occurs due to:
a) Efflux pumps
b) Enzyme activation
c) Alteration of ribosomal binding site
d) Increased permeability
Answer: c) Alteration of ribosomal binding site
FAQs
1. Why is erythromycin considered bacteriostatic?
It inhibits protein synthesis without directly killing bacteria.
2. Why is erythromycin poorly tolerated gastrointestinally?
Due to stimulation of motilin receptors in the gut.
3. Can erythromycin be used in penicillin allergy?
Yes, it is a common alternative.
4. Why does erythromycin cause drug interactions?
Because it strongly inhibits CYP3A4.
5. Is erythromycin effective against atypical organisms?
Yes, especially Mycoplasma, Chlamydia, and Legionella.
References
- Goodman & Gilman’s The Pharmacological Basis of Therapeutics
https://accesspharmacy.mhmedical.com - Katzung BG. Basic and Clinical Pharmacology
https://accessmedicine.mhmedical.com - Tripathi KD. Essentials of Medical Pharmacology
- Harrison’s Principles of Internal Medicine
https://accessmedicine.mhmedical.com

I am pursuing MBA in pharmaceutical management from NIPER Hyderabad with a strong academic record and proven success in national-level pharmacy entrance exams. I secured AIR 61 in NIPER 2024 (MS/M.Pharm) and AIR 27 in NIPER MBA, along with AIR 147 in GPAT 2024 and AIR 907 in GPAT 2023. I also achieved AIR 6 in AIIMS CRE-2025 for Drug Store Keeper and was selected as a Pharmacist (AIR 61) for ESIC. Additionally, I was the Runner-Up in Round 2 of the EY Case Study Competition.
At PharmacyFreak.com, I aim to guide future pharmacists through expert content, exam strategies, and insightful resources based on real experience and academic excellence.
Mail- harsh@pharmacyfreak.com