Table of Contents
Introduction
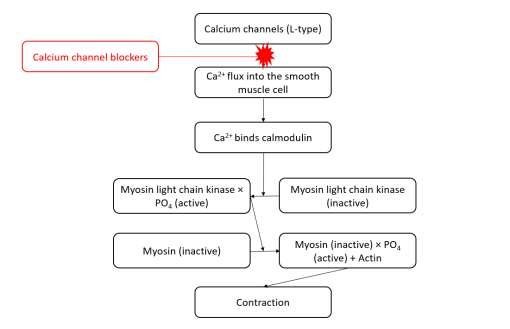
Calcium Channel Blockers (CCBs) are a major class of antihypertensive and anti-anginal medications. They work by blocking voltage-gated L-type calcium channels, leading to relaxation of smooth muscle in blood vessels and the heart.
CCBs are divided into two major subtypes:
- Dihydropyridines (DHPs) – e.g., Amlodipine, Nifedipine
- Predominantly affect vascular smooth muscle
- Used primarily for hypertension
- Non-dihydropyridines (non-DHPs) – e.g., Verapamil, Diltiazem
- Act on both vascular smooth muscle and cardiac muscle
- Used for arrhythmias and angina
They are widely prescribed in the U.S. and feature prominently in USMLE, NCLEX, NAPLEX, GPAT, and NEET-PG syllabi.
Stepwise Mechanism of Action of CCBs
- Blockade of L-type Calcium Channels
CCBs inhibit voltage-dependent L-type calcium channels located on the smooth muscle cells of blood vessels and cardiac myocytes. - Reduced Intracellular Calcium
Blocking calcium entry reduces intracellular calcium concentration, which is essential for muscle contraction. - Vasodilation (DHP CCBs)
In DHPs like Amlodipine, reduced calcium leads to arteriolar vasodilation, decreasing systemic vascular resistance and blood pressure. - Negative Inotropic and Chronotropic Effects (non-DHP CCBs)
Non-DHPs like Verapamil and Diltiazem also act on the SA and AV nodes, causing slowed heart rate (negative chronotropy) and reduced myocardial contractility (negative inotropy). - Anti-Anginal and Antiarrhythmic Effects
Non-DHP CCBs help in rate control of arrhythmias like atrial fibrillation and reduce myocardial oxygen demand, useful in angina.
Pharmacokinetic Parameters of CCBs
| Parameter | Dihydropyridines (e.g., Amlodipine) | Non-DHPs (e.g., Verapamil, Diltiazem) |
|---|---|---|
| Bioavailability | 60–90% | 20–40% |
| Half-life | Amlodipine: ~30–50 hrs | Verapamil: ~4–6 hrs; Diltiazem: ~3–5 hrs |
| Onset of Action | Gradual (2–4 hrs) | Fast (within 1 hr) |
| Metabolism | Hepatic (CYP3A4) | Hepatic |
| Excretion | Renal and fecal | Renal and fecal |
Clinical Uses of CCBs
Dihydropyridines (Amlodipine, Nifedipine):
- Hypertension
- Vasospastic (Prinzmetal) angina
- Raynaud’s phenomenon
Non-DHPs (Verapamil, Diltiazem):
- Supraventricular arrhythmias (AF, atrial flutter)
- Angina pectoris
- Hypertension (as add-on therapy)
- Migraine prophylaxis (Verapamil)
Adverse Effects of CCBs
Dihydropyridines:
- Peripheral edema
- Reflex tachycardia
- Flushing, headache, dizziness
- Gingival hyperplasia (long-term)
Non-Dihydropyridines:
- Bradycardia
- AV block
- Constipation (especially Verapamil)
- Exacerbation of heart failure (avoid in HFrEF)
Comparative Analysis: DHP vs Non-DHP CCBs
| Feature | DHP CCBs (Amlodipine) | Non-DHP CCBs (Verapamil, Diltiazem) |
|---|---|---|
| Primary Site of Action | Vascular smooth muscle | Cardiac and vascular tissues |
| Heart rate effect | Minimal | Decreased (negative chronotropy) |
| Blood pressure reduction | Strong | Moderate |
| Use in arrhythmia | No | Yes |
| Risk of bradycardia | Low | High |
Practice MCQs
Q1. What is the main site of action of calcium channel blockers?
a. Potassium channels
b. Sodium channels
c. L-type calcium channels ✅
d. Ryanodine receptors
Q2. Which subtype of CCBs primarily affects cardiac conduction?
a. Dihydropyridines
b. Non-dihydropyridines ✅
c. Loop diuretics
d. Thiazides
Q3. Which of the following is a common side effect of amlodipine?
a. Bradycardia
b. Peripheral edema ✅
c. Diarrhea
d. Hypokalemia
Q4. Which CCB should be avoided in patients with heart failure?
a. Amlodipine
b. Diltiazem
c. Verapamil ✅
d. Nifedipine
Q5. Which CCB is preferred in supraventricular tachyarrhythmias?
a. Amlodipine
b. Verapamil ✅
c. Nifedipine
d. Felodipine
Q6. Verapamil causes which of the following side effects?
a. Diuresis
b. Constipation ✅
c. Hypoglycemia
d. Reflex tachycardia
Q7. What is the mechanism behind vasodilation caused by CCBs?
a. Sodium channel inhibition
b. Potassium efflux
c. Decreased intracellular calcium ✅
d. cAMP activation
Q8. Which enzyme metabolizes most CCBs?
a. CYP2D6
b. CYP3A4 ✅
c. CYP1A2
d. CYP2C9
Q9. Gingival hyperplasia is a side effect of:
a. Beta-blockers
b. Loop diuretics
c. Amlodipine ✅
d. Diltiazem
Q10. Which of the following CCBs has the longest half-life?
a. Nifedipine
b. Verapamil
c. Amlodipine ✅
d. Diltiazem
FAQs
Q1: Can calcium channel blockers be used in heart failure?
Non-DHP CCBs should be avoided in HFrEF, but Amlodipine may be used cautiously.
Q2: What is the role of CCBs in angina?
They reduce myocardial oxygen demand and prevent coronary vasospasm, especially in Prinzmetal angina.
Q3: Are CCBs safe in pregnancy?
DHP CCBs like Nifedipine are sometimes used under specialist care; non-DHPs are generally avoided.
Q4: Can CCBs be combined with beta-blockers?
Avoid combining non-DHPs with beta-blockers due to risk of bradycardia and AV block.
References
- KD Tripathi – Essentials of Medical Pharmacology
- Goodman & Gilman – The Pharmacological Basis of Therapeutics
- Review of Pharmacology – Sparsh Gupta
- ACC/AHA Hypertension Guidelines
- NCBI: https://www.ncbi.nlm.nih.gov/books/NBK538251/

I am pursuing MBA in pharmaceutical management from NIPER Hyderabad with a strong academic record and proven success in national-level pharmacy entrance exams. I secured AIR 61 in NIPER 2024 (MS/M.Pharm) and AIR 27 in NIPER MBA, along with AIR 147 in GPAT 2024 and AIR 907 in GPAT 2023. I also achieved AIR 6 in AIIMS CRE-2025 for Drug Store Keeper and was selected as a Pharmacist (AIR 61) for ESIC. Additionally, I was the Runner-Up in Round 2 of the EY Case Study Competition.
At PharmacyFreak.com, I aim to guide future pharmacists through expert content, exam strategies, and insightful resources based on real experience and academic excellence.
Mail- harsh@pharmacyfreak.com

