Table of Contents
Introduction
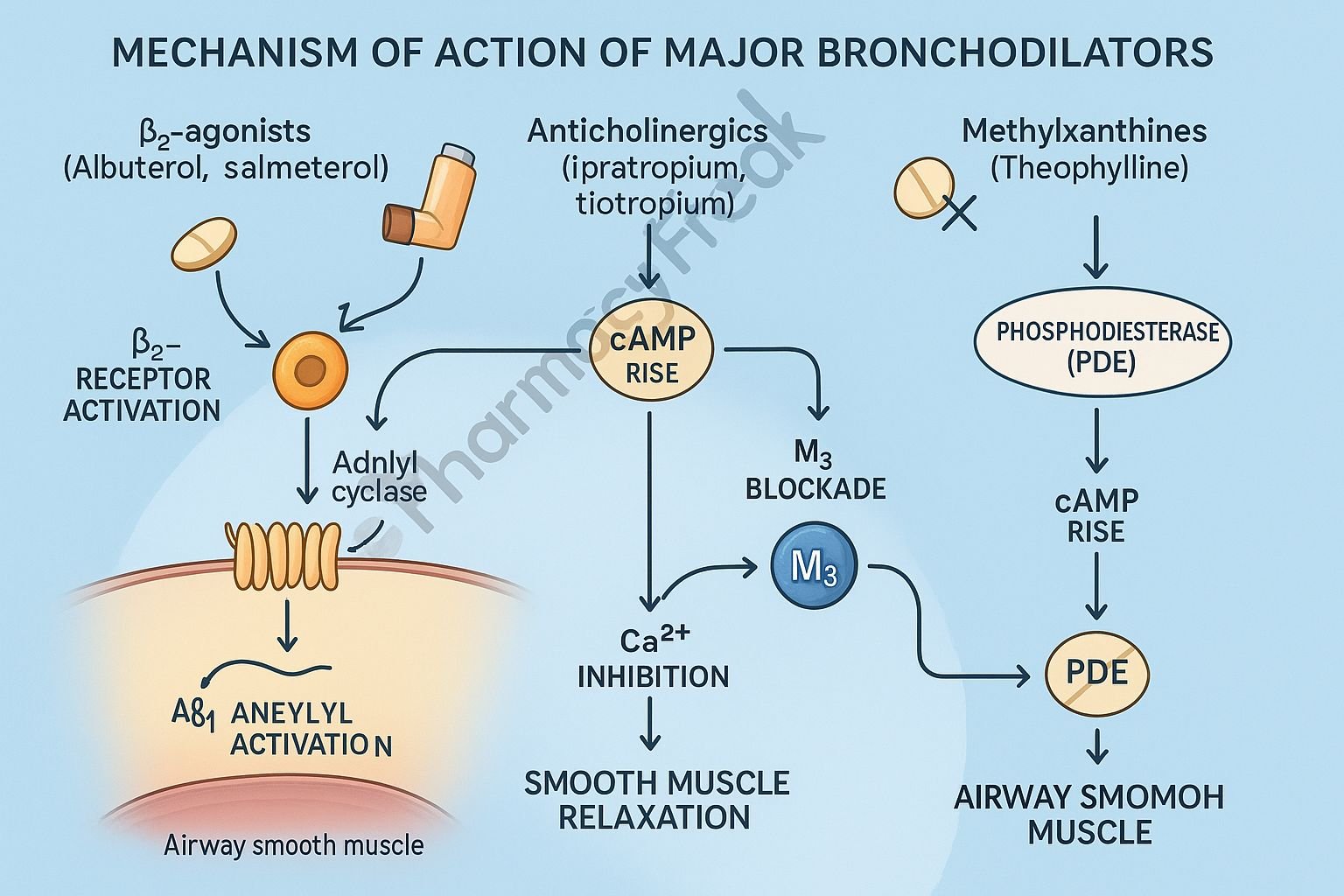
Bronchodilators are a broad class of drugs used to relieve bronchoconstriction, improve airflow, and treat respiratory disorders such as asthma, COPD, and bronchospasm. They work by relaxing airway smooth muscle, reducing airway resistance, and enhancing ventilation.
The main drug classes that act as bronchodilators include:
- Beta-2 adrenergic agonists
- Anticholinergics (muscarinic antagonists)
- Methylxanthines (e.g., theophylline)
Each class uses a different mechanism, but all ultimately lead to bronchial smooth muscle relaxation.



Mechanism of Action (Step-wise)
1. Beta-2 Adrenergic Agonists (Primary Bronchodilators)
Examples: Salbutamol, Formoterol, Salmeterol
Mechanism:
- Bind to β2 receptors on bronchial smooth muscle
- Activate adenylyl cyclase
- ↑ cAMP levels
- Activate protein kinase A (PKA)
- PKA phosphorylates smooth muscle proteins → muscle relaxation
Effects:
- Rapid bronchodilation
- ↓ Airway resistance
- Improved airflow
Short-acting (SABA): salbutamol
Long-acting (LABA): salmeterol, formoterol
2. Anticholinergics (Muscarinic Antagonists)
Examples: Ipratropium, Tiotropium
Mechanism:
- Block M3 muscarinic receptors in the airways
- Prevent parasympathetic-mediated bronchoconstriction
- ↓ IP₃ formation
- ↓ Intracellular Ca²⁺ release
- Smooth muscle relaxation
Effects:
- Bronchodilation
- ↓ Mucus secretion
- Particularly effective in COPD
3. Methylxanthines (Theophylline, Aminophylline)
Mechanism:
- Inhibit phosphodiesterase (PDE) → prevents breakdown of cAMP
- ↑ cAMP → bronchodilation
- Block adenosine receptors (which normally cause bronchoconstriction)
Effects:
- Bronchodilation
- Improved diaphragm contractility
- Anti-inflammatory effects
4. Summary of Mechanisms
| Drug Class | Mechanism | Key Effect |
|---|---|---|
| Beta-2 agonists | ↑ cAMP via β2 stimulation | Rapid bronchodilation |
| Anticholinergics | Block M3 receptors → ↓ Ca²⁺ | Sustained bronchodilation (COPD) |
| Methylxanthines | PDE inhibition → ↑ cAMP | Bronchodilation + CNS stimulation |
Pharmacokinetics
- Beta-2 agonists: Rapid onset, inhaled
- Anticholinergics: Longer duration, minimal systemic absorption
- Theophylline: Narrow therapeutic index, hepatic metabolism
Clinical Uses
- Asthma (acute + maintenance)
- COPD
- Exercise-induced bronchospasm
- Acute severe asthma (status asthmaticus)
- Bronchospasm prevention
Adverse Effects
Beta-2 agonists
- Tremors
- Tachycardia
- Hypokalemia
Anticholinergics
- Dry mouth
- Urinary retention
- Glaucoma risk (if nebulized into eyes)
Methylxanthines
- Nausea
- Arrhythmias
- Seizures (toxicity)
Contraindications
- Uncontrolled arrhythmias (β2 agonists)
- Narrow-angle glaucoma (anticholinergics)
- Epilepsy, cardiac disease (theophylline)
Comparative Analysis
| Feature | β2 Agonists | Anticholinergics | Methylxanthines |
|---|---|---|---|
| Onset | Fast | Moderate | Slow |
| Duration | Short/long | Long | Variable |
| Use | Asthma > COPD | COPD > Asthma | Add-on therapy |
| Safety | High | High | Low (toxicity) |
MCQs
1. Beta-2 agonists relax bronchial smooth muscle by:
a) Decreasing cAMP
b) Increasing cAMP
c) Blocking M3 receptors
d) Blocking PDE
Answer: b) Increasing cAMP
2. The primary receptor blocked by ipratropium is:
a) Beta-1
b) Beta-2
c) M3
d) M2
Answer: c) M3
3. Theophylline acts mainly by:
a) Stimulating M3 receptors
b) Inhibiting PDE
c) Blocking β2 receptors
d) Decreasing cAMP
Answer: b) Inhibiting PDE
4. Long-acting anticholinergic preferred in COPD:
a) Salbutamol
b) Tiotropium
c) Salmeterol
d) Theophylline
Answer: b) Tiotropium
5. β2 agonists cause tremors because of stimulation of:
a) Skeletal muscle β2 receptors
b) Cardiac β1 receptors
c) CNS dopamine receptors
d) NMDA receptors
Answer: a) Skeletal muscle β2 receptors
FAQs
Q1. Which bronchodilator works the fastest?
Short-acting β2 agonists (SABA) like salbutamol.
Q2. Which bronchodilator is best for COPD?
Long-acting anticholinergics like tiotropium.
Q3. Why is theophylline rarely used?
Narrow therapeutic window and risk of toxicity.
Q4. Can bronchodilators be combined?
Yes—β2 agonists + anticholinergics is a common combination.
Q5. Do bronchodilators reduce inflammation?
Only mildly (theophylline); steroids are required for anti-inflammatory action.
References
Goodman & Gilman’s Pharmacological Basis of Therapeutics
https://accesspharmacy.mhmedical.com/book.aspx?bookid=2189
Katzung: Basic and Clinical Pharmacology
https://accessmedicine.mhmedical.com/book.aspx?bookid=2464
Tripathi: Essentials of Medical Pharmacology
https://jaypeebrothers.com/
Harrison’s Principles of Internal Medicine
https://accessmedicine.mhmedical.com/book.aspx?bookid=2129

I am pursuing MBA in pharmaceutical management from NIPER Hyderabad with a strong academic record and proven success in national-level pharmacy entrance exams. I secured AIR 61 in NIPER 2024 (MS/M.Pharm) and AIR 27 in NIPER MBA, along with AIR 147 in GPAT 2024 and AIR 907 in GPAT 2023. I also achieved AIR 6 in AIIMS CRE-2025 for Drug Store Keeper and was selected as a Pharmacist (AIR 61) for ESIC. Additionally, I was the Runner-Up in Round 2 of the EY Case Study Competition.
At PharmacyFreak.com, I aim to guide future pharmacists through expert content, exam strategies, and insightful resources based on real experience and academic excellence.
Mail- harsh@pharmacyfreak.com