Table of Contents
Introduction
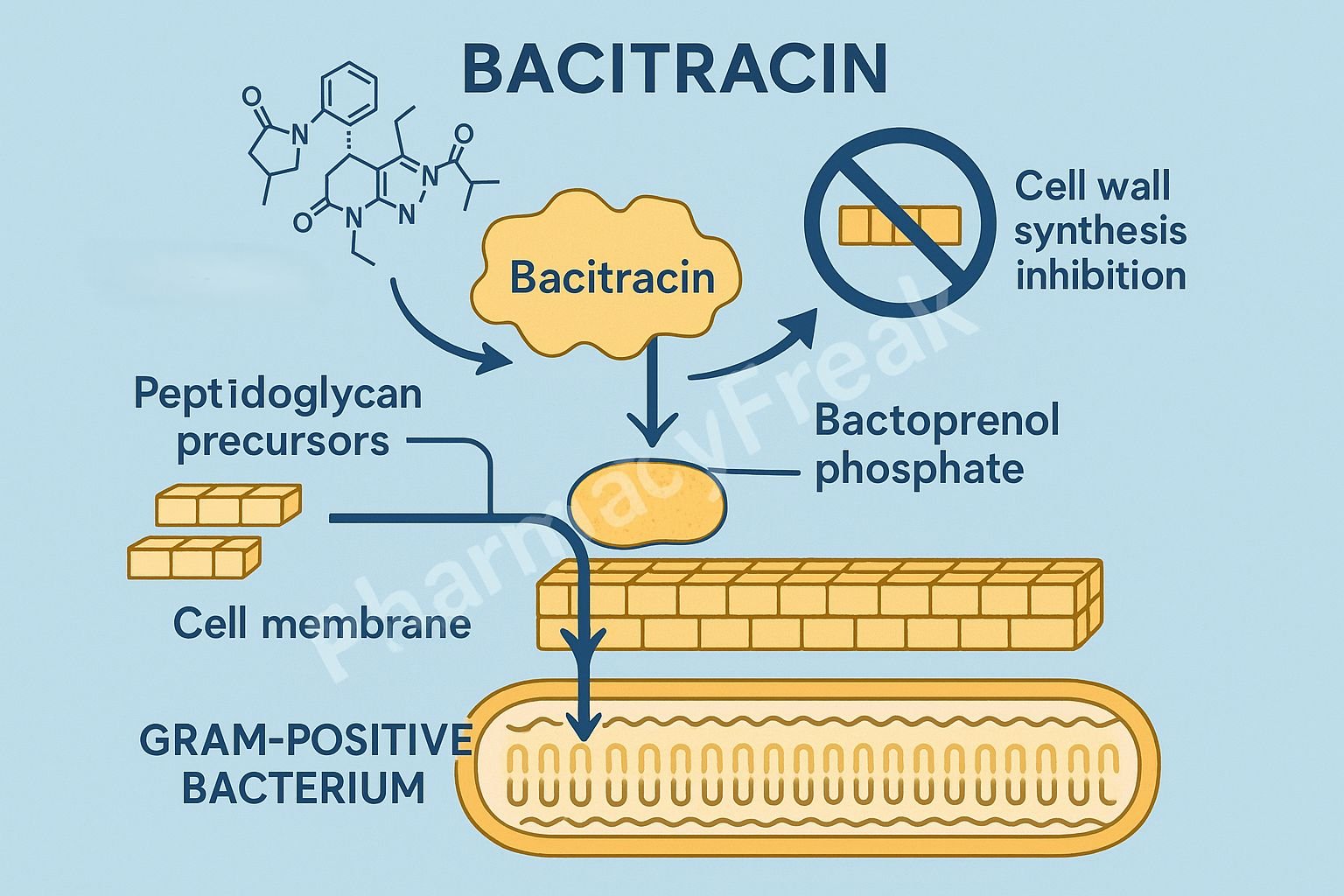
Bacitracin is a polypeptide antibiotic primarily used topically for the treatment and prevention of gram-positive bacterial infections. It is commonly found in combination ointments such as bacitracin-neomycin-polymyxin B (triple antibiotic ointment).
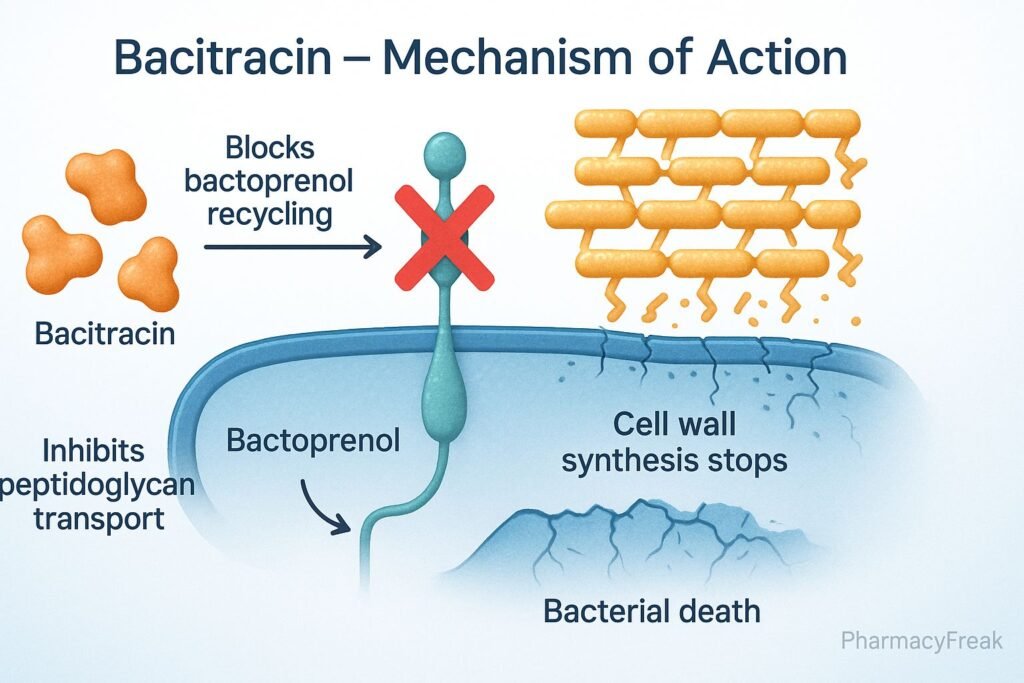
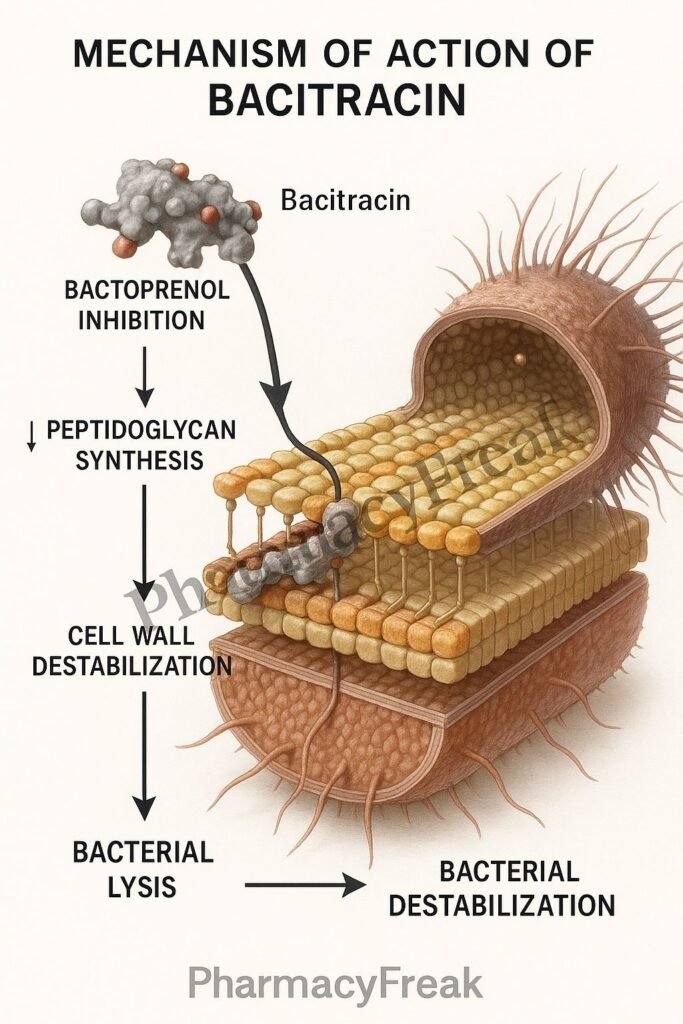
Mechanism of Action of Bacitracin involves inhibition of bacterial cell wall synthesis by interfering with the dephosphorylation of the lipid carrier (bactoprenol phosphate) responsible for peptidoglycan precursor transport. This blocks cell wall formation, leading to bacterial cell lysis.
Bacitracin is bactericidal against actively dividing bacteria and exhibits strong activity against Staphylococcus and Streptococcus species.
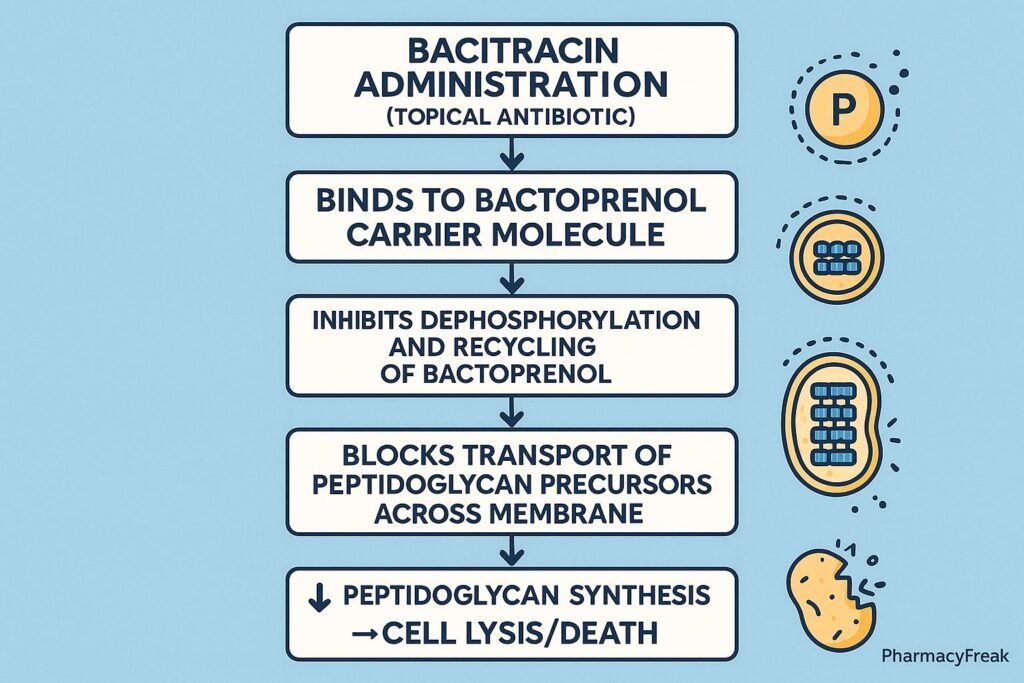
Mechanism of Action (Step-wise)
1. Target: Bacterial Cell Wall Synthesis
- Mechanism:
- Bacterial cell walls are composed of peptidoglycan, a polymer of N-acetylglucosamine (NAG) and N-acetylmuramic acid (NAM) cross-linked by peptide chains.
- The synthesis of peptidoglycan involves a lipid carrier molecule, bactoprenol, that shuttles precursors from the cytoplasm across the cell membrane.
2. Inhibition of Bactoprenol Dephosphorylation
- Mechanism:
- Bacitracin binds to bactoprenol pyrophosphate (C55-isoprenyl pyrophosphate), the carrier responsible for transporting peptidoglycan precursors through the cell membrane.
- It prevents the dephosphorylation of this molecule to its active form, bactoprenol phosphate, which is required for recycling and continued peptidoglycan synthesis.
- Effect:
- Peptidoglycan precursors accumulate inside the cytoplasm.
- Cell wall synthesis is halted.
3. Resulting Disruption of Cell Wall Integrity
- Mechanism:
- Without new peptidoglycan synthesis, the bacterial cell wall becomes weak and unable to maintain osmotic stability.
- This results in cell lysis due to osmotic pressure.
- Effect:
- Bactericidal effect on growing bacteria.
4. Stepwise Summary
| Step | Normal Process | Bacitracin Action | Result |
|---|---|---|---|
| 1 | Bactoprenol transports peptidoglycan precursors across the membrane | Binds bactoprenol pyrophosphate | Prevents dephosphorylation |
| 2 | Bactoprenol recycled to active form | Inhibited | Stops precursor transport |
| 3 | Peptidoglycan synthesized | Blocked | Weak cell wall → Lysis |
Spectrum of Activity
| Type | Bacteria Affected | Examples |
|---|---|---|
| Gram-positive (Highly Sensitive) | Staphylococci, Streptococci, Clostridia, Corynebacteria | Staphylococcus aureus, Streptococcus pyogenes |
| Gram-negative (Resistant) | Outer membrane prevents access to target | E. coli, Pseudomonas aeruginosa |
Pharmacokinetics
- Absorption: Poor from the gastrointestinal tract → unsuitable for systemic use.
- Administration: Topical application only; rarely used parenterally due to nephrotoxicity.
- Distribution: Localized at the site of application.
- Excretion: Renal (when given systemically).
Clinical Uses
- Topical:
- Skin infections (impetigo, minor burns, cuts, abrasions).
- Wound and postoperative infection prophylaxis.
- Ophthalmic:
- Eye ointments for conjunctivitis and blepharitis.
- ENT Infections:
- Topical use in nasal or ear preparations.
- Systemic Use:
- Rarely used; only in life-threatening infections with highly resistant Staphylococcus when alternatives fail (due to nephrotoxicity).
Adverse Effects
- Topical: Contact dermatitis, rash, or allergic reactions.
- Systemic (rare): Severe nephrotoxicity and neurotoxicity (limits systemic use).
- Hypersensitivity: More common when combined with neomycin or polymyxin in topical products.
Mechanism Comparison with Other Cell Wall Inhibitors
| Drug Class | Target | Mechanism | Example |
|---|---|---|---|
| β-Lactams | Transpeptidase enzyme | Inhibit cross-linking of peptidoglycan chains | Penicillin |
| Glycopeptides | D-Ala–D-Ala terminus | Block peptidoglycan elongation | Vancomycin |
| Polypeptides (Bacitracin) | Bactoprenol recycling | Inhibit lipid carrier regeneration | Bacitracin |
MCQs
1. Bacitracin inhibits bacterial cell wall synthesis by:
a) Blocking transpeptidase enzyme
b) Preventing bactoprenol dephosphorylation
c) Inhibiting D-Ala–D-Ala linkage
d) Blocking β-lactamase
Answer: b) Preventing bactoprenol dephosphorylation
2. Bacitracin is primarily active against:
a) Gram-negative bacteria
b) Gram-positive bacteria
c) Mycobacteria
d) Anaerobes only
Answer: b) Gram-positive bacteria
3. The primary use of bacitracin is:
a) Oral therapy for systemic infections
b) Intravenous antibiotic
c) Topical application for skin infections
d) Antifungal prophylaxis
Answer: c) Topical application for skin infections
4. Systemic use of bacitracin is limited because of:
a) Hepatotoxicity
b) Nephrotoxicity
c) Ototoxicity
d) Bone marrow suppression
Answer: b) Nephrotoxicity
5. Bactoprenol is involved in:
a) Protein synthesis
b) Peptidoglycan transport across the cell membrane
c) RNA replication
d) Lipid oxidation
Answer: b) Peptidoglycan transport across the cell membrane
6. Bacitracin is classified as a:
a) β-Lactam antibiotic
b) Polypeptide antibiotic
c) Macrolide
d) Glycopeptide
Answer: b) Polypeptide antibiotic
7. Which combination contains bacitracin as a topical agent?
a) Neosporin (Triple antibiotic ointment)
b) Augmentin
c) Bactrim
d) Ciproxin
Answer: a) Neosporin (Triple antibiotic ointment)
8. Bacitracin differs from penicillin because it:
a) Acts on ribosomes
b) Inhibits lipid carrier recycling
c) Blocks β-lactamase
d) Affects nucleic acid synthesis
Answer: b) Inhibits lipid carrier recycling
9. Bacitracin cannot be used orally because:
a) It is inactivated by gastric acid
b) Poor absorption from GIT
c) Causes diarrhea
d) High hepatic metabolism
Answer: b) Poor absorption from GIT
10. The lipid carrier targeted by bacitracin is:
a) Bactoprenol
b) Dolichol
c) Phosphatidylserine
d) Cardiolipin
Answer: a) Bactoprenol
FAQs
Q1. What is the main difference between bacitracin and β-lactam antibiotics?
Bacitracin inhibits the early stage of peptidoglycan synthesis (precursor transport), while β-lactams inhibit the final cross-linking step.
Q2. Why is bacitracin not used systemically?
Because it causes severe nephrotoxicity, limiting its use to topical applications only.
Q3. Can bacitracin be used for gram-negative infections?
No, it is ineffective against gram-negative bacteria due to poor penetration through their outer membrane.
Q4. How is bacitracin commonly administered?
Topically, in ointments or creams, often combined with neomycin and polymyxin B.
Q5. Is bacitracin bacteriostatic or bactericidal?
Bactericidal, but only against actively dividing gram-positive bacteria.
References
- Goodman & Gilman’s The Pharmacological Basis of Therapeutics
- Katzung BG. Basic and Clinical Pharmacology
- Tripathi KD. Essentials of Medical Pharmacology
- Harrison’s Principles of Internal Medicine
Related Internal Links

I am pursuing MBA in pharmaceutical management from NIPER Hyderabad with a strong academic record and proven success in national-level pharmacy entrance exams. I secured AIR 61 in NIPER 2024 (MS/M.Pharm) and AIR 27 in NIPER MBA, along with AIR 147 in GPAT 2024 and AIR 907 in GPAT 2023. I also achieved AIR 6 in AIIMS CRE-2025 for Drug Store Keeper and was selected as a Pharmacist (AIR 61) for ESIC. Additionally, I was the Runner-Up in Round 2 of the EY Case Study Competition.
At PharmacyFreak.com, I aim to guide future pharmacists through expert content, exam strategies, and insightful resources based on real experience and academic excellence.
Mail- harsh@pharmacyfreak.com
it is very supportive
thanks 🙏