Table of Contents
Introduction
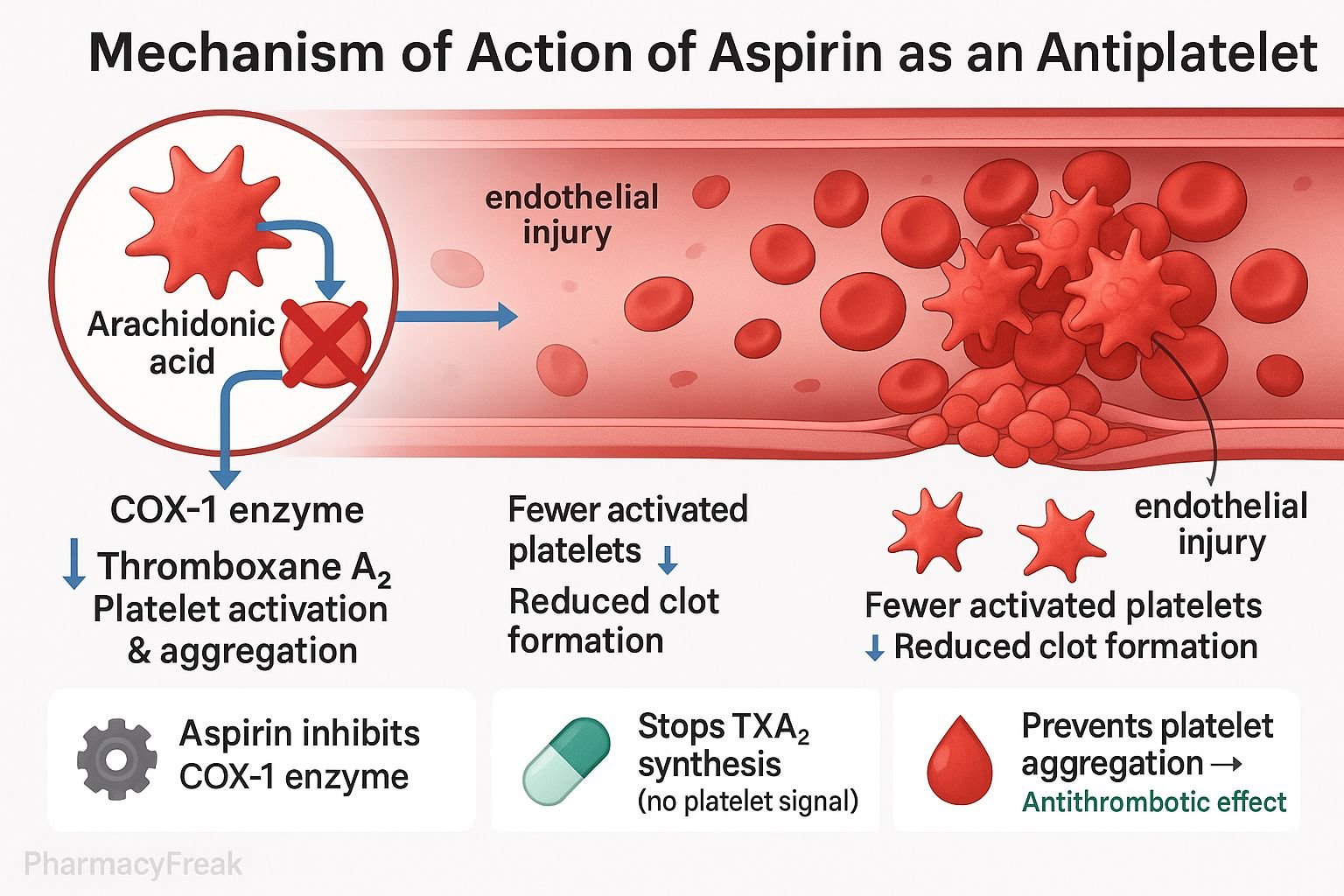
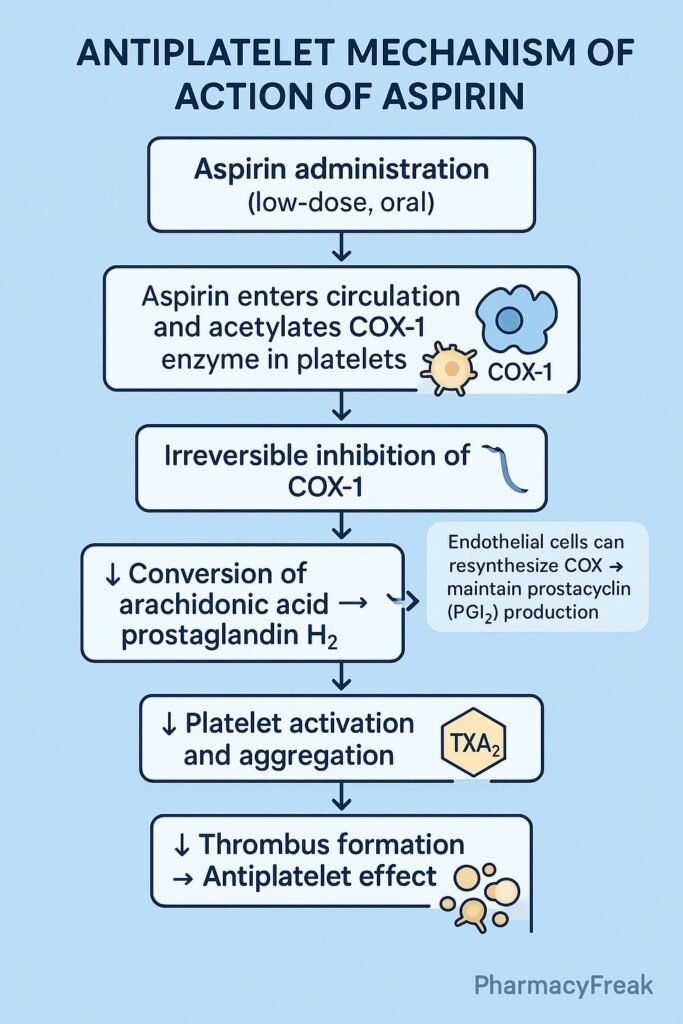
Aspirin (Acetylsalicylic Acid, ASA) is the most widely used antiplatelet agent in clinical medicine. Its antiplatelet mechanism of action is distinct because it causes irreversible inhibition of platelet cyclooxygenase-1 (COX-1), blocking the formation of thromboxane A₂ (TXA₂) — a potent inducer of platelet aggregation and vasoconstriction.
Low-dose aspirin (typically 75–150 mg/day) preferentially inhibits platelet COX-1 without significantly affecting endothelial prostacyclin (PGI₂) production, thereby preventing arterial thrombosis in conditions like myocardial infarction, ischemic stroke, and unstable angina.
Mechanism of Action (Step-wise)
1. Inhibition of Cyclooxygenase-1 (COX-1) in Platelets
- Mechanism:
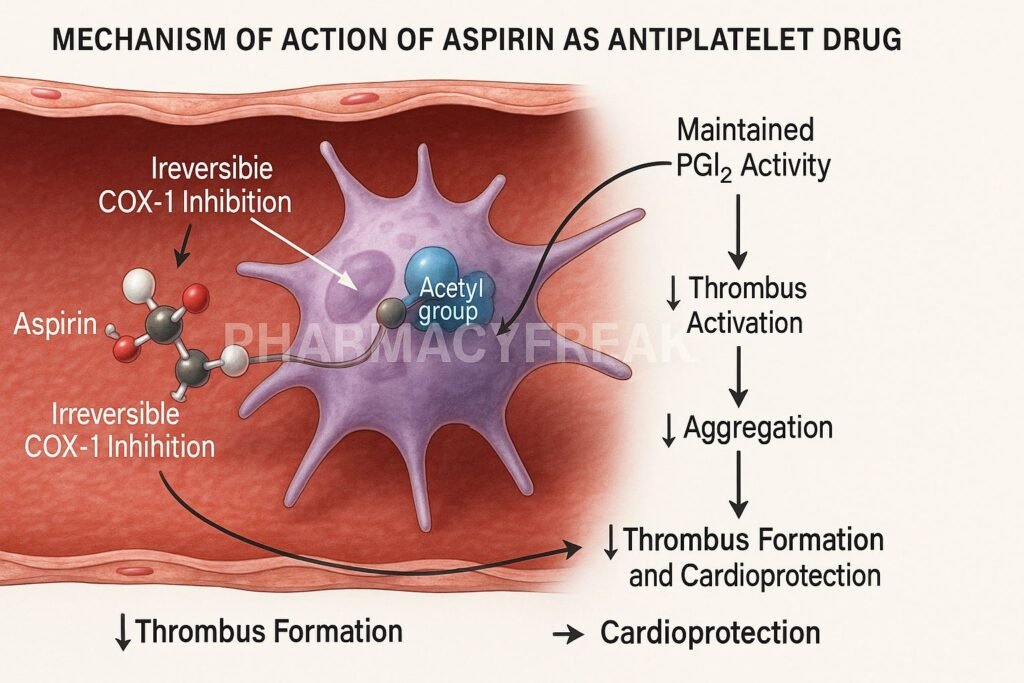
- Aspirin acetylates a serine residue (Ser530) on the active site of COX-1 enzyme in platelets.
- This irreversibly inhibits COX-1, preventing the conversion of arachidonic acid to prostaglandin H₂ (PGH₂).
- As a result, synthesis of thromboxane A₂ (TXA₂) — a key mediator of platelet activation and aggregation — is blocked.
2. Irreversible Effect on Platelets
- Mechanism:
- Platelets are anucleate cells (they lack nuclei), hence they cannot synthesize new COX-1 enzymes once inhibited.
- Therefore, the effect of aspirin persists for the entire lifespan of platelets (7–10 days), even after aspirin is cleared from circulation.
- Outcome:
- Sustained reduction in TXA₂ levels → Reduced platelet activation → Reduced clot formation.
3. Selective Action at Low Doses
- Mechanism:
- Low-dose aspirin (75–150 mg/day) primarily affects platelet COX-1 in the portal circulation, before first-pass hepatic metabolism.
- Endothelial cells, however, can regenerate COX enzymes and continue producing prostacyclin (PGI₂) — a vasodilator and inhibitor of platelet aggregation.
- Effect:
- The balance shifts toward antithrombotic activity: ↓ TXA₂ (prothrombotic) and maintained PGI₂ (antithrombotic).
4. Final Biological Effect
| Pathway | Normal Function | Effect of Aspirin |
|---|---|---|
| Arachidonic acid → COX-1 → TXA₂ | Promotes platelet aggregation & vasoconstriction | Inhibited |
| Endothelial COX → PGI₂ | Inhibits aggregation & causes vasodilation | Largely preserved |
| Net Effect | Balance between TXA₂ and PGI₂ | Shift toward vasodilation & reduced aggregation |
5. Summary of Pharmacodynamic Actions
- ↓ Thromboxane A₂ synthesis → ↓ Platelet aggregation
- Irreversible inhibition of COX-1 → Long-lasting effect
- Preservation of PGI₂ → Maintained vasodilatory tone
- Clinical result: Prevention of arterial thrombosis (not venous, where anticoagulants are used).
Clinical Uses
- Secondary prevention of myocardial infarction and ischemic stroke.
- After percutaneous coronary intervention (PCI) with stenting (as part of dual antiplatelet therapy).
- Unstable angina or acute coronary syndromes (ACS).
- Peripheral arterial disease and transient ischemic attack (TIA) prophylaxis.
Pharmacokinetics
- Absorption: Rapid oral absorption from the stomach and upper intestine.
- Onset of Action: Within 30–60 minutes.
- Half-Life: Short (~15–20 minutes), but platelet effect lasts 7–10 days.
- Metabolism: Deacetylated to salicylic acid in the liver.
- Elimination: Renal.
Adverse Effects
- Bleeding: Especially gastrointestinal or intracranial hemorrhage (due to inhibited platelet function).
- Gastrointestinal irritation and ulceration: Due to inhibition of prostaglandin synthesis in gastric mucosa.
- Hypersensitivity reactions: Bronchospasm, aspirin-induced asthma.
- Reye’s syndrome: Avoid in children with viral infections.
Comparative Note
| Feature | Aspirin | Clopidogrel | Ticagrelor |
|---|---|---|---|
| Target | COX-1 enzyme | P2Y₁₂ receptor | P2Y₁₂ receptor |
| Action Type | Irreversible | Irreversible | Reversible |
| Duration | 7–10 days | 7–10 days | 2–3 days |
| Key Use | Primary & secondary prevention of arterial thrombosis | Dual therapy with aspirin | DAPT (short-term use) |
MCQs
1. Aspirin inhibits platelet aggregation by blocking:
a) COX-1 enzyme
b) COX-2 enzyme
c) P2Y₁₂ receptor
d) GPIIb/IIIa receptor
Answer: a) COX-1 enzyme
2. The effect of aspirin on platelets lasts for:
a) 24 hours
b) 3 days
c) 7–10 days
d) Until drug is metabolized
Answer: c) 7–10 days
3. Which product of COX-1 inhibition mediates platelet aggregation?
a) Prostaglandin E₂
b) Thromboxane A₂
c) Prostacyclin
d) Leukotriene B₄
Answer: b) Thromboxane A₂
4. Low-dose aspirin spares which beneficial mediator?
a) TXA₂
b) PGI₂ (prostacyclin)
c) PGE₂
d) Leukotriene
Answer: b) PGI₂ (prostacyclin)
5. Why is aspirin used in myocardial infarction?
a) It increases fibrin formation
b) It inhibits platelet aggregation
c) It enhances thrombin activation
d) It inhibits calcium entry into platelets
Answer: b) It inhibits platelet aggregation
6. Why does aspirin have a prolonged antiplatelet effect?
a) It binds reversibly to COX-1
b) It irreversibly inhibits COX-1 in anucleate platelets
c) It blocks thrombin receptors
d) It inhibits fibrinogen
Answer: b) It irreversibly inhibits COX-1 in anucleate platelets
7. What is the primary dose range for antiplatelet activity?
a) 50–150 mg/day
b) 500–1000 mg/day
c) 2 g/day
d) 4 g/day
Answer: a) 50–150 mg/day
8. Which of the following is a contraindication for aspirin use?
a) History of myocardial infarction
b) Peptic ulcer disease
c) Hypertension
d) Diabetes mellitus
Answer: b) Peptic ulcer disease
FAQs
Q1. Why is aspirin used in low doses for antiplatelet therapy?
Because low doses selectively inhibit platelet COX-1 without significantly affecting endothelial COX-2, preserving prostacyclin.
Q2. Why does aspirin’s antiplatelet effect last longer than its half-life?
Because COX-1 inhibition in platelets is irreversible, and platelets cannot synthesize new enzymes.
Q3. Can aspirin be combined with other antiplatelet agents?
Yes, in Dual Antiplatelet Therapy (DAPT), aspirin is combined with clopidogrel or ticagrelor for enhanced protection after PCI or ACS.
Q4. What happens if aspirin is stopped suddenly after long-term use?
Platelet function returns gradually as new platelets are produced over 7–10 days, which may increase thrombotic risk temporarily.
Q5. How does aspirin differ from other NSAIDs in platelet inhibition?
Aspirin causes irreversible COX-1 inhibition, whereas other NSAIDs (like ibuprofen) cause reversible inhibition and shorter effects.
References
- Goodman & Gilman’s The Pharmacological Basis of Therapeutics
- Katzung BG. Basic and Clinical Pharmacology
- Tripathi KD. Essentials of Medical Pharmacology
- Harrison’s Principles of Internal Medicine
Related Internal Links

I am pursuing MBA in pharmaceutical management from NIPER Hyderabad with a strong academic record and proven success in national-level pharmacy entrance exams. I secured AIR 61 in NIPER 2024 (MS/M.Pharm) and AIR 27 in NIPER MBA, along with AIR 147 in GPAT 2024 and AIR 907 in GPAT 2023. I also achieved AIR 6 in AIIMS CRE-2025 for Drug Store Keeper and was selected as a Pharmacist (AIR 61) for ESIC. Additionally, I was the Runner-Up in Round 2 of the EY Case Study Competition.
At PharmacyFreak.com, I aim to guide future pharmacists through expert content, exam strategies, and insightful resources based on real experience and academic excellence.
Mail- harsh@pharmacyfreak.com