Table of Contents
Introduction
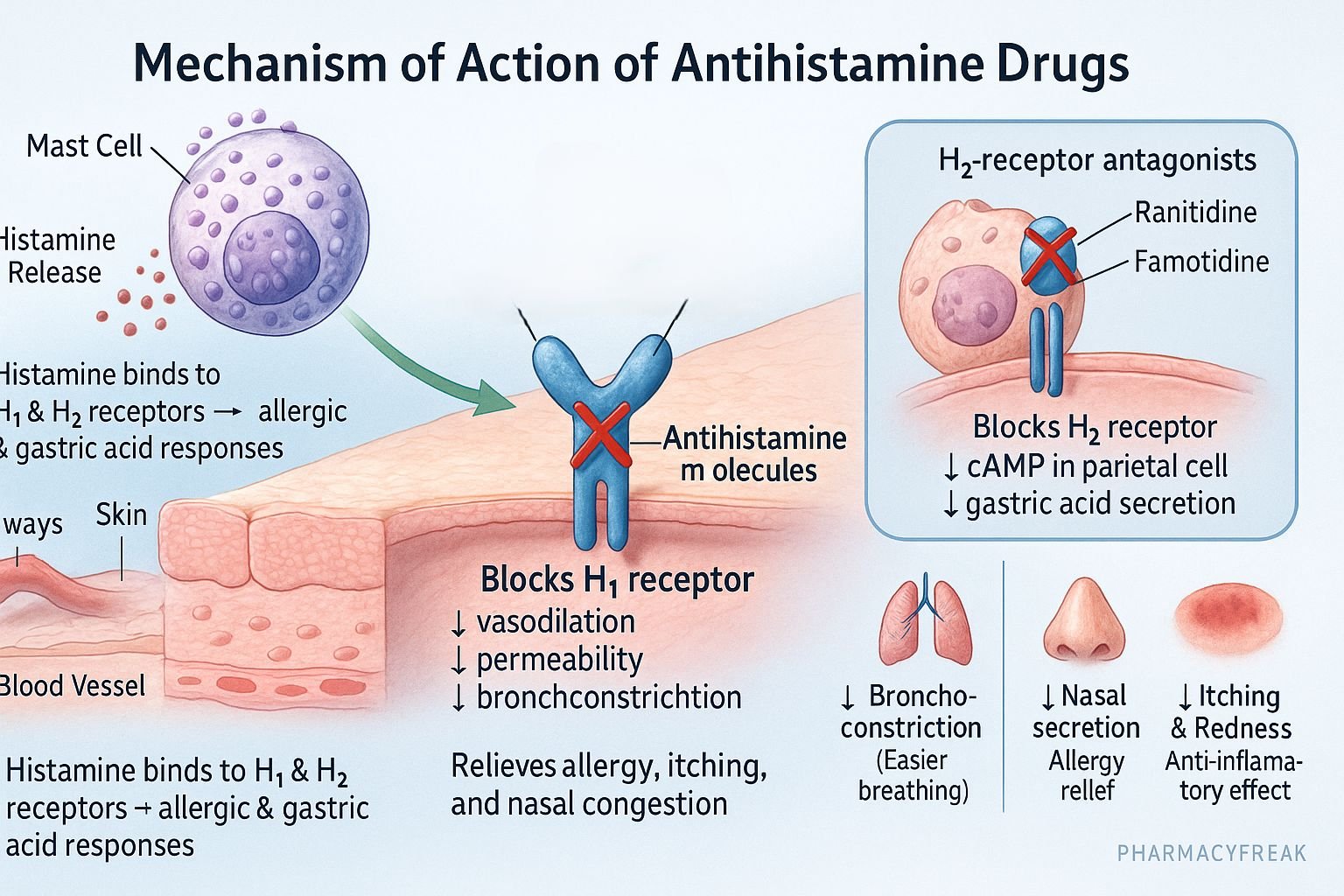
Antihistamines are pharmacological agents that counteract the effects of histamine, a biogenic amine released during allergic and inflammatory responses. Mechanism of Action of Antihistamine Drugs involves competitive antagonism at histamine H₁ or H₂ receptors, thereby reducing vasodilation, vascular permeability, smooth muscle contraction, and gastric acid secretion. Clinically, antihistamines are used in the management of allergic rhinitis, urticaria, anaphylaxis, motion sickness, insomnia, and peptic ulcer disease.

Mechanism of Action (Step-wise)
Antihistamines act by blocking histamine receptors in various tissues without affecting histamine release from mast cells or basophils.
1. Histamine Receptors Overview
- H₁ Receptors: Found in smooth muscle, endothelium, and CNS. Responsible for allergic and inflammatory reactions (vasodilation, bronchoconstriction, itching).
- H₂ Receptors: Located in gastric parietal cells. Regulate acid secretion.
- H₃ Receptors: Presynaptic autoreceptors regulating histamine release (mainly CNS).
- H₄ Receptors: Involved in immune cell chemotaxis and inflammation.
2. H₁ Receptor Antagonists (Classical Antihistamines)
- Mechanism:
- Act as inverse agonists or competitive antagonists at H₁ receptors, stabilizing them in an inactive state.
- Prevent histamine-induced vasodilation, increased vascular permeability, bronchoconstriction, and sensory nerve stimulation (itching).
- Effect:
- Decrease in allergic symptoms such as itching, sneezing, rhinorrhea, and swelling.
- Secondary effects include sedation (first-generation agents) and anticholinergic activity.
- Examples:
- First-generation: Diphenhydramine, Chlorpheniramine, Promethazine, Hydroxyzine.
- Second-generation: Cetirizine, Loratadine, Fexofenadine, Desloratadine.
- Clinical Uses: Allergic rhinitis, urticaria, conjunctivitis, anaphylaxis (adjunct), motion sickness, insomnia.
3. H₂ Receptor Antagonists
- Mechanism:
- Competitively inhibit histamine binding at H₂ receptors on gastric parietal cells.
- This suppresses both basal and stimulated gastric acid secretion.
- Effect: Reduced gastric acidity → healing of ulcers and prevention of acid reflux.
- Examples: Ranitidine, Famotidine, Nizatidine, Cimetidine.
- Clinical Uses: Peptic ulcer disease, GERD, Zollinger–Ellison syndrome.
4. Pharmacological Actions (H₁ Blockers)
| System | Effect of H₁ Blockers |
|---|---|
| Vascular | ↓ Capillary permeability and vasodilation |
| Respiratory | ↓ Bronchoconstriction |
| CNS | Sedation (first-gen only) |
| GI Tract | Mild antispasmodic action |
| Eye & Skin | ↓ Itching, tearing, redness |
| Autonomic | Antimuscarinic → dry mouth, urinary retention (first-gen) |

Pharmacokinetics
- Absorption: Rapid oral absorption.
- Distribution: Lipid-soluble; first-gen drugs cross blood-brain barrier.
- Metabolism: Hepatic (CYP450 enzymes).
- Excretion: Renal, mainly as metabolites.
- Onset: 15–60 minutes (H₁ blockers); 1–2 hours (H₂ blockers).
Adverse Effects
- First-generation H₁ blockers: Sedation, dizziness, dry mouth, urinary retention, blurred vision.
- Second-generation H₁ blockers: Minimal sedation and anticholinergic effects.
- H₂ blockers: Diarrhea, headache, rash; Cimetidine may cause gynecomastia and CYP inhibition.
- Contraindications: Narrow-angle glaucoma, prostatic hypertrophy, and concurrent CNS depressant use (for sedating antihistamines).
Comparative Analysis
| Parameter | H₁ Antagonists | H₂ Antagonists |
|---|---|---|
| Main Site of Action | Respiratory & vascular tissues | Gastric parietal cells |
| Primary Function | Anti-allergic | Anti-secretory |
| Examples | Diphenhydramine, Loratadine | Ranitidine, Famotidine |
| CNS Effects | Sedation (1st gen) | None |
| Adverse Effects | Drowsiness, dry mouth | Headache, diarrhea, gynecomastia (Cimetidine) |
| Clinical Uses | Allergy, rhinitis, urticaria | Peptic ulcer, GERD |
MCQs
1. Antihistamines act primarily by:
a) Blocking histamine release
b) Blocking histamine receptors
c) Inhibiting mast cell degranulation
d) Destroying histamine
Answer: b) Blocking histamine receptors
2. H₁ receptor blockade results in:
a) Decreased gastric acid secretion
b) Decreased allergic symptoms
c) Increased vascular permeability
d) Increased heart rate
Answer: b) Decreased allergic symptoms
3. H₂ blockers are used to treat:
a) Allergic rhinitis
b) Peptic ulcer disease
c) Asthma
d) Motion sickness
Answer: b) Peptic ulcer disease
4. Which antihistamine causes least sedation?
a) Diphenhydramine
b) Chlorpheniramine
c) Cetirizine
d) Promethazine
Answer: c) Cetirizine
5. The enzyme inhibited by cimetidine is:
a) CYP450
b) MAO
c) COMT
d) Acetylcholinesterase
Answer: a) CYP450
6. The receptor subtype involved in gastric acid secretion is:
a) H₁
b) H₂
c) H₃
d) H₄
Answer: b) H₂
7. The first-generation antihistamines cause sedation because:
a) They block dopamine receptors
b) They cross the blood-brain barrier
c) They block serotonin
d) They have poor oral absorption
Answer: b) They cross the blood-brain barrier
8. Which drug is an H₂ receptor blocker?
a) Ranitidine
b) Loratadine
c) Cetirizine
d) Promethazine
Answer: a) Ranitidine
9. Which drug acts as an inverse agonist at the H₁ receptor?
a) Diphenhydramine
b) Famotidine
c) Omeprazole
d) Fexofenadine
Answer: a) Diphenhydramine
10. Which antihistamine has anticholinergic properties?
a) Promethazine
b) Fexofenadine
c) Loratadine
d) Cetirizine
Answer: a) Promethazine
FAQs
Q1. What is the difference between H₁ and H₂ antihistamines?
H₁ blockers treat allergic conditions, while H₂ blockers reduce gastric acid secretion.
Q2. Why do first-generation antihistamines cause drowsiness?
Because they cross the blood-brain barrier and block central H₁ receptors.
Q3. Can antihistamines be used for motion sickness?
Yes, first-generation H₁ blockers such as Diphenhydramine and Promethazine are effective.
Q4. What is the safest antihistamine for long-term allergy treatment?
Second-generation agents like Loratadine or Fexofenadine due to minimal CNS effects.
Q5. Why is cimetidine less preferred among H₂ blockers?
It causes drug interactions by inhibiting CYP450 enzymes and can lead to gynecomastia.
Q6. Do antihistamines block histamine release from mast cells?
No, they only block receptor binding, not histamine release.
References
- Goodman & Gilman’s The Pharmacological Basis of Therapeutics
- Katzung’s Basic and Clinical Pharmacology
- Tripathi KD, Essentials of Medical Pharmacology
- Rang & Dale’s Pharmacology

I am pursuing MBA in pharmaceutical management from NIPER Hyderabad with a strong academic record and proven success in national-level pharmacy entrance exams. I secured AIR 61 in NIPER 2024 (MS/M.Pharm) and AIR 27 in NIPER MBA, along with AIR 147 in GPAT 2024 and AIR 907 in GPAT 2023. I also achieved AIR 6 in AIIMS CRE-2025 for Drug Store Keeper and was selected as a Pharmacist (AIR 61) for ESIC. Additionally, I was the Runner-Up in Round 2 of the EY Case Study Competition.
At PharmacyFreak.com, I aim to guide future pharmacists through expert content, exam strategies, and insightful resources based on real experience and academic excellence.
Mail- harsh@pharmacyfreak.com