Table of Contents
Introduction
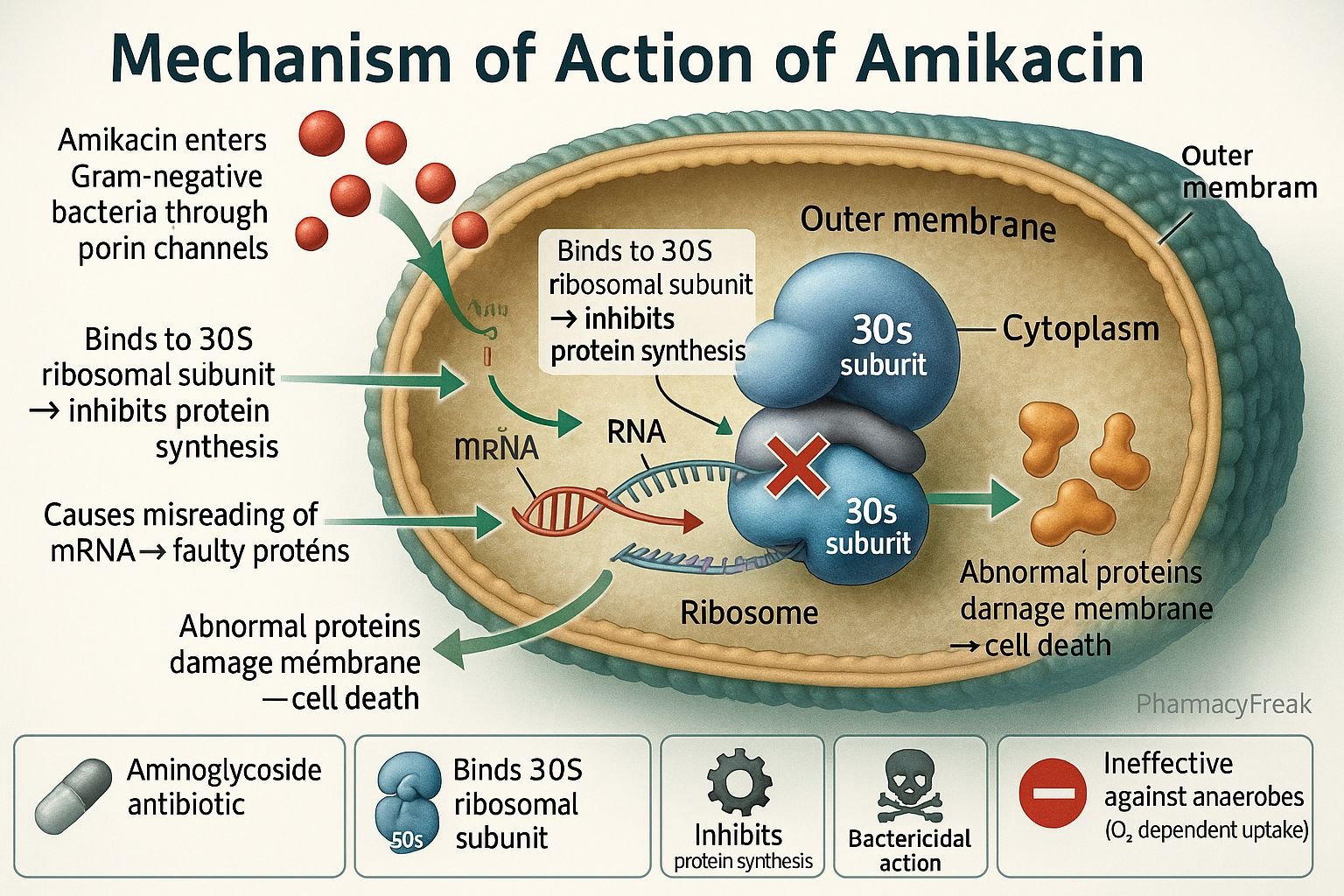
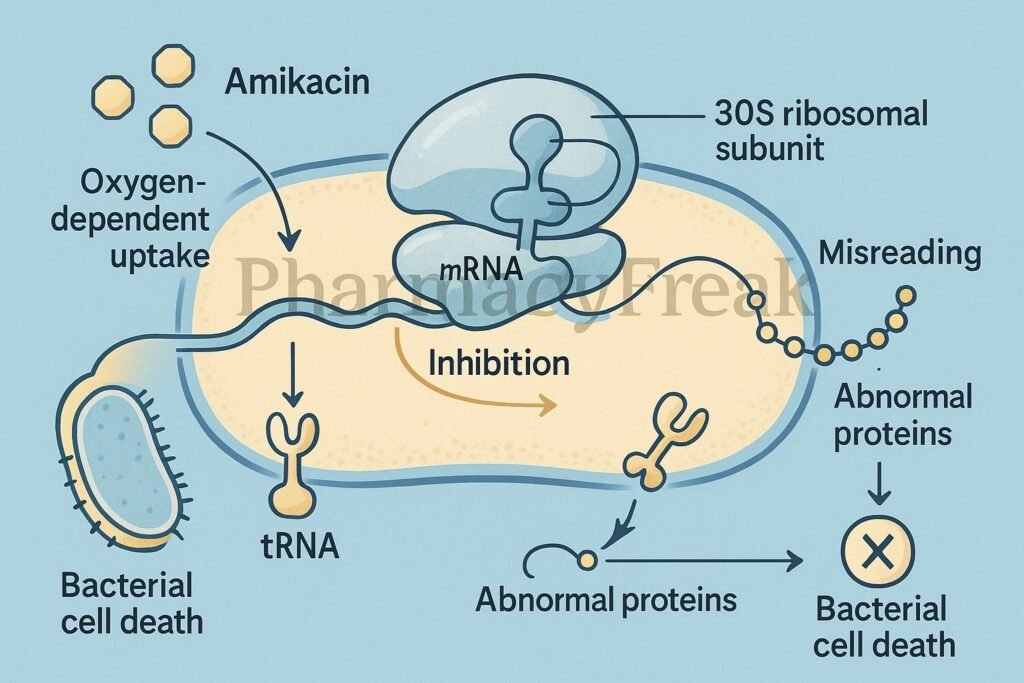
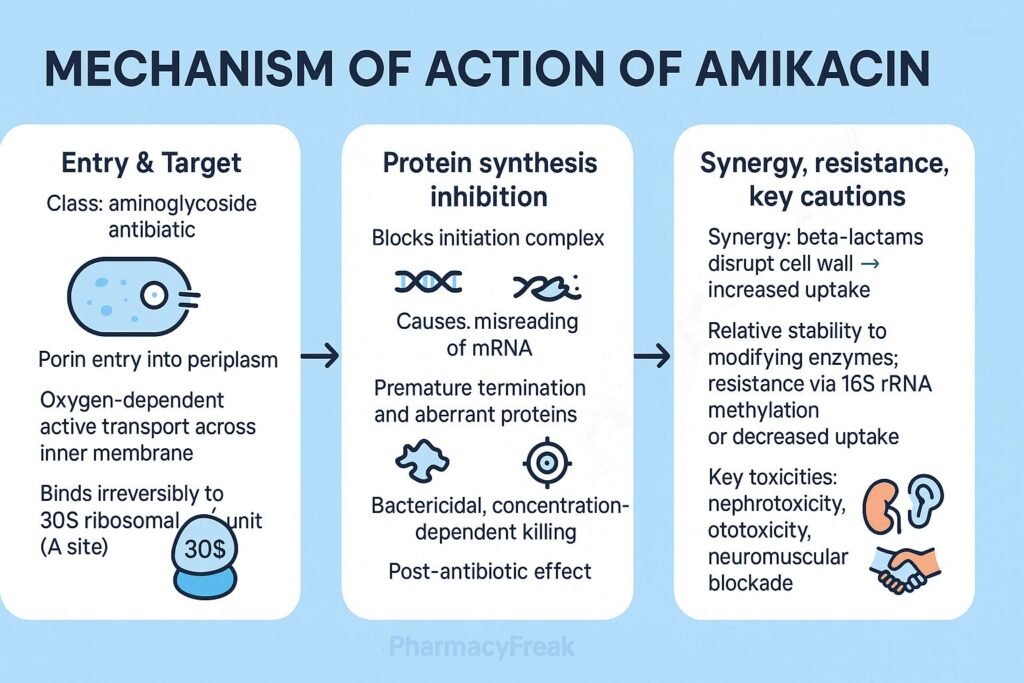
Amikacin is a broad-spectrum aminoglycoside antibiotic primarily used to treat severe Gram-negative bacterial infections, including those resistant to other aminoglycosides. Mechanism of Action of Amikacin involves irreversible inhibition of bacterial protein synthesis by binding to the 30S ribosomal subunit, leading to misreading of mRNA and defective protein formation. Because of its stability against many bacterial enzymes, amikacin is effective against multidrug-resistant strains such as Pseudomonas aeruginosa, Klebsiella pneumoniae, and Acinetobacter species.
Mechanism of Action (Step-wise)
- Active Transport into Bacterial Cell
- Amikacin enters bacterial cells through an oxygen-dependent active transport mechanism across the cytoplasmic membrane.
- This step is inhibited under anaerobic or acidic conditions, explaining its inactivity against anaerobes.
- Binding to the 30S Ribosomal Subunit
- Once inside the cytoplasm, amikacin binds irreversibly to the 30S subunit of bacterial ribosomes.
- This interaction interferes with the formation of the initiation complex for protein synthesis.
- Misreading of mRNA
- Amikacin induces misreading of genetic code during translation.
- This leads to incorporation of incorrect amino acids, resulting in nonfunctional or toxic proteins within the bacterial cell.
- Inhibition of Translocation
- The drug also interferes with the translocation step, preventing elongation of the peptide chain.
- Bacterial Cell Death
- Accumulation of defective proteins and disruption of membrane integrity leads to cell death, making amikacin bactericidal, unlike most other protein synthesis inhibitors (which are bacteriostatic).
- Overall Effect
- Amikacin → 30S binding → mRNA misreading → abnormal proteins → cell death.
Pharmacokinetics
- Absorption: Poor oral absorption; given intravenously or intramuscularly.
- Distribution: High concentrations in extracellular fluids (pleural, peritoneal, synovial).
- Metabolism: Not significantly metabolized.
- Excretion: Unchanged in urine via glomerular filtration.
- Half-life: 2–3 hours (prolonged in renal impairment).
- Post-antibiotic effect: Persistent bactericidal action even after drug levels drop below MIC.
Clinical Uses
- Severe Gram-negative infections: Pseudomonas, E. coli, Klebsiella, Enterobacter, Serratia.
- Tuberculosis (as second-line drug) resistant to streptomycin or kanamycin.
- Sepsis, pneumonia, peritonitis, urinary tract infections, and endocarditis (in combination therapy).
- Neonatal sepsis (carefully monitored dosing).
Adverse Effects
- Nephrotoxicity: Dose-related; reversible upon discontinuation.
- Ototoxicity: Irreversible damage to auditory and vestibular functions.
- Neuromuscular blockade: Can occur with high doses or in patients with myasthenia gravis.
- Allergic reactions: Rare, but may include rash or fever.
- Contraindications: Pre-existing renal disease, auditory nerve damage, or hypersensitivity to aminoglycosides.
Comparative Analysis
| Feature | Amikacin | Gentamicin | Tobramycin |
|---|---|---|---|
| Spectrum | Broad (Gram-negative + resistant strains) | Gram-negative, moderate resistance | Pseudomonas-focused |
| Enzyme resistance | Highly resistant | Moderate | Moderate |
| Route of administration | IV/IM only | IV/IM/topical | IV/IM/inhalation |
| Ototoxicity risk | High (both auditory & vestibular) | Moderate | High (vestibular) |
| Use in MDR infections | Yes | Limited | Moderate |
MCQs
1. Amikacin belongs to which antibiotic class?
a) Macrolides
b) Aminoglycosides
c) Tetracyclines
d) Fluoroquinolones
Answer: b) Aminoglycosides
2. The primary mechanism of action of amikacin is:
a) Inhibition of cell wall synthesis
b) Inhibition of protein synthesis at 30S ribosomal subunit
c) Inhibition of DNA replication
d) Disruption of folate synthesis
Answer: b) Inhibition of protein synthesis at 30S ribosomal subunit
3. Amikacin causes misreading of:
a) tRNA
b) mRNA
c) DNA
d) rRNA
Answer: b) mRNA
4. Amikacin is bactericidal because it:
a) Disrupts the bacterial membrane
b) Inhibits RNA polymerase
c) Causes production of abnormal proteins
d) Blocks folate synthesis
Answer: c) Causes production of abnormal proteins
5. Amikacin is ineffective against:
a) Aerobic Gram-negative bacilli
b) Anaerobic bacteria
c) Pseudomonas species
d) Enterobacter species
Answer: b) Anaerobic bacteria
6. The main route of elimination for amikacin is:
a) Liver
b) Kidneys
c) Lungs
d) Bile
Answer: b) Kidneys
7. Which of the following is a major dose-limiting toxicity of amikacin?
a) Hepatotoxicity
b) Nephrotoxicity and ototoxicity
c) Cardiotoxicity
d) Neurotoxicity only
Answer: b) Nephrotoxicity and ototoxicity
8. Amikacin should not be given with:
a) Beta-lactams
b) Cephalosporins
c) Loop diuretics
d) Macrolides
Answer: c) Loop diuretics
9. The transport of amikacin into bacteria is:
a) Passive diffusion
b) Active transport (oxygen-dependent)
c) Facilitated diffusion
d) Endocytosis
Answer: b) Active transport (oxygen-dependent)
10. Amikacin is effective against which resistant organism?
a) MRSA
b) ESBL-producing E. coli
c) Pseudomonas aeruginosa
d) Mycoplasma pneumoniae
Answer: c) Pseudomonas aeruginosa
FAQs
Q1. How does amikacin differ from gentamicin?
Amikacin is more resistant to bacterial inactivating enzymes and effective against multidrug-resistant Gram-negative organisms.
Q2. Why can’t amikacin treat anaerobic infections?
Its transport into bacterial cells requires oxygen-dependent mechanisms absent in anaerobes.
Q3. How is amikacin administered?
It is given by IV or IM injection; oral absorption is negligible.
Q4. Can amikacin be used in combination with other antibiotics?
Yes, it is often used synergistically with beta-lactams or vancomycin against severe infections.
Q5. What should be monitored during amikacin therapy?
Serum creatinine, urine output, and hearing function to prevent toxicity.
Q6. Is amikacin safe in pregnancy?
No, it is avoided due to the risk of fetal ototoxicity and nephrotoxicity.
References
- Goodman & Gilman’s The Pharmacological Basis of Therapeutics
- Katzung’s Basic and Clinical Pharmacology
- Harrison’s Principles of Internal Medicine
- WHO Antimicrobial Therapy Guidelines
Related Internal Links

I am pursuing MBA in pharmaceutical management from NIPER Hyderabad with a strong academic record and proven success in national-level pharmacy entrance exams. I secured AIR 61 in NIPER 2024 (MS/M.Pharm) and AIR 27 in NIPER MBA, along with AIR 147 in GPAT 2024 and AIR 907 in GPAT 2023. I also achieved AIR 6 in AIIMS CRE-2025 for Drug Store Keeper and was selected as a Pharmacist (AIR 61) for ESIC. Additionally, I was the Runner-Up in Round 2 of the EY Case Study Competition.
At PharmacyFreak.com, I aim to guide future pharmacists through expert content, exam strategies, and insightful resources based on real experience and academic excellence.
Mail- harsh@pharmacyfreak.com