Table of Contents
Introduction
Fluconazole is a triazole antifungal agent widely used in the treatment and prophylaxis of systemic and superficial fungal infections. It is especially effective against Candida species and Cryptococcus neoformans. Fluconazole is high-yield for pharmacology and infectious disease examinations due to its selective inhibition of fungal sterol synthesis, excellent oral bioavailability, CNS penetration, and characteristic drug–drug interactions.
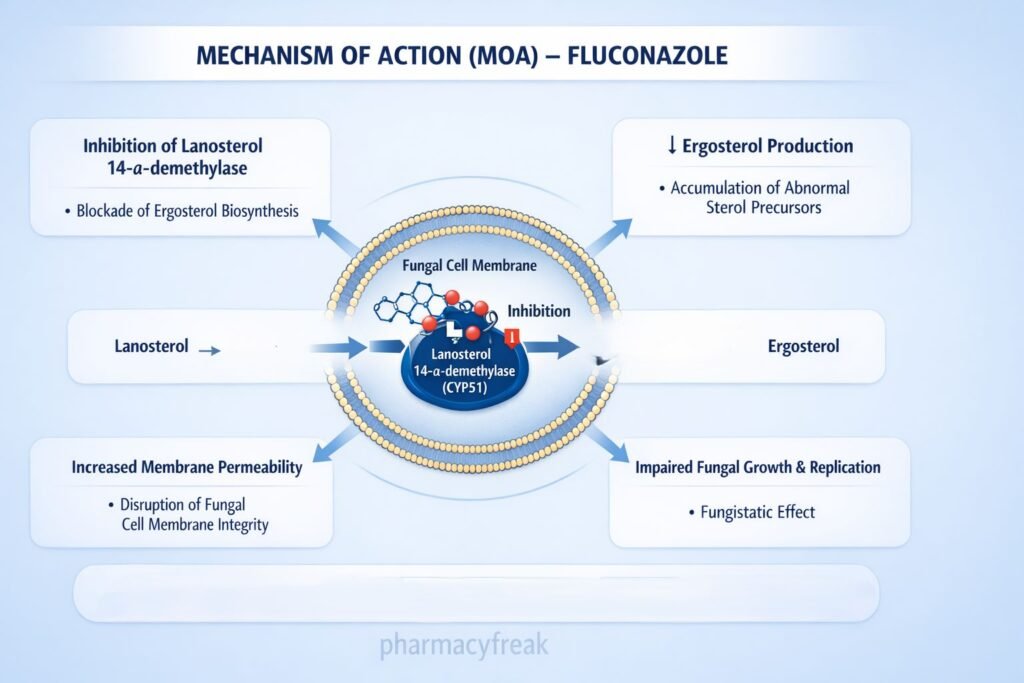

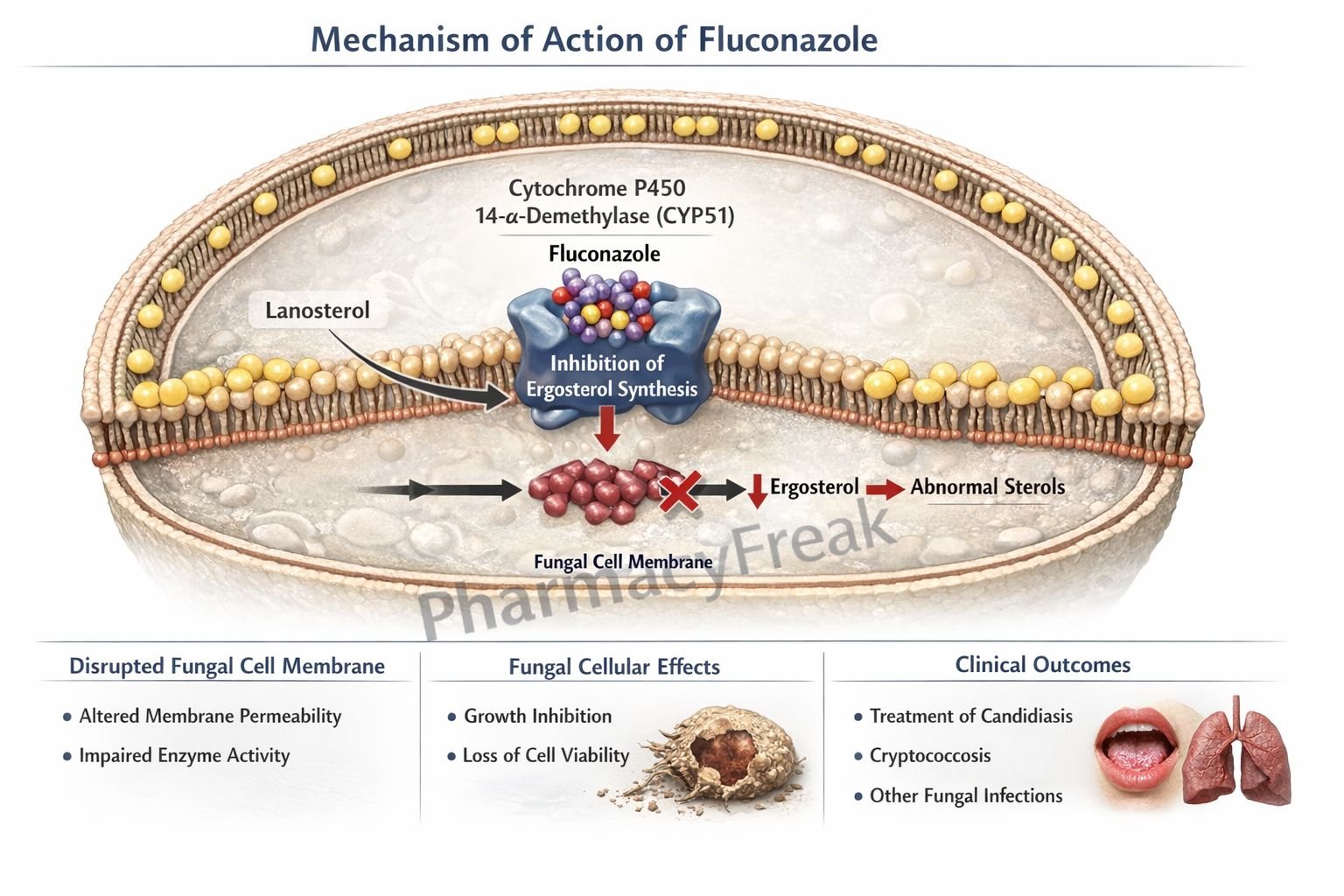
Mechanism of Action (Step-wise)
Fluconazole inhibits fungal cell membrane synthesis by blocking ergosterol production.
Step 1: Entry into fungal cells
Fluconazole penetrates fungal cells and reaches intracellular metabolic pathways.
Step 2: Inhibition of fungal cytochrome P450 enzyme
It selectively inhibits lanosterol 14-α-demethylase, a fungal cytochrome P450–dependent enzyme.
Step 3: Blockade of ergosterol synthesis
Inhibition of this enzyme prevents conversion of lanosterol to ergosterol, a critical component of the fungal cell membrane.
Step 4: Accumulation of toxic sterol intermediates
Abnormal sterol accumulation disrupts membrane integrity and function.
Step 5: Increased membrane permeability and growth inhibition
Defective cell membranes impair fungal growth and replication, producing a fungistatic effect.
Exam pearl:
Fluconazole has minimal effect on human cholesterol synthesis due to higher selectivity for fungal enzymes.
Pharmacokinetics
- Route of administration: Oral, IV
- Bioavailability: >90% (not affected by food or gastric pH)
- Protein binding: Low
- Distribution: Excellent tissue and CSF penetration
- Metabolism: Minimal hepatic metabolism
- Half-life: ~30 hours
- Excretion: Primarily renal (unchanged drug)
- Dose adjustment: Required in renal impairment
Clinical Uses
- Oropharyngeal and esophageal candidiasis
- Vulvovaginal candidiasis
- Systemic candidiasis
- Cryptococcal meningitis (maintenance therapy)
- Fungal prophylaxis in immunocompromised patients
- Coccidioidomycosis
Fluconazole is ineffective against molds such as Aspergillus.
Adverse Effects
Gastrointestinal:
- Nausea
- Abdominal pain
- Diarrhea
Hepatic:
- Elevated liver enzymes
- Hepatotoxicity (rare)
Dermatological:
- Rash
- Stevens–Johnson syndrome (rare)
Endocrine:
- Minimal (unlike ketoconazole)
Drug interactions:
- Inhibition of CYP2C9 and CYP3A4 → ↑ warfarin, phenytoin, sulfonylurea levels
Comparative Analysis
Fluconazole vs Ketoconazole vs Amphotericin B
| Feature | Fluconazole | Ketoconazole | Amphotericin B |
|---|---|---|---|
| Drug class | Triazole | Imidazole | Polyene |
| Ergosterol synthesis inhibition | Yes | Yes | No |
| Cell membrane binding | No | No | Yes |
| Oral bioavailability | Excellent | Variable | Poor |
| CNS penetration | Good | Poor | Poor |
| Major toxicity | Hepatotoxicity | Endocrine effects | Nephrotoxicity |
| Fungistatic/cidal | Fungistatic | Fungistatic | Fungicidal |
Explanation:
Fluconazole offers superior safety and CNS penetration compared with ketoconazole and amphotericin B. Amphotericin B is fungicidal but limited by severe toxicity.
MCQs
- Fluconazole inhibits synthesis of:
a) Peptidoglycan
b) Ergosterol
c) Cholesterol
d) Mycolic acid
Answer: b) Ergosterol
- Target enzyme inhibited by fluconazole is:
a) Squalene epoxidase
b) DNA gyrase
c) Lanosterol 14-α-demethylase
d) Topoisomerase II
Answer: c) Lanosterol 14-α-demethylase
- Fluconazole belongs to which antifungal class?
a) Polyenes
b) Echinocandins
c) Imidazoles
d) Triazoles
Answer: d) Triazoles
- Nature of antifungal action of fluconazole is:
a) Fungicidal
b) Fungistatic
c) Virucidal
d) Bactericidal
Answer: b) Fungistatic
- Fluconazole has excellent penetration into:
a) Bone
b) CSF
c) Adipose tissue
d) Pleural fluid only
Answer: b) CSF
- Fluconazole is primarily excreted via the:
a) Liver
b) Bile
c) Kidney
d) Lungs
Answer: c) Kidney
- Which organism is commonly treated with fluconazole?
a) Aspergillus fumigatus
b) Candida albicans
c) Mucor
d) Histoplasma capsulatum
Answer: b) Candida albicans
- Fluconazole increases levels of warfarin because it:
a) Induces CYP enzymes
b) Inhibits CYP enzymes
c) Increases renal excretion
d) Blocks protein binding
Answer: b) Inhibits CYP enzymes
- Compared to ketoconazole, fluconazole causes:
a) More endocrine effects
b) Less hepatotoxicity
c) Poor oral absorption
d) More drug interactions
Answer: b) Less hepatotoxicity
- Dose adjustment of fluconazole is required in:
a) Liver disease
b) Renal impairment
c) Heart failure
d) Diabetes
Answer: b) Renal impairment
FAQs
1. Why is fluconazole preferred for cryptococcal meningitis?
Because it penetrates the CSF effectively.
2. Does fluconazole affect human cholesterol synthesis?
Minimal effect due to fungal enzyme selectivity.
3. Can fluconazole be used orally?
Yes, with excellent bioavailability.
4. Is fluconazole effective against molds?
No, it is ineffective against Aspergillus.
5. Why are drug interactions common with fluconazole?
Due to CYP450 enzyme inhibition.
References
- Goodman & Gilman’s The Pharmacological Basis of Therapeutics
https://accesspharmacy.mhmedical.com - Katzung BG. Basic and Clinical Pharmacology
https://accessmedicine.mhmedical.com - Tripathi KD. Essentials of Medical Pharmacology
- Harrison’s Principles of Internal Medicine
https://accessmedicine.mhmedical.com

I am pursuing MBA in pharmaceutical management from NIPER Hyderabad with a strong academic record and proven success in national-level pharmacy entrance exams. I secured AIR 61 in NIPER 2024 (MS/M.Pharm) and AIR 27 in NIPER MBA, along with AIR 147 in GPAT 2024 and AIR 907 in GPAT 2023. I also achieved AIR 6 in AIIMS CRE-2025 for Drug Store Keeper and was selected as a Pharmacist (AIR 61) for ESIC. Additionally, I was the Runner-Up in Round 2 of the EY Case Study Competition.
At PharmacyFreak.com, I aim to guide future pharmacists through expert content, exam strategies, and insightful resources based on real experience and academic excellence.
Mail- harsh@pharmacyfreak.com