Table of Contents
Introduction
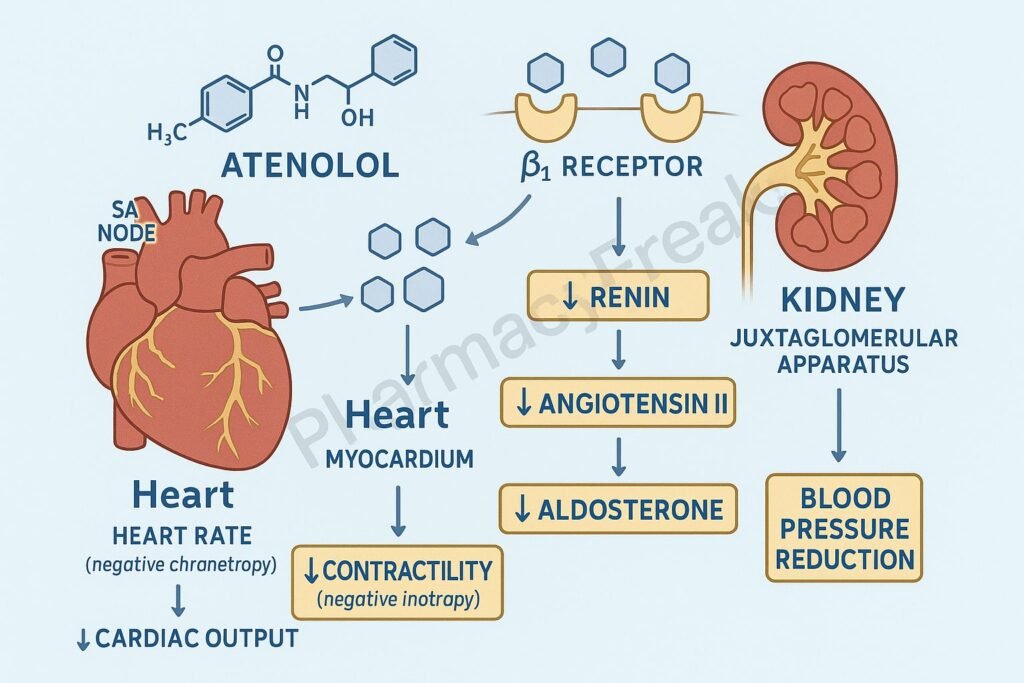
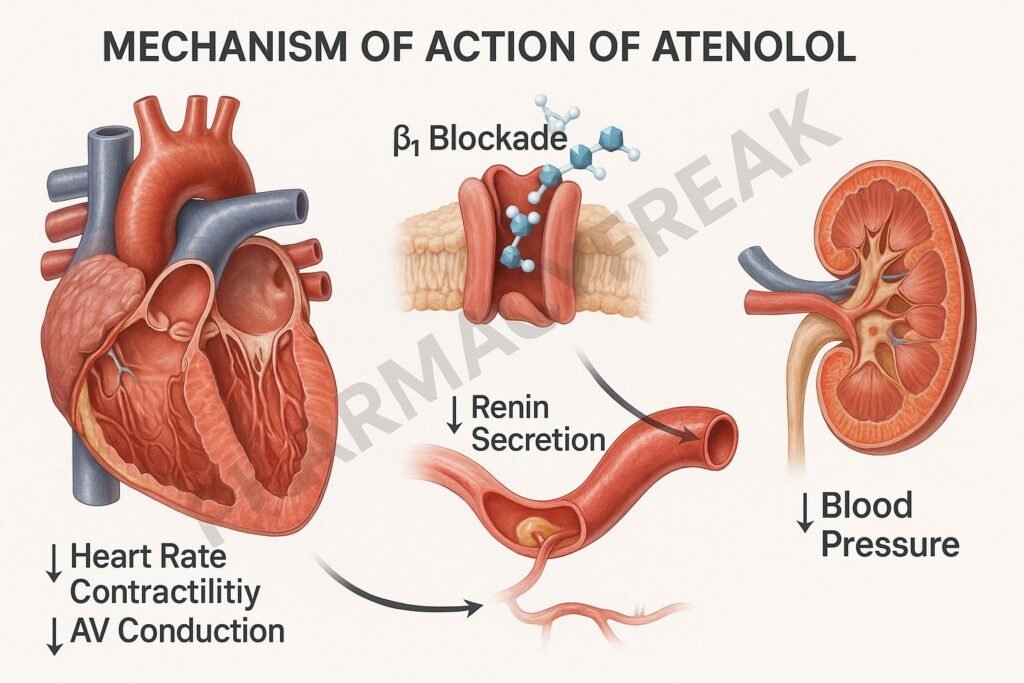
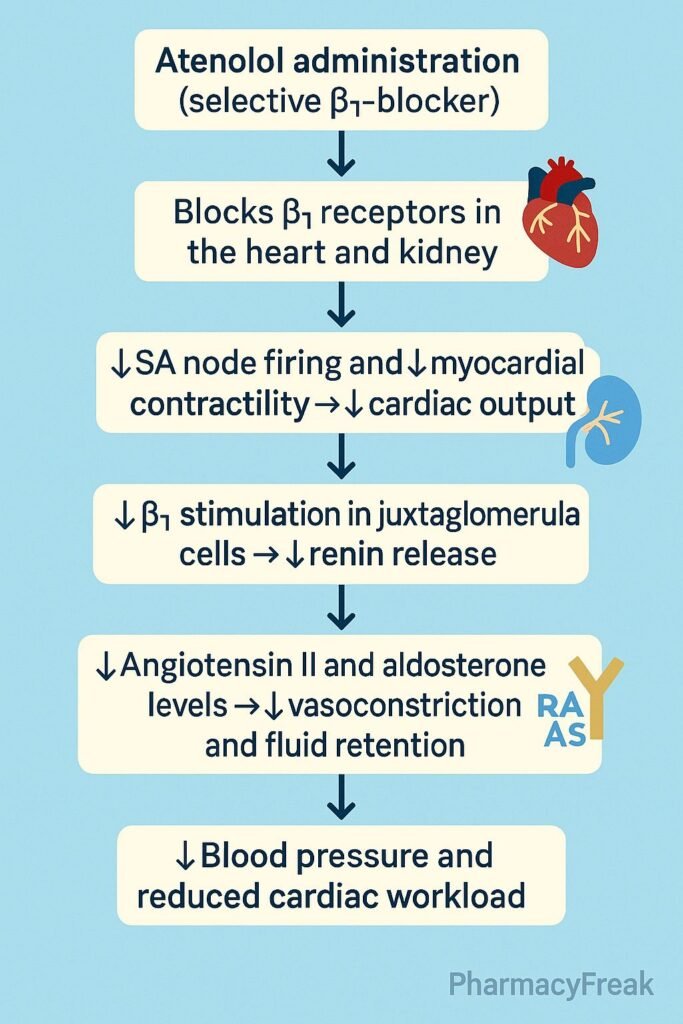
Atenolol is a selective β₁-adrenergic receptor blocker (β-blocker) primarily used in the management of hypertension, angina pectoris, arrhythmias, and post-myocardial infarction therapy. Its mechanism of action involves blocking β₁ receptors in the heart, which decreases heart rate, contractility, and cardiac output — leading to a reduction in blood pressure and myocardial oxygen demand.
Unlike non-selective β-blockers (e.g., propranolol), atenolol exhibits cardioselectivity, meaning it primarily affects the heart without significantly influencing β₂ receptors in bronchial or vascular smooth muscle. This makes it safer for patients with mild respiratory disease.
Mechanism of Action (Step-wise)
1. Blockade of β₁-Adrenergic Receptors in the Heart
- Mechanism:
- Atenolol competitively blocks β₁-adrenergic receptors located in cardiac tissue.
- These receptors normally respond to sympathetic neurotransmitters — norepinephrine and epinephrine — which increase heart rate and force of contraction via adenylyl cyclase activation and cAMP production.
- By inhibiting these receptors, atenolol reduces intracellular cAMP levels, decreasing calcium influx into cardiac myocytes.
- Effects:
- ↓ Heart rate (negative chronotropic effect)
- ↓ Myocardial contractility (negative inotropic effect)
- ↓ AV node conduction (negative dromotropic effect)
- ↓ Myocardial oxygen demand
2. Reduction in Cardiac Output and Blood Pressure
- Mechanism:
- Reduced contractility and heart rate lead to decreased cardiac output (CO = HR × SV).
- Long-term use lowers total peripheral resistance (TPR) through baroreceptor and renin suppression mechanisms.
- Effects:
- ↓ Blood pressure
- ↓ Workload on the heart
3. Inhibition of Renin Release (Renin–Angiotensin–Aldosterone System)
- Mechanism:
- β₁ receptors are present in juxtaglomerular cells of the kidney.
- Atenolol blocks these receptors, inhibiting renin secretion → ↓ formation of angiotensin II → ↓ aldosterone release.
- Effects:
- ↓ Sodium and water retention
- ↓ Plasma volume and vascular resistance
- Further contributes to antihypertensive action
4. Decrease in Sympathetic Outflow
- Mechanism:
- Chronic β₁ blockade reduces central sympathetic activity and catecholamine sensitivity.
- This dampens reflex tachycardia, especially beneficial in hypertension and ischemic heart disease.
- Effect:
- Stabilized heart rhythm and reduced cardiovascular reactivity to stress.
5. Overall Pharmacodynamic Effects
| Site of Action | Mechanism | Resulting Effect |
|---|---|---|
| Heart (β₁ blockade) | ↓ cAMP → ↓ Ca²⁺ influx | ↓ HR, ↓ contractility |
| Kidneys | ↓ Renin secretion | ↓ Angiotensin II, ↓ BP |
| CNS (indirect) | ↓ Sympathetic tone | ↓ HR, ↓ BP |
| AV Node | Slowed conduction | Antiarrhythmic effect |
Pharmacokinetics
- Absorption: Well absorbed orally; bioavailability ~50% (due to first-pass metabolism).
- Onset of Action: 1–2 hours after oral dose.
- Half-life: ~6–9 hours.
- Metabolism: Minimal hepatic metabolism (unlike propranolol).
- Elimination: Primarily renal (unchanged drug).
- Dosing: Once or twice daily (25–100 mg typical dose).
Clinical Uses
- Hypertension (monotherapy or combination therapy).
- Angina pectoris (reduces oxygen demand and improves exercise tolerance).
- Myocardial infarction (reduces reinfarction and mortality risk).
- Cardiac arrhythmias (especially supraventricular tachycardia, atrial fibrillation rate control).
- Migraine prophylaxis (off-label).
Adverse Effects
- Common: Bradycardia, fatigue, dizziness, hypotension, cold extremities.
- Metabolic: May mask hypoglycemia symptoms in diabetic patients.
- Respiratory: Caution in asthma/COPD (though cardioselective, β₂ cross-reactivity possible at high doses).
- CNS: Depression, sleep disturbances (less likely than lipophilic β-blockers).
- Withdrawal: Sudden discontinuation may cause rebound tachycardia or hypertension.
Contraindications
- Sinus bradycardia, second or third-degree AV block.
- Overt cardiac failure.
- Cardiogenic shock.
- Severe peripheral vascular disease.
- Caution: Asthma, diabetes, renal impairment.
Comparative Table: Atenolol vs Other β-Blockers
| Feature | Atenolol | Propranolol | Metoprolol |
|---|---|---|---|
| Selectivity | β₁-selective | Non-selective (β₁ + β₂) | β₁-selective |
| Lipid Solubility | Low | High | Moderate |
| CNS Effects | Minimal | Prominent | Moderate |
| Metabolism | Renal excretion | Hepatic metabolism | Hepatic metabolism |
| Half-life | 6–9 hours | 3–6 hours | 3–7 hours |
| Uses | HTN, angina, MI, arrhythmia | HTN, tremor, migraine | HTN, heart failure, MI |
MCQs
1. Atenolol is classified as:
a) Non-selective β-blocker
b) β₁-selective blocker
c) α-blocker
d) Mixed α/β blocker
Answer: b) β₁-selective blocker
2. Primary mechanism of atenolol involves:
a) Calcium channel blockade
b) β₁ receptor blockade
c) α₁ receptor blockade
d) ACE inhibition
Answer: b) β₁ receptor blockade
3. Atenolol lowers blood pressure by:
a) Increasing heart rate
b) Reducing cardiac output and renin release
c) Blocking α₂ receptors
d) Enhancing sodium reabsorption
Answer: b) Reducing cardiac output and renin release
4. The major site of atenolol action is:
a) Liver
b) Heart and kidneys
c) Brain
d) Adrenal glands
Answer: b) Heart and kidneys
5. Atenolol is preferred in:
a) COPD
b) Asthma
c) Hypertension with angina
d) Peripheral vascular disease
Answer: c) Hypertension with angina
6. Atenolol differs from propranolol because it:
a) Is non-selective
b) Is lipophilic
c) Has minimal CNS effects
d) Causes bronchoconstriction
Answer: c) Has minimal CNS effects
7. The main mechanism in arrhythmia control by atenolol is:
a) Sodium channel blockade
b) Potassium channel blockade
c) AV node conduction slowing
d) Calcium influx stimulation
Answer: c) AV node conduction slowing
8. Atenolol reduces myocardial oxygen demand by:
a) Increasing HR
b) Decreasing HR and contractility
c) Increasing preload
d) Stimulating β₂ receptors
Answer: b) Decreasing HR and contractility
9. Abrupt withdrawal of atenolol causes:
a) Bradycardia
b) Rebound hypertension and tachycardia
c) Sedation
d) Hypotension only
Answer: b) Rebound hypertension and tachycardia
10. The elimination route of atenolol is primarily:
a) Biliary
b) Renal
c) Hepatic
d) Pulmonary
Answer: b) Renal
FAQs
Q1. Why is atenolol called cardioselective?
Because it selectively blocks β₁ receptors in cardiac tissue, minimizing β₂ receptor blockade in bronchi and vessels.
Q2. Can atenolol be used in asthma?
It may be used with caution in mild asthma, but cardioselectivity is dose-dependent — higher doses can still cause bronchospasm.
Q3. Why is atenolol preferred in hypertension with angina?
Because it reduces both blood pressure and myocardial oxygen demand, relieving anginal pain.
Q4. Can atenolol be given to diabetic patients?
Yes, but it may mask hypoglycemia symptoms like tachycardia; glucose monitoring is advised.
Q5. What happens if atenolol is abruptly stopped?
Sudden discontinuation can cause rebound hypertension, tachycardia, or angina due to upregulation of β receptors.
References

I am pursuing MBA in pharmaceutical management from NIPER Hyderabad with a strong academic record and proven success in national-level pharmacy entrance exams. I secured AIR 61 in NIPER 2024 (MS/M.Pharm) and AIR 27 in NIPER MBA, along with AIR 147 in GPAT 2024 and AIR 907 in GPAT 2023. I also achieved AIR 6 in AIIMS CRE-2025 for Drug Store Keeper and was selected as a Pharmacist (AIR 61) for ESIC. Additionally, I was the Runner-Up in Round 2 of the EY Case Study Competition.
At PharmacyFreak.com, I aim to guide future pharmacists through expert content, exam strategies, and insightful resources based on real experience and academic excellence.
Mail- harsh@pharmacyfreak.com

