Table of Contents
Introduction
Warfarin is a widely used oral anticoagulant that inhibits the synthesis of vitamin K-dependent clotting factors. It is commonly prescribed for atrial fibrillation, deep vein thrombosis (DVT), pulmonary embolism, and prosthetic heart valves. Due to its narrow therapeutic window, multiple drug interactions, and the need for INR monitoring, warfarin is a high-yield topic for students preparing for USMLE, NCLEX, NAPLEX, GPAT, and NEET-PG.
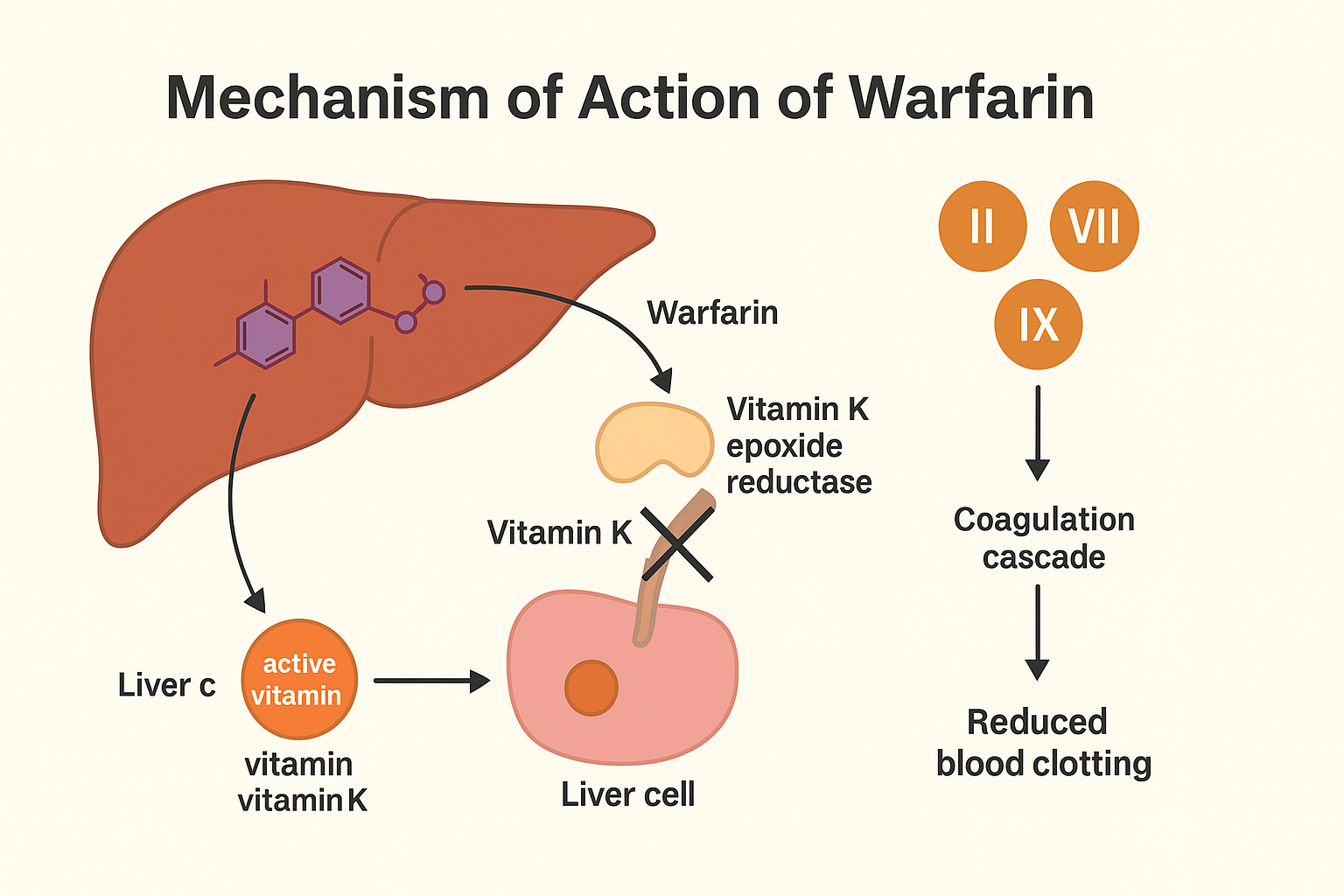
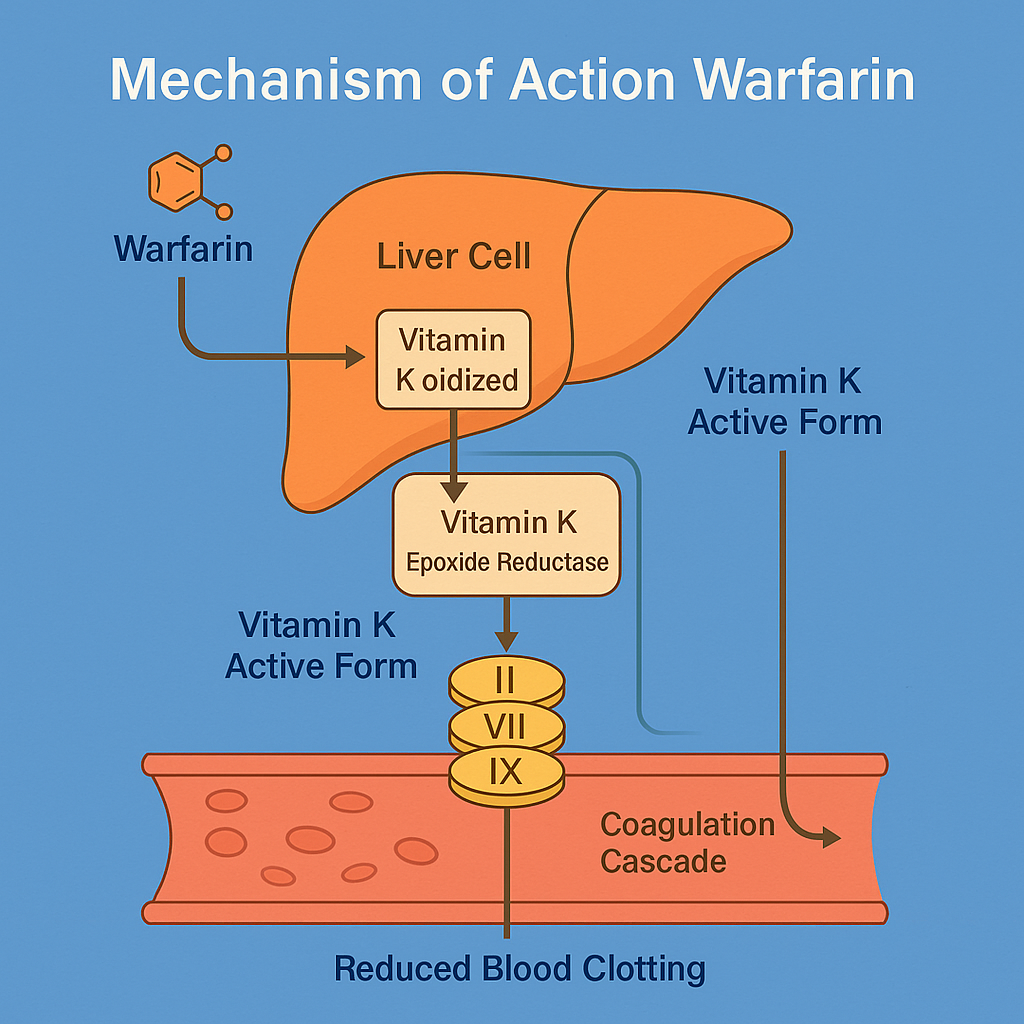
Mechanism of Action of Warfarin: Step-by-Step
- Inhibition of Vitamin K epoxide reductase (VKORC1)
Warfarin inhibits VKORC1, the enzyme responsible for regenerating reduced vitamin K. - Prevention of γ-carboxylation
Without reduced vitamin K, the γ-carboxylation of glutamic acid residues in clotting factors is blocked. - Production of inactive clotting factors
This leads to the synthesis of biologically inactive clotting factors II, VII, IX, and X, and proteins C and S. - Delayed onset of action
Warfarin does not affect already circulating clotting factors, so the full anticoagulant effect is delayed until existing factors degrade. - Monitoring with INR
The drug’s activity is monitored via the international normalized ratio (INR), with a typical therapeutic range of 2.0–3.0.
Pharmacokinetic Parameters of Warfarin
| Parameter | Value |
|---|---|
| Bioavailability | ~100% (oral) |
| Half-life | ~36–42 hours |
| Protein binding | ~99% (albumin) |
| Metabolism | Hepatic (CYP2C9, CYP3A4) |
| Excretion | Renal (as metabolites) |
| Onset of action | 24–72 hours |
| Duration of action | 2–5 days (due to irreversible inhibition) |
Clinical Uses of Warfarin
- Prophylaxis and treatment of DVT and PE
- Prevention of stroke in atrial fibrillation
- Mechanical prosthetic heart valves
- Post-MI prophylaxis in selected patients
- Hypercoagulable states (e.g., protein C or S deficiency)
Adverse Effects of Warfarin
- Bleeding (major risk)
- Skin necrosis (early, due to protein C depletion)
- Teratogenicity (fetal warfarin syndrome)
- Purple toe syndrome
- Drug interactions (CYP inhibitors/inducers)
- Requires regular INR monitoring
Comparative Analysis: Warfarin vs DOACs (e.g., Apixaban)
| Feature | Warfarin | DOACs (Apixaban, Rivaroxaban) |
|---|---|---|
| Target | Vitamin K epoxide reductase | Factor Xa or thrombin |
| Onset of action | Slow (24–72 hrs) | Rapid (2–4 hrs) |
| Monitoring | Required (INR) | Usually not required |
| Reversal agent | Vitamin K, FFP | Andexanet alfa (Xa); idarucizumab (IIa) |
| Diet interaction | Yes (vitamin K intake matters) | No |
| Use in pregnancy | Contraindicated | Contraindicated |
Practice MCQs
Q1. Warfarin inhibits which enzyme?
a. Cyclooxygenase
b. Thrombin
c. Vitamin K epoxide reductase ✅
d. Factor Xa
Q2. Which clotting factors are affected by warfarin?
a. II, VII, IX, X ✅
b. I, V, VIII, XIII
c. All clotting factors
d. Platelet factors
Q3. Warfarin requires monitoring of:
a. aPTT
b. Platelet count
c. INR ✅
d. Bleeding time
Q4. Warfarin is contraindicated in:
a. Diabetes
b. Pregnancy ✅
c. Asthma
d. Hypertension
Q5. Onset of action of warfarin is:
a. Immediate
b. 6 hours
c. 24–72 hours ✅
d. 1 week
Q6. Which protein is affected early by warfarin and causes skin necrosis?
a. Protein A
b. Protein B
c. Protein C ✅
d. Protein D
Q7. Warfarin is metabolized by:
a. Kidneys
b. CYP3A4 and CYP2C9 ✅
c. Plasma esterases
d. Acetylation
Q8. Which vitamin reverses warfarin effect?
a. B12
b. C
c. K ✅
d. D
Q9. Which food reduces warfarin’s effect?
a. Cheese
b. Yogurt
c. Leafy greens (high vitamin K) ✅
d. Eggs
Q10. Antidote for warfarin overdose includes:
a. Protamine
b. Vitamin K ✅
c. Naloxone
d. Glucagon
FAQs
Q1: Is warfarin safe in pregnancy?
No. Warfarin is teratogenic and contraindicated during pregnancy.
Q2: Can I eat spinach while on warfarin?
Yes, but maintain consistent intake of vitamin K-rich foods.
Q3: Why is INR monitoring necessary?
To avoid bleeding or inadequate anticoagulation. Target INR: 2.0–3.0 (except in mechanical valves: 2.5–3.5).
Q4: What drugs interact with warfarin?
Many, including NSAIDs, antibiotics, antifungals, and antiepileptics.
Q5: Can warfarin and aspirin be used together?
Yes, but increases bleeding risk — only under strict medical supervision.
References
- KD Tripathi – Essentials of Medical Pharmacology
- Goodman & Gilman – The Pharmacological Basis of Therapeutics
- Sparsh Gupta – Review of Pharmacology
- NCBI: https://www.ncbi.nlm.nih.gov/books/NBK470440/

I am pursuing MBA in pharmaceutical management from NIPER Hyderabad with a strong academic record and proven success in national-level pharmacy entrance exams. I secured AIR 61 in NIPER 2024 (MS/M.Pharm) and AIR 27 in NIPER MBA, along with AIR 147 in GPAT 2024 and AIR 907 in GPAT 2023. I also achieved AIR 6 in AIIMS CRE-2025 for Drug Store Keeper and was selected as a Pharmacist (AIR 61) for ESIC. Additionally, I was the Runner-Up in Round 2 of the EY Case Study Competition.
At PharmacyFreak.com, I aim to guide future pharmacists through expert content, exam strategies, and insightful resources based on real experience and academic excellence.
Mail- harsh@pharmacyfreak.com