Table of Contents
Introduction
Flucytosine (5-fluorocytosine) is a fluorinated pyrimidine antifungal agent primarily used in combination therapy for serious systemic fungal infections. It is especially important in the treatment of cryptococcal meningitis and severe candidiasis, where it is commonly combined with amphotericin B to enhance efficacy and reduce resistance. Flucytosine is high-yield for exams due to its unique intracellular activation, selective fungal toxicity, and characteristic bone marrow suppression.
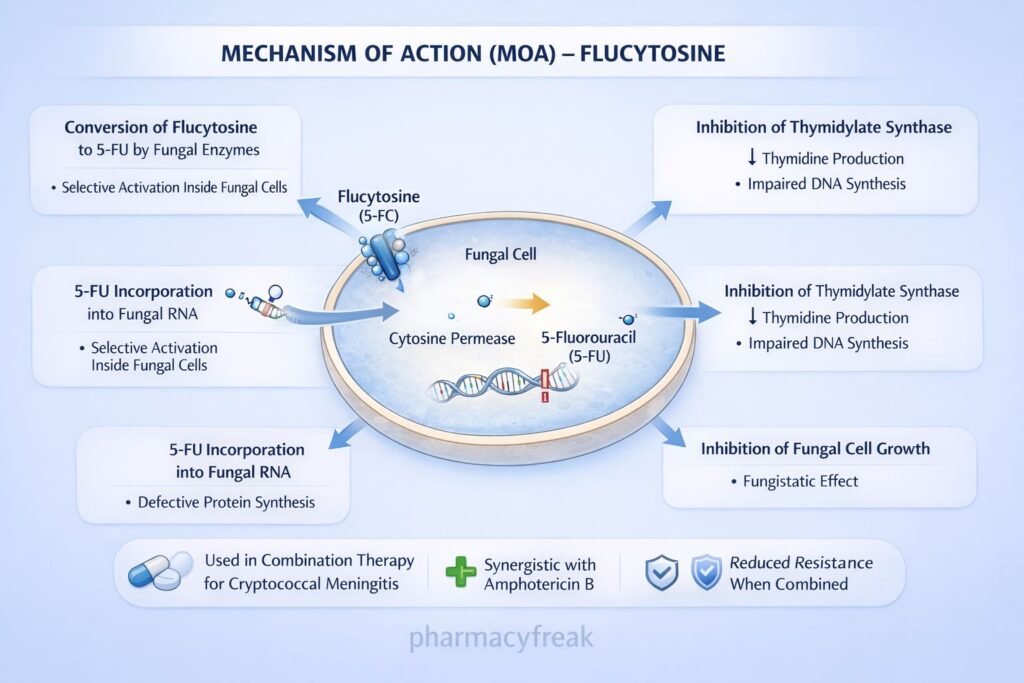
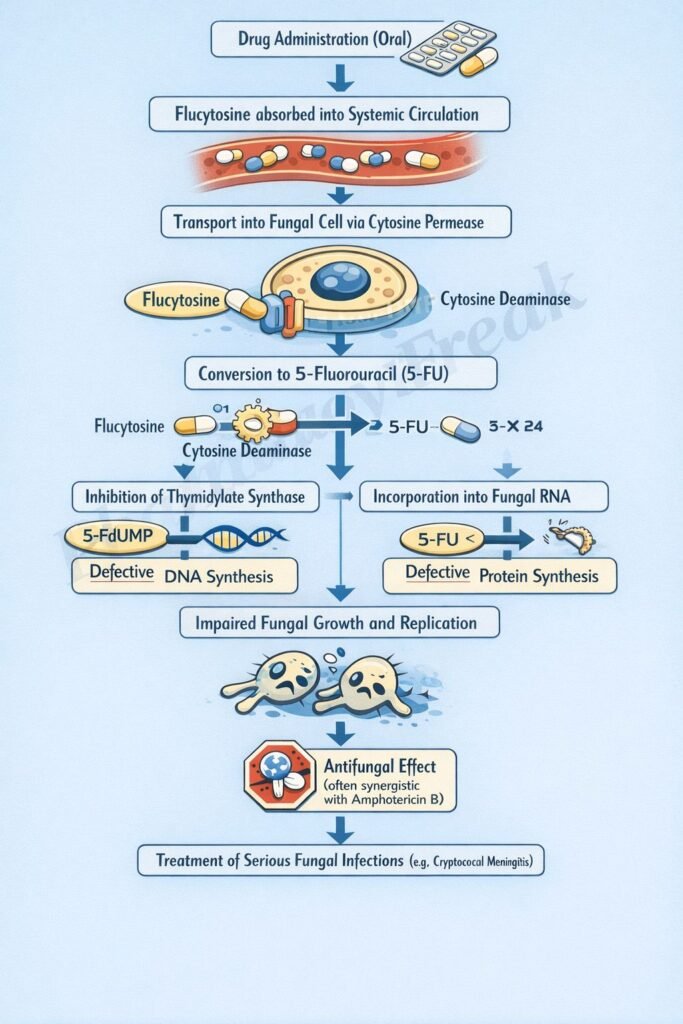
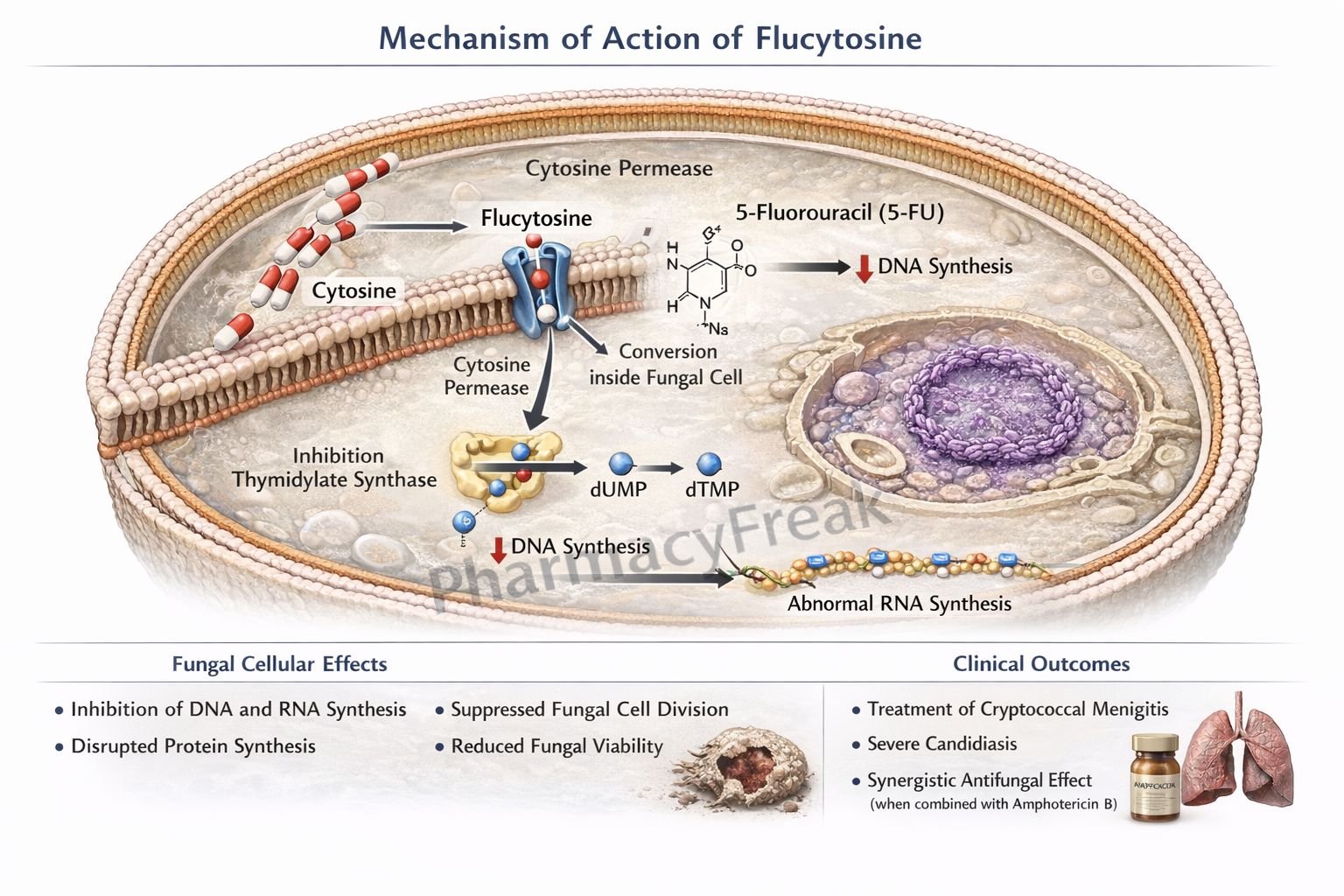
Mechanism of Action (Step-wise)
Flucytosine inhibits fungal DNA and RNA synthesis after intracellular conversion to active metabolites.
Step 1: Entry into fungal cells
Flucytosine enters fungal cells via cytosine permease, a transporter absent in human cells.
Step 2: Conversion to 5-fluorouracil (5-FU)
Inside the fungal cell, flucytosine is deaminated by cytosine deaminase to form 5-fluorouracil.
Step 3: Inhibition of DNA synthesis
5-FU is converted to 5-fluorodeoxyuridine monophosphate (FdUMP), which inhibits thymidylate synthase, reducing thymidine production and impairing DNA synthesis.
Step 4: Inhibition of RNA synthesis
Another metabolite, 5-fluorouridine triphosphate (FUTP), is incorporated into fungal RNA, leading to defective RNA and protein synthesis.
Step 5: Fungistatic effect
Combined inhibition of DNA and RNA synthesis suppresses fungal growth and replication.
Exam pearl:
Human cells lack cytosine deaminase, explaining selective antifungal toxicity.
Pharmacokinetics
- Route of administration: Oral
- Bioavailability: ~90%
- Protein binding: Minimal
- Distribution: Excellent tissue and CSF penetration
- Metabolism: Minimal hepatic metabolism
- Half-life: 3–6 hours
- Excretion: Renal (unchanged drug)
- Dose adjustment: Required in renal impairment
Clinical Uses
- Cryptococcal meningitis (with amphotericin B)
- Systemic candidiasis (combination therapy)
- Fungal endocarditis (adjunct)
Flucytosine is never used as monotherapy due to rapid development of resistance.
Adverse Effects
Hematological (dose-limiting):
- Bone marrow suppression
- Leukopenia
- Thrombocytopenia
Gastrointestinal:
- Nausea
- Vomiting
- Diarrhea
Hepatic:
- Elevated liver enzymes
Dermatological:
- Rash
Exam warning:
Toxicity resembles 5-fluorouracil due to metabolic conversion.
Comparative Analysis
Flucytosine vs Fluconazole vs Amphotericin B
| Feature | Flucytosine | Fluconazole | Amphotericin B |
|---|---|---|---|
| Mechanism | DNA & RNA synthesis inhibition | Ergosterol synthesis inhibition | Cell membrane binding |
| Fungistatic/cidal | Fungistatic | Fungistatic | Fungicidal |
| CNS penetration | Excellent | Excellent | Poor |
| Resistance | Rapid (monotherapy) | Moderate | Rare |
| Major toxicity | Bone marrow suppression | Hepatotoxicity | Nephrotoxicity |
| Use alone | No | Yes | Yes |
Explanation:
Flucytosine’s intracellular activation and dual inhibition of nucleic acid synthesis make it highly effective when combined with amphotericin B. However, rapid resistance and hematologic toxicity limit its standalone use.
MCQs
- Flucytosine enters fungal cells via:
a) Passive diffusion
b) Ergosterol pores
c) Cytosine permease
d) Endocytosis
Answer: c) Cytosine permease
- Active metabolite of flucytosine is:
a) Fluconazole
b) 5-fluorouracil
c) Amphotericin B
d) Cytosine
Answer: b) 5-fluorouracil
- Enzyme converting flucytosine to 5-FU is:
a) Thymidylate synthase
b) Cytosine deaminase
c) DNA polymerase
d) RNA polymerase
Answer: b) Cytosine deaminase
- Flucytosine inhibits DNA synthesis by blocking:
a) DNA gyrase
b) RNA polymerase
c) Thymidylate synthase
d) Topoisomerase II
Answer: c) Thymidylate synthase
- Major dose-limiting toxicity of flucytosine is:
a) Nephrotoxicity
b) Hepatotoxicity
c) Bone marrow suppression
d) Neurotoxicity
Answer: c) Bone marrow suppression
- Flucytosine is most commonly used with:
a) Ketoconazole
b) Fluconazole
c) Amphotericin B
d) Caspofungin
Answer: c) Amphotericin B
- Flucytosine has excellent penetration into the:
a) Bone
b) CSF
c) Adipose tissue
d) Pleura only
Answer: b) CSF
- Flucytosine is primarily excreted by the:
a) Liver
b) Lung
c) Kidney
d) Intestine
Answer: c) Kidney
- Resistance to flucytosine develops rapidly due to:
a) Efflux pumps
b) Loss of cytosine permease
c) Ergosterol mutation
d) Increased metabolism
Answer: b) Loss of cytosine permease
- Flucytosine toxicity resembles which anticancer drug?
a) Methotrexate
b) Cyclophosphamide
c) 5-Fluorouracil
d) Cisplatin
Answer: c) 5-Fluorouracil
FAQs
1. Why is flucytosine not used alone?
Due to rapid development of resistance.
2. Why is flucytosine selective for fungi?
Human cells lack cytosine deaminase.
3. What infection is flucytosine most associated with?
Cryptococcal meningitis.
4. What lab parameter should be monitored closely?
Complete blood count.
5. Can flucytosine cross the blood–brain barrier?
Yes, it has excellent CSF penetration.
References
- Goodman & Gilman’s The Pharmacological Basis of Therapeutics
https://accesspharmacy.mhmedical.com - Katzung BG. Basic and Clinical Pharmacology
https://accessmedicine.mhmedical.com - Tripathi KD. Essentials of Medical Pharmacology
- Harrison’s Principles of Internal Medicine
https://accessmedicine.mhmedical.com

I am pursuing MBA in pharmaceutical management from NIPER Hyderabad with a strong academic record and proven success in national-level pharmacy entrance exams. I secured AIR 61 in NIPER 2024 (MS/M.Pharm) and AIR 27 in NIPER MBA, along with AIR 147 in GPAT 2024 and AIR 907 in GPAT 2023. I also achieved AIR 6 in AIIMS CRE-2025 for Drug Store Keeper and was selected as a Pharmacist (AIR 61) for ESIC. Additionally, I was the Runner-Up in Round 2 of the EY Case Study Competition.
At PharmacyFreak.com, I aim to guide future pharmacists through expert content, exam strategies, and insightful resources based on real experience and academic excellence.
Mail- harsh@pharmacyfreak.com