Table of Contents
Introduction
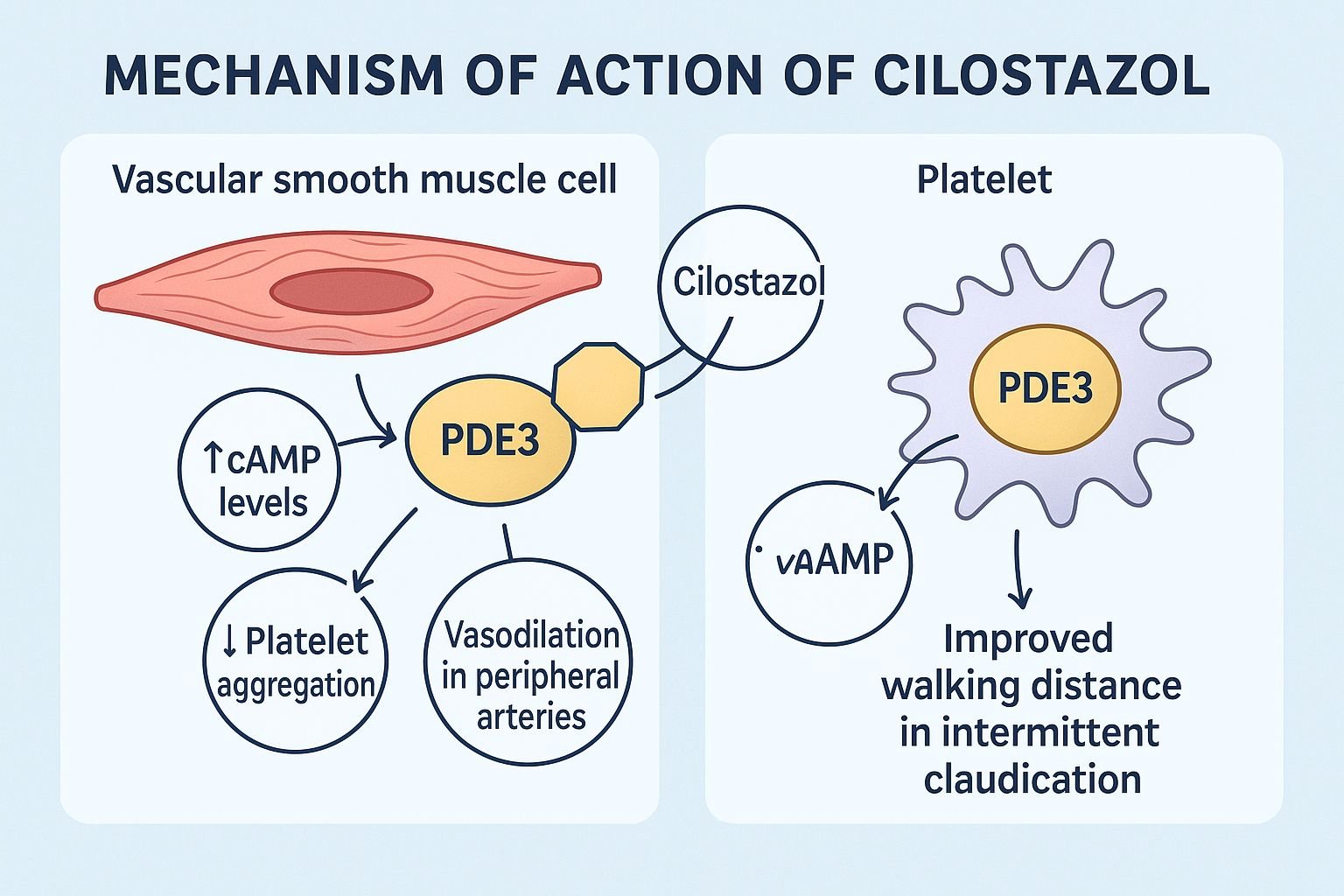
Cilostazol is a phosphodiesterase-3 (PDE3) inhibitor used primarily for the treatment of intermittent claudication caused by peripheral arterial disease (PAD). It improves walking distance and reduces pain by promoting vasodilation and inhibiting platelet aggregation.
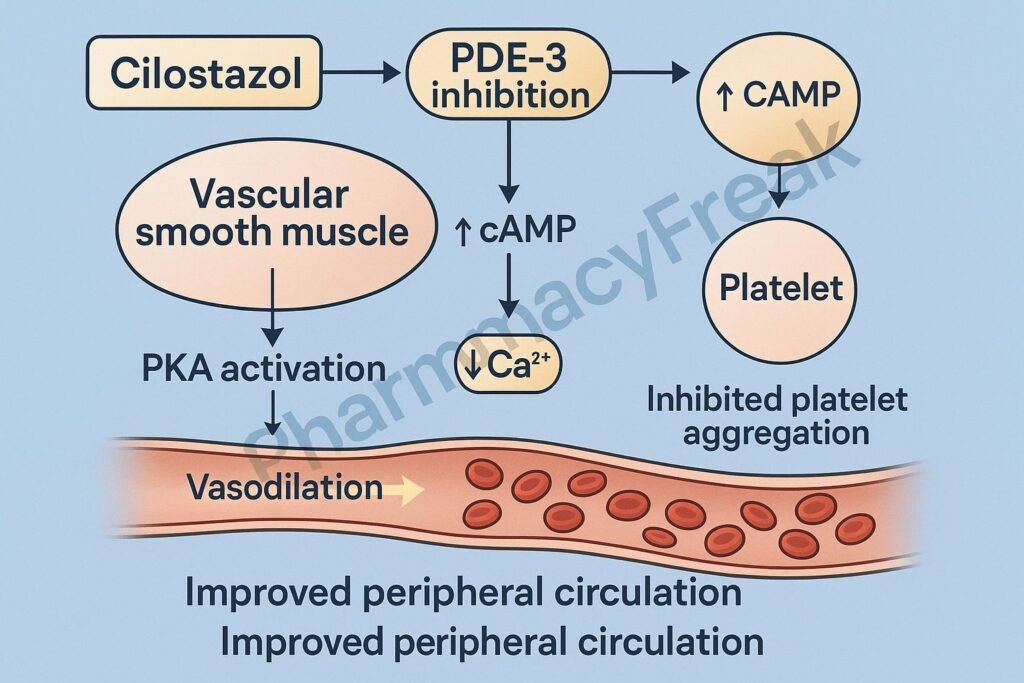
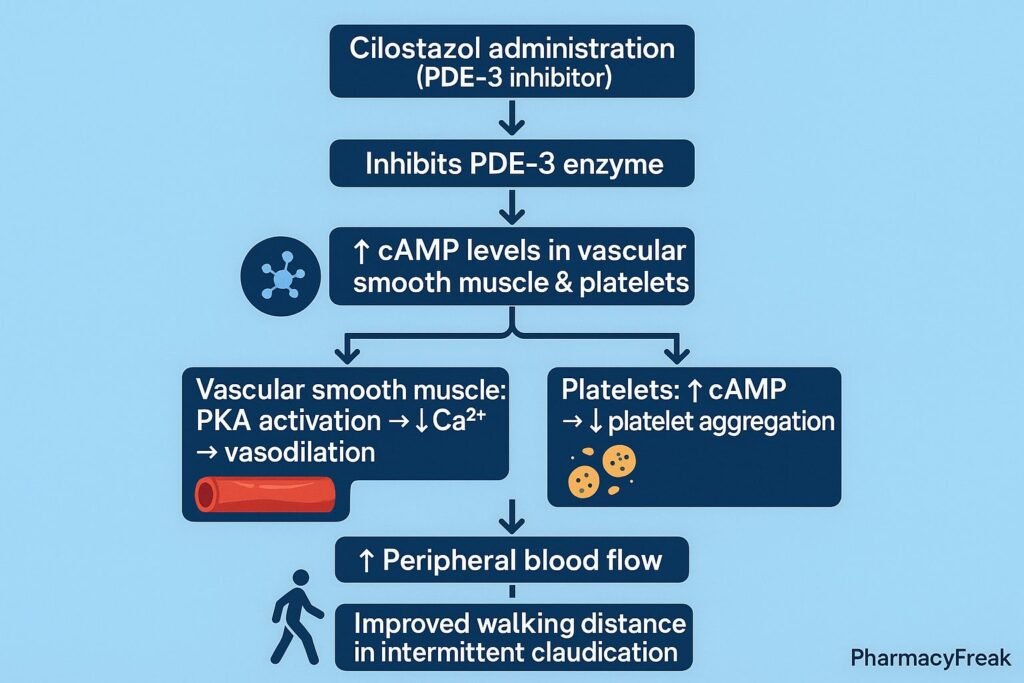
The Mechanism of Action of Cilostazol involves inhibition of PDE3, resulting in increased cyclic adenosine monophosphate (cAMP) levels in platelets and vascular smooth muscle, leading to antiplatelet activity and vasodilation.
Mechanism of Action (Step-wise)
1. Inhibition of Phosphodiesterase-3 (PDE3) – Primary Mechanism
Cilostazol selectively inhibits PDE3, the enzyme responsible for degrading cAMP.
Effects:
- ↑ Intracellular cAMP
- Enhanced cAMP-mediated signaling in platelets and vascular smooth muscle
This is the central mechanism responsible for its dual actions.
2. Inhibition of Platelet Aggregation
Increased platelet cAMP leads to:
- ↓ Release of granules (ADP, serotonin)
- ↓ Activation of GPIIb/IIIa receptors
- ↓ Platelet aggregation
Thus, cilostazol acts as an antiplatelet agent.
3. Vasodilation of Peripheral Arteries
Elevated cAMP in vascular smooth muscle:
- Activates protein kinase A (PKA)
- Inhibits myosin light chain kinase (MLCK)
- Promotes smooth muscle relaxation
Result:
- Vasodilation
- Improved blood flow in peripheral arteries
Improved perfusion reduces symptoms of claudication.
4. Inhibition of Vascular Smooth Muscle Proliferation
Cilostazol reduces:
- Proliferation of smooth muscle cells
- Neointimal hyperplasia
This may help prevent restenosis after vascular interventions.
5. Improvement in Lipid Profile (Secondary Effect)
Cilostazol modestly:
- ↑ HDL levels
- ↓ Triglycerides
These contribute to long-term vascular health.
6. Summary of Mechanism
| Mechanism | Effect |
|---|---|
| PDE3 inhibition | ↑ cAMP |
| Platelet inhibition | ↓ Aggregation |
| Vasodilation | Improved peripheral blood flow |
| ↓ Smooth muscle proliferation | Less restenosis |
| Minor lipid improvement | Cardioprotective |
Pharmacokinetics
- Absorption: Good oral absorption
- Metabolism: Hepatic via CYP3A4 and CYP2C19
- Half-life: ~11–13 hours
- Excretion: Renal and fecal
- Steady-state: Reached in 4 days
Clinical Uses
- Intermittent claudication (first-line pharmacotherapy)
- Secondary prevention in peripheral arterial disease
- Adjunct to reduce restenosis after angioplasty (off-label)
Adverse Effects
Common
- Headache
- Palpitations
- Diarrhea
- Dizziness
- Peripheral edema
Serious
- Tachyarrhythmias
- Thrombocytopenia
- Agranulocytosis (rare)
Contraindications
- Heart failure (absolute contraindication)
PDE3 inhibitors increase mortality in HF patients. - Severe hepatic or renal impairment
- Bleeding disorders
- Concomitant use with strong CYP3A4 inhibitors or inducers

Comparative Analysis
| Feature | Cilostazol | Clopidogrel | Aspirin |
|---|---|---|---|
| Mechanism | PDE3 inhibitor | P2Y12 inhibitor | COX-1 inhibitor |
| Vasodilation | Yes | No | No |
| Effect on walking distance | Strongest | Minimal | Minimal |
| HF contraindication | Yes | No | No |
MCQs
1. Cilostazol acts by inhibiting:
a) PDE5
b) PDE3
c) COX-1
d) ADP receptor
Answer: b) PDE3
2. Increased cAMP in platelets leads to:
a) Increased aggregation
b) Decreased aggregation
c) Increased serotonin release
d) Vasoconstriction
Answer: b) Decreased aggregation
3. Cilostazol is contraindicated in:
a) Diabetes
b) Hypertension
c) Heart failure
d) Gastritis
Answer: c) Heart failure
4. Cilostazol improves walking distance in PAD mainly by:
a) Increasing RBC count
b) Vasodilation and antiplatelet effects
c) Increasing heart rate
d) Enhancing oxygen extraction
Answer: b) Vasodilation and antiplatelet effects
5. Cilostazol metabolism occurs primarily via:
a) CYP1A2
b) CYP3A4 and CYP2C19
c) CYP2D6
d) CYP7A1
Answer: b) CYP3A4 and CYP2C19
FAQs
Q1. How long does cilostazol take to improve symptoms?
2–4 weeks for noticeable improvement; maximum benefit at ~12 weeks.
Q2. Why is it contraindicated in heart failure?
PDE3 inhibitors increase mortality by worsening arrhythmias and myocardial workload.
Q3. Can cilostazol be combined with aspirin or clopidogrel?
Yes—commonly used in combination for PAD.
Q4. Does cilostazol cause tachycardia?
Yes—due to PDE3 inhibition in cardiac tissue.
Q5. Is cilostazol useful in diabetic PAD?
Yes—one of the most effective pharmacotherapies.
References
Goodman & Gilman’s Pharmacological Basis of Therapeutics
https://accesspharmacy.mhmedical.com/book.aspx?bookid=2189
Katzung: Basic and Clinical Pharmacology
https://accessmedicine.mhmedical.com/book.aspx?bookid=2464
Tripathi: Essentials of Medical Pharmacology
https://jaypeebrothers.com/
Harrison’s Principles of Internal Medicine
https://accessmedicine.mhmedical.com/book.aspx?bookid=2129

I am pursuing MBA in pharmaceutical management from NIPER Hyderabad with a strong academic record and proven success in national-level pharmacy entrance exams. I secured AIR 61 in NIPER 2024 (MS/M.Pharm) and AIR 27 in NIPER MBA, along with AIR 147 in GPAT 2024 and AIR 907 in GPAT 2023. I also achieved AIR 6 in AIIMS CRE-2025 for Drug Store Keeper and was selected as a Pharmacist (AIR 61) for ESIC. Additionally, I was the Runner-Up in Round 2 of the EY Case Study Competition.
At PharmacyFreak.com, I aim to guide future pharmacists through expert content, exam strategies, and insightful resources based on real experience and academic excellence.
Mail- harsh@pharmacyfreak.com