Table of Contents
Introduction
Bupivacaine is a long-acting amide-type local anesthetic widely used for regional anesthesia, epidural anesthesia, nerve blocks, infiltration anesthesia, and obstetric analgesia. It is known for its high potency, long duration of action, and strong sensory blockade. Because of its strong affinity for cardiac sodium channels, it carries a higher risk of cardiotoxicity compared to other local anesthetics.
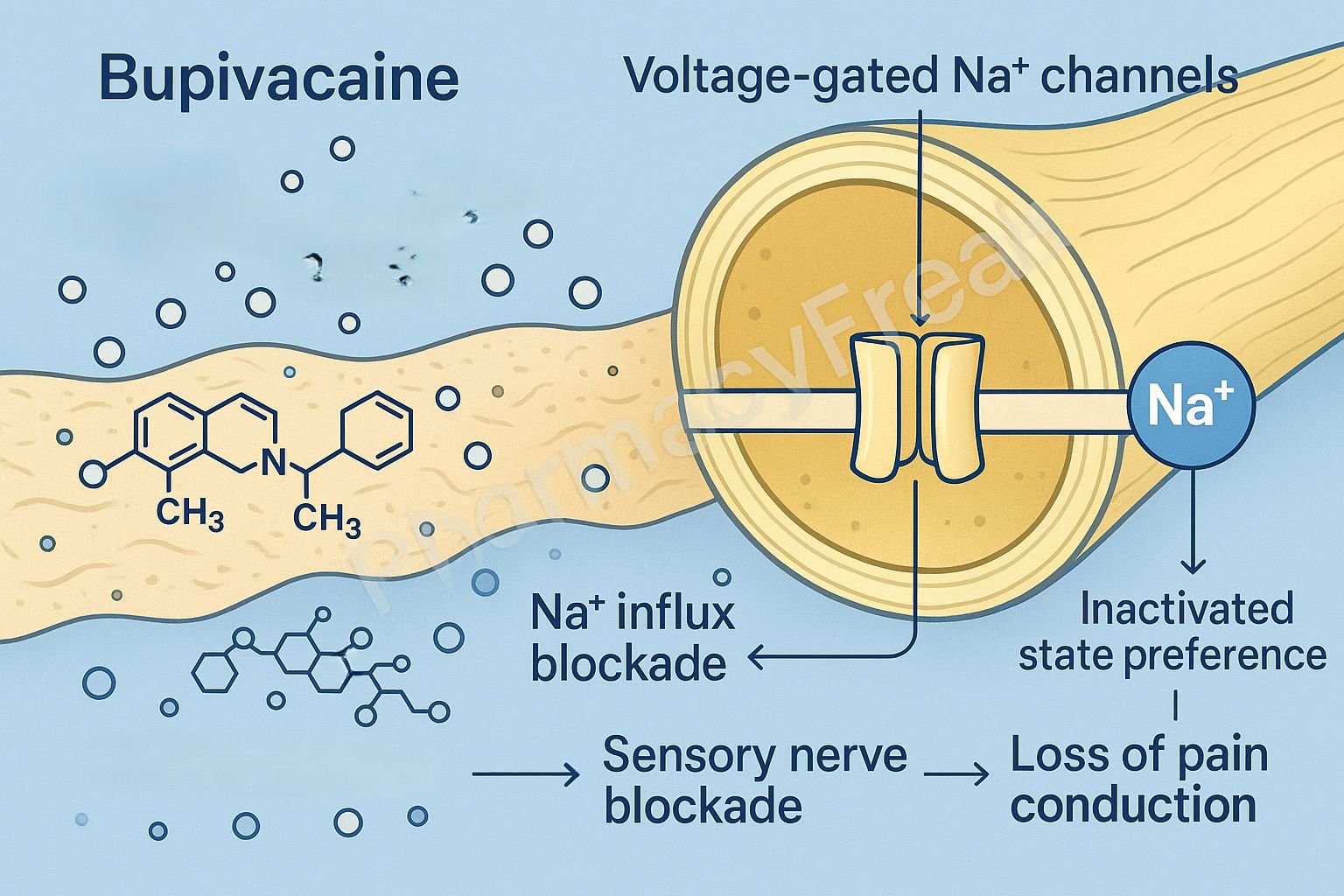
The Mechanism of Action of Bupivacaine centers on reversible inhibition of voltage-gated sodium channels, preventing nerve depolarization and propagation of action potentials.


Mechanism of Action (Step-wise)
1. Binding to Voltage-Gated Sodium (Na⁺) Channels – Primary Mechanism
Bupivacaine enters nerve cells in its uncharged (lipid-soluble) form, then converts into its charged form and binds from the intracellular side to voltage-gated Na⁺ channels (Nav1.x).
Results:
- ↓ Na⁺ influx
- ↓ Rate of depolarization
- Blocked action potential initiation
- Blocked action potential propagation
Effect: Reversible loss of sensation and motor function.
2. Preferential Binding to Active and Inactivated Channels
Bupivacaine has higher affinity for:
- Open (activated) Na⁺ channels
- Inactivated Na⁺ channels
This produces use-dependent block, meaning greater blockade in rapidly firing nerves (pain fibers).
3. Differential Blockade of Nerve Fibers
Sensitivity of nerve fibers to bupivacaine:
- B > C > Aδ > Aγ > Aβ > Aα
- B fibers: autonomic
- C fibers: pain and temperature
- A fibers: motor and proprioception
Result:
- Pain blocked first
- Motor block occurs later and is less intense
4. Long Duration of Action
Bupivacaine is:
- Highly lipid-soluble
- Highly protein-bound (95%)
This prolongs residence in nerve tissue and extends anesthetic duration to 3–8 hours, depending on site.
5. Cardiotoxicity Mechanism (Important)
Bupivacaine binds strongly to cardiac Na⁺ channels and dissociates slowly.
Effects:
- ↓ Cardiac conduction
- QRS widening
- Ventricular arrhythmias
- Myocardial depression
Lipid emulsion therapy is used to treat toxicity.

6. Summary of Mechanism
| Mechanism | Effect |
|---|---|
| Na⁺ channel blockade | Prevents depolarization |
| Use-dependent block | Strong effect on pain fibers |
| High lipid solubility | Long duration |
| Cardiac Na⁺ channel binding | Risk of cardiotoxicity |
Pharmacokinetics
- Class: Amide local anesthetic
- Onset: 5–10 minutes
- Duration: 3–8 hours (long-acting)
- Protein binding: ~95%
- Metabolism: Hepatic (CYP3A4 and CYP1A2)
- Elimination: Renal
Clinical Uses
- Epidural anesthesia
- Spinal anesthesia
- Peripheral nerve blocks
- Caudal blocks
- Obstetric analgesia (low-concentration bupivacaine)
- Infiltration anesthesia
Adverse Effects
Local Anesthetic Systemic Toxicity (LAST)
- CNS: tinnitus, metallic taste, seizures
- CVS:
- Severe cardiotoxicity
- Ventricular arrhythmias
- Cardiac arrest
Other Effects
- Hypotension
- Bradycardia
- Respiratory depression (with high doses)
- Allergic reactions (rare in amide anesthetics)
Contraindications
- History of amide anesthetic allergy
- Severe hepatic impairment
- Existing cardiac conduction abnormalities (caution)
- Pregnancy (high concentration epidurals avoided due to cardiotoxicity risk)
Comparative Analysis
| Feature | Bupivacaine | Lidocaine | Ropivacaine |
|---|---|---|---|
| Duration | Long | Medium | Long |
| Potency | High | Moderate | High |
| Cardiotoxicity | Highest | Low | Lower |
| Use | Epidural/nerve block | Infiltration, IV regional | Labor analgesia, nerve block |
MCQs
1. Bupivacaine primarily blocks which channel?
a) Calcium channels
b) Sodium channels
c) Potassium channels
d) Chloride channels
Answer: b) Sodium channels
2. Bupivacaine exhibits high affinity for:
a) Closed Na⁺ channels
b) Open and inactivated Na⁺ channels
c) Calcium channels only
d) AMPA receptors
Answer: b) Open and inactivated Na⁺ channels
3. A major toxicity associated with bupivacaine is:
a) Nephrotoxicity
b) Cardiotoxicity
c) Hepatotoxicity
d) Pneumonitis
Answer: b) Cardiotoxicity
4. Bupivacaine duration is prolonged because of:
a) Low protein binding
b) Low lipid solubility
c) High protein binding and lipid solubility
d) Rapid metabolism
Answer: c) High protein binding and lipid solubility
5. Which fiber is blocked earliest by bupivacaine?
a) Aα
b) Aβ
c) C fibers
d) Aδ fibers
Answer: c) C fibers
FAQs
Q1. Why is bupivacaine avoided in IV regional anesthesia (Bier’s block)?
Due to severe cardiotoxicity risk.
Q2. Is bupivacaine safe for obstetric anesthesia?
Yes—low concentrations are used safely for epidurals.
Q3. What is the antidote for bupivacaine toxicity?
20% lipid emulsion therapy (Intralipid).
Q4. Does bupivacaine cause vasodilation or vasoconstriction?
It generally causes vasodilation, enhancing absorption.
Q5. How does bupivacaine compare with ropivacaine?
Ropivacaine is similar but less cardiotoxic.
References
Goodman & Gilman’s Pharmacological Basis of Therapeutics
https://accesspharmacy.mhmedical.com/book.aspx?bookid=2189
Katzung: Basic and Clinical Pharmacology
https://accessmedicine.mhmedical.com/book.aspx?bookid=2464
Tripathi: Essentials of Medical Pharmacology
https://jaypeebrothers.com/
Harrison’s Principles of Internal Medicine
https://accessmedicine.mhmedical.com/book.aspx?bookid=2129

I am pursuing MBA in pharmaceutical management from NIPER Hyderabad with a strong academic record and proven success in national-level pharmacy entrance exams. I secured AIR 61 in NIPER 2024 (MS/M.Pharm) and AIR 27 in NIPER MBA, along with AIR 147 in GPAT 2024 and AIR 907 in GPAT 2023. I also achieved AIR 6 in AIIMS CRE-2025 for Drug Store Keeper and was selected as a Pharmacist (AIR 61) for ESIC. Additionally, I was the Runner-Up in Round 2 of the EY Case Study Competition.
At PharmacyFreak.com, I aim to guide future pharmacists through expert content, exam strategies, and insightful resources based on real experience and academic excellence.
Mail- harsh@pharmacyfreak.com