Table of Contents
Introduction
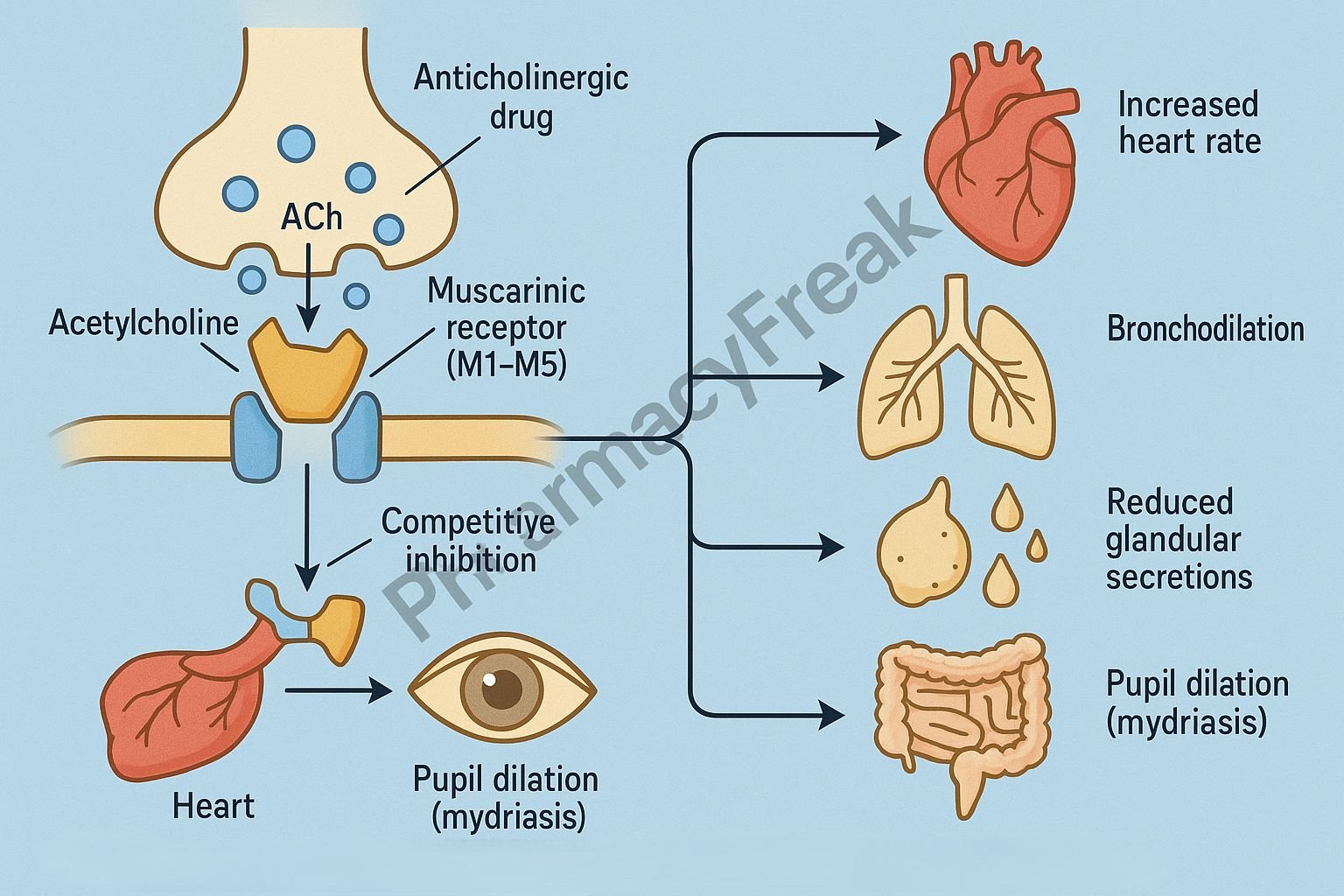
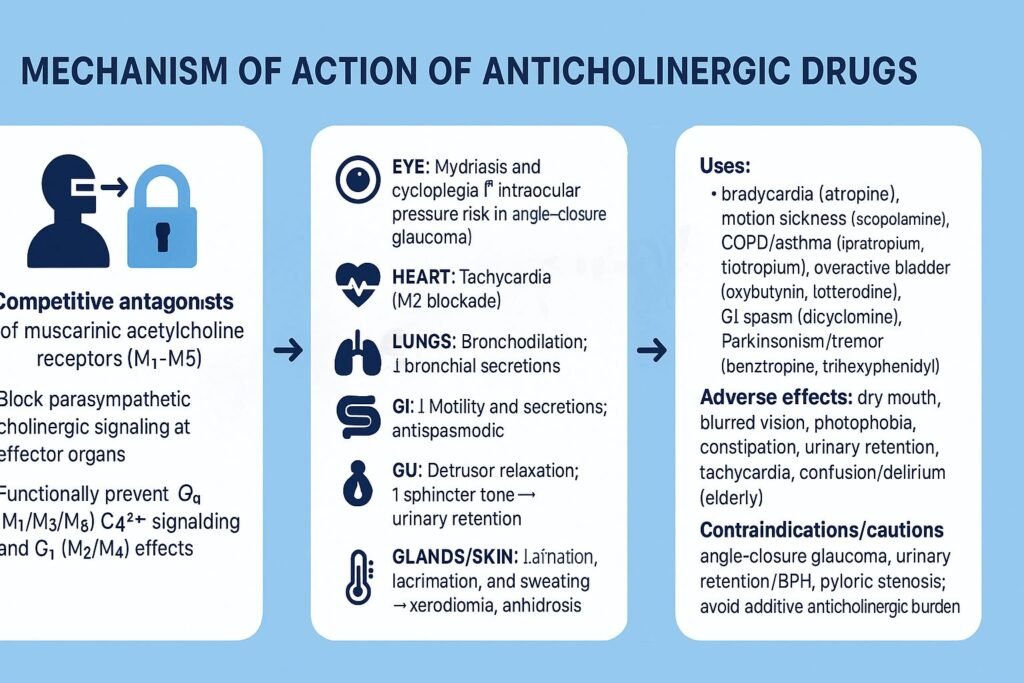
Anticholinergic drugs, also known as parasympatholytic agents, inhibit the actions of the neurotransmitter acetylcholine (ACh) at muscarinic receptors in the central and peripheral nervous systems. Mechanism of Action of Anticholinergic Drugs involves competitive antagonism of acetylcholine at muscarinic (M1–M5) receptor sites, thereby reducing parasympathetic activity. These drugs are used to treat disorders such as bronchial asthma, COPD, peptic ulcer disease, motion sickness, Parkinson’s disease, and urinary incontinence.

Mechanism of Action (Step-wise)
- Blockade of Muscarinic Receptors
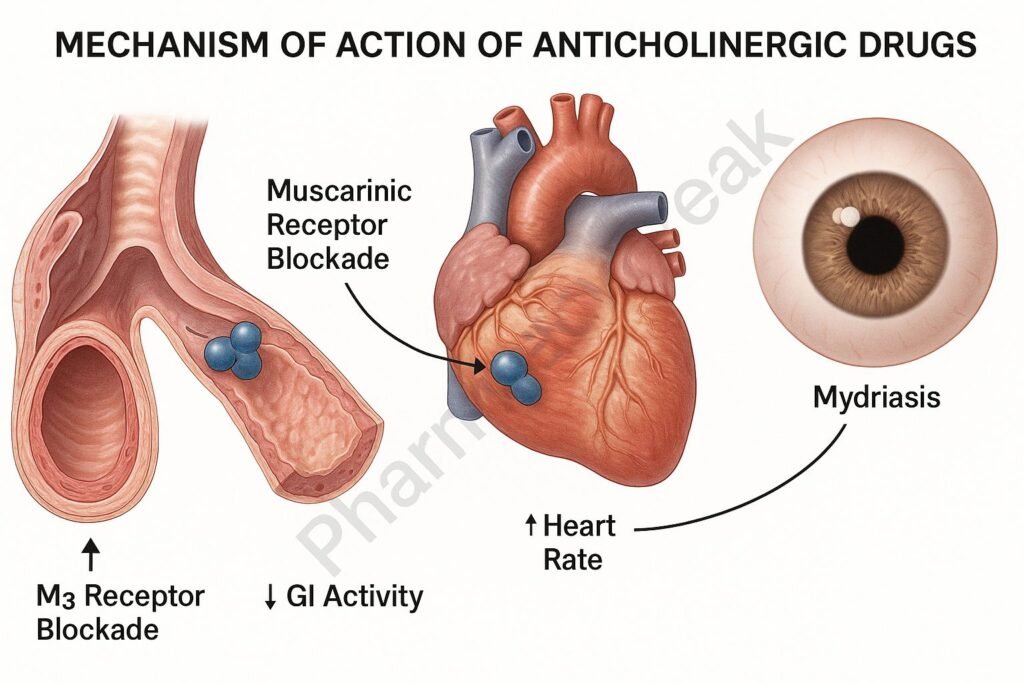
- Anticholinergic drugs competitively block acetylcholine from binding to muscarinic receptors located in smooth muscle, cardiac muscle, and glands.
- The receptors affected include:
- M1 (neural): Gastric parietal cells and CNS
- M2 (cardiac): Heart (SA and AV nodes)
- M3 (glandular/smooth muscle): Airways, eyes, GIT, bladder, glands
- Inhibition of Parasympathetic Nerve Function
- By preventing ACh binding, these drugs inhibit parasympathetic (cholinergic) impulses.
- This leads to decreased glandular secretions, smooth muscle relaxation, and pupil dilation (mydriasis).
- Reduction in Glandular Secretions
- In salivary glands → decreased saliva → dry mouth
- In gastric glands → reduced gastric acid → anti-ulcer effect
- In respiratory tract → reduced mucus → improved airflow in COPD/asthma
- Smooth Muscle Relaxation
- In bronchi → bronchodilation (Ipratropium, Tiotropium)
- In bladder → reduced detrusor contraction (Oxybutynin, Tolterodine)
- In GI tract → decreased motility (Hyoscine, Dicyclomine)
- Cardiac Effects
- Blockade of vagal stimulation → tachycardia and increased cardiac output
- Used in bradycardia management (e.g., Atropine).
- CNS Effects
- Centrally acting agents like Trihexyphenidyl and Benztropine restore the dopamine–acetylcholine balance in Parkinson’s disease.
- Scopolamine blocks cholinergic transmission in the vestibular nuclei, reducing motion sickness symptoms.
- Overall Effects
- ↓ Secretions + ↑ Heart Rate + Smooth Muscle Relaxation + CNS Modulation → Parasympathetic inhibition and symptom relief.

Pharmacokinetics
- Absorption: Good oral absorption; some agents used topically (e.g., eye drops) or by inhalation.
- Distribution: Widely distributed; lipid-soluble drugs cross the blood-brain barrier.
- Metabolism: Primarily hepatic.
- Excretion: Renal (as metabolites or unchanged drug).
- Half-life: Varies (short for ipratropium, long for atropine or tiotropium).
Clinical Uses
- Respiratory: COPD, bronchial asthma (Ipratropium, Tiotropium).
- Cardiac: Sinus bradycardia, AV block (Atropine).
- Gastrointestinal: Peptic ulcer disease, IBS (Hyoscine, Dicyclomine).
- Urinary tract: Overactive bladder, urinary incontinence (Oxybutynin, Tolterodine, Solifenacin).
- Neurological: Parkinson’s disease (Benztropine, Trihexyphenidyl).
- Ophthalmic: Mydriasis for eye exams (Tropicamide, Atropine).
- Anesthesia adjunct: Reduce salivation and bronchial secretions (Glycopyrrolate, Atropine).
- Motion sickness: Scopolamine patches.
Adverse Effects
- Dry mouth (xerostomia)
- Blurred vision (due to mydriasis and cycloplegia)
- Constipation
- Urinary retention
- Tachycardia
- Confusion, hallucinations (especially in elderly due to CNS effects)
- Hyperthermia (due to inhibition of sweating)
- Contraindications: Glaucoma, prostatic hypertrophy, paralytic ileus.
Comparative Analysis
| Drug | Main Action | Clinical Use | Notable Adverse Effect |
|---|---|---|---|
| Atropine | Muscarinic blocker (non-selective) | Bradycardia, organophosphate poisoning | Tachycardia, dry mouth |
| Ipratropium | M3 blockade in bronchi | COPD, asthma | Dry mouth |
| Oxybutynin | M3 blockade in bladder | Overactive bladder | Urinary retention |
| Scopolamine | CNS blockade | Motion sickness | Sedation, confusion |
| Trihexyphenidyl | Central M blockade | Parkinson’s disease | Confusion, blurred vision |
MCQs
1. Anticholinergic drugs act by:
a) Stimulating muscarinic receptors
b) Blocking muscarinic receptors
c) Blocking nicotinic receptors
d) Stimulating acetylcholine release
Answer: b) Blocking muscarinic receptors
2. Atropine acts on which receptor type?
a) Nicotinic
b) Muscarinic
c) Dopaminergic
d) Adrenergic
Answer: b) Muscarinic
3. Which of the following is used in motion sickness?
a) Atropine
b) Scopolamine
c) Ipratropium
d) Oxybutynin
Answer: b) Scopolamine
4. The anticholinergic used in COPD is:
a) Glycopyrrolate
b) Ipratropium
c) Tropicamide
d) Atropine
Answer: b) Ipratropium
5. Anticholinergic drugs cause:
a) Miosis
b) Bradycardia
c) Dry mouth and tachycardia
d) Salivation and sweating
Answer: c) Dry mouth and tachycardia
6. Which anticholinergic crosses the blood-brain barrier most easily?
a) Atropine
b) Glycopyrrolate
c) Ipratropium
d) Tiotropium
Answer: a) Atropine
7. The mechanism of action of oxybutynin is:
a) Beta-3 receptor activation
b) Muscarinic receptor blockade (M3)
c) Dopamine receptor activation
d) Alpha receptor blockade
Answer: b) Muscarinic receptor blockade (M3)
8. A patient with glaucoma should avoid:
a) Beta-blockers
b) Anticholinergics
c) Alpha-agonists
d) ACE inhibitors
Answer: b) Anticholinergics
9. Which effect is caused by anticholinergics in the eye?
a) Miosis
b) Mydriasis and cycloplegia
c) Lacrimation
d) Accommodation for near vision
Answer: b) Mydriasis and cycloplegia
10. Anticholinergics are contraindicated in:
a) Diarrhea
b) Prostatic hypertrophy
c) Parkinson’s disease
d) Bradycardia
Answer: b) Prostatic hypertrophy
FAQs
Q1. What are anticholinergic drugs?
They are agents that block the effects of acetylcholine at muscarinic receptors in the CNS and PNS.
Q2. What are the main effects of anticholinergics?
Reduced secretions, bronchodilation, mydriasis, increased heart rate, and decreased GI and urinary motility.
Q3. Why are they called parasympatholytic drugs?
Because they inhibit parasympathetic nerve activity, opposing acetylcholine’s effects.
Q4. Which anticholinergic is used in Parkinson’s disease?
Trihexyphenidyl or Benztropine help correct cholinergic–dopaminergic imbalance.
Q5. What are common side effects of anticholinergics?
Dry mouth, blurred vision, constipation, tachycardia, and urinary retention.
Q6. Can anticholinergics be used in elderly patients?
Caution is required as they may cause confusion and memory impairment.
References
- Goodman & Gilman’s The Pharmacological Basis of Therapeutics
- Katzung’s Basic and Clinical Pharmacology
- Rang & Dale’s Pharmacology
- Harrison’s Principles of Internal Medicine
Related Internal Links

I am pursuing MBA in pharmaceutical management from NIPER Hyderabad with a strong academic record and proven success in national-level pharmacy entrance exams. I secured AIR 61 in NIPER 2024 (MS/M.Pharm) and AIR 27 in NIPER MBA, along with AIR 147 in GPAT 2024 and AIR 907 in GPAT 2023. I also achieved AIR 6 in AIIMS CRE-2025 for Drug Store Keeper and was selected as a Pharmacist (AIR 61) for ESIC. Additionally, I was the Runner-Up in Round 2 of the EY Case Study Competition.
At PharmacyFreak.com, I aim to guide future pharmacists through expert content, exam strategies, and insightful resources based on real experience and academic excellence.
Mail- harsh@pharmacyfreak.com