Table of Contents
Introduction
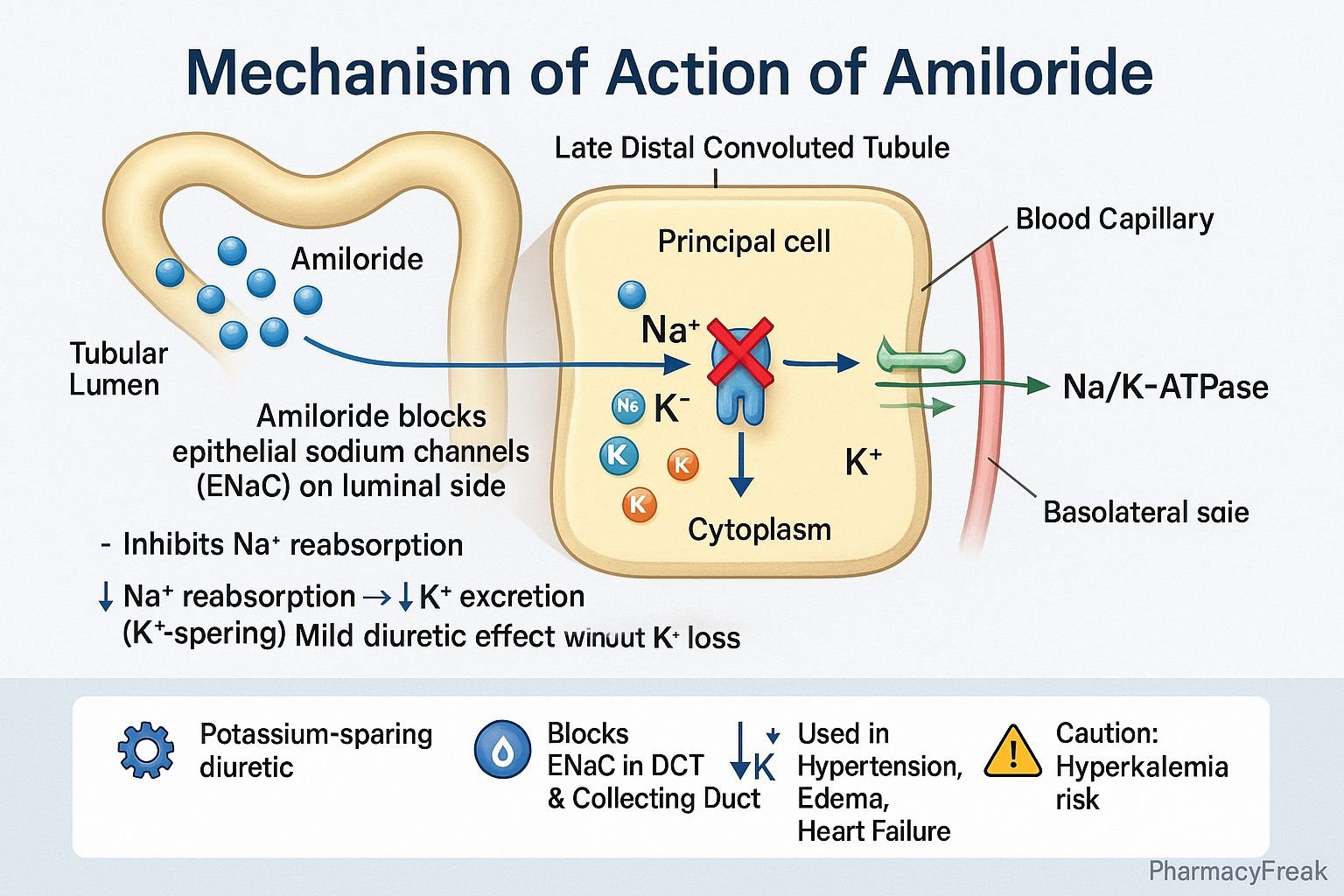
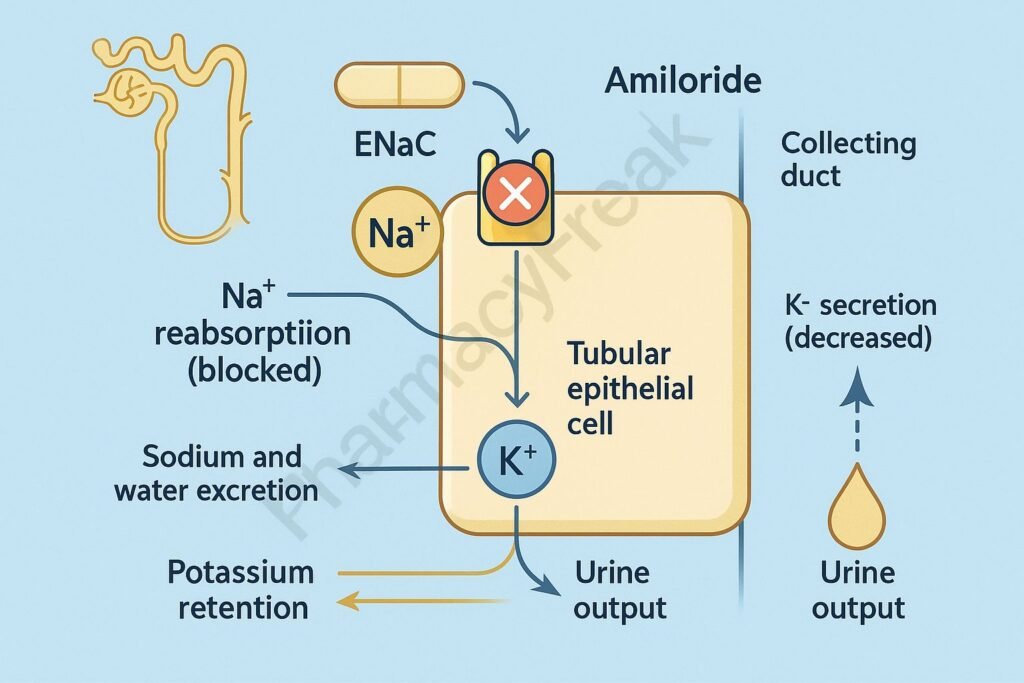
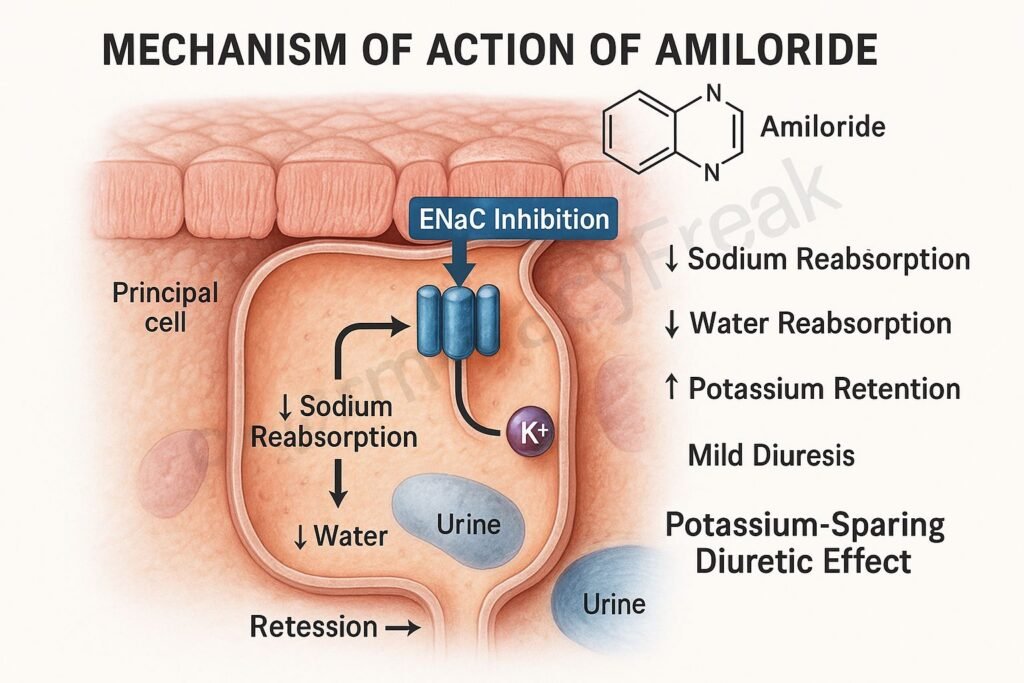
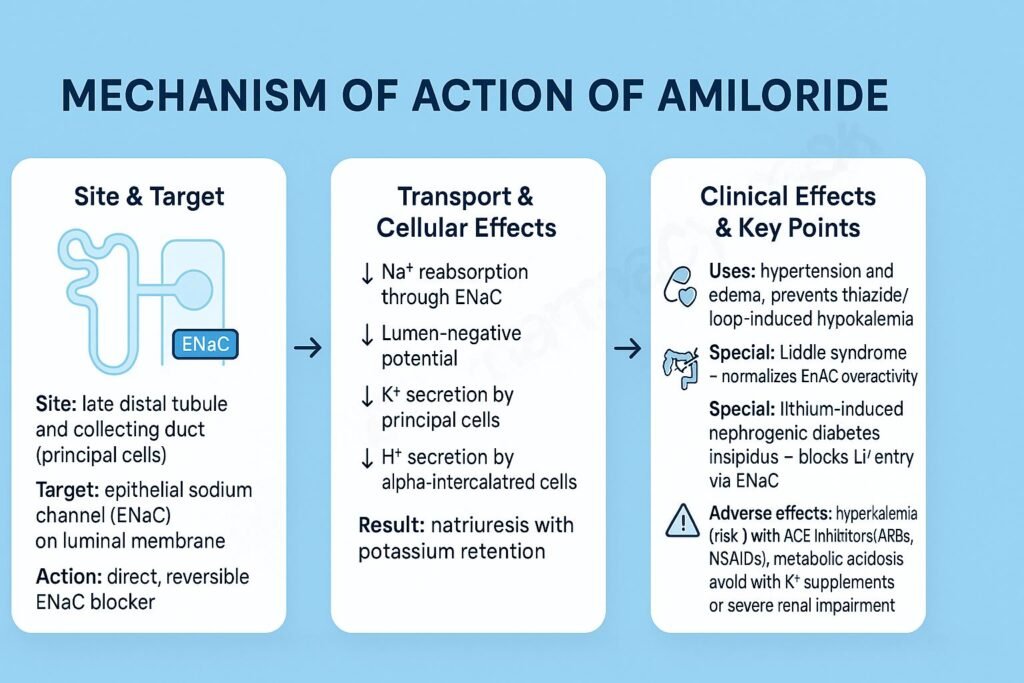
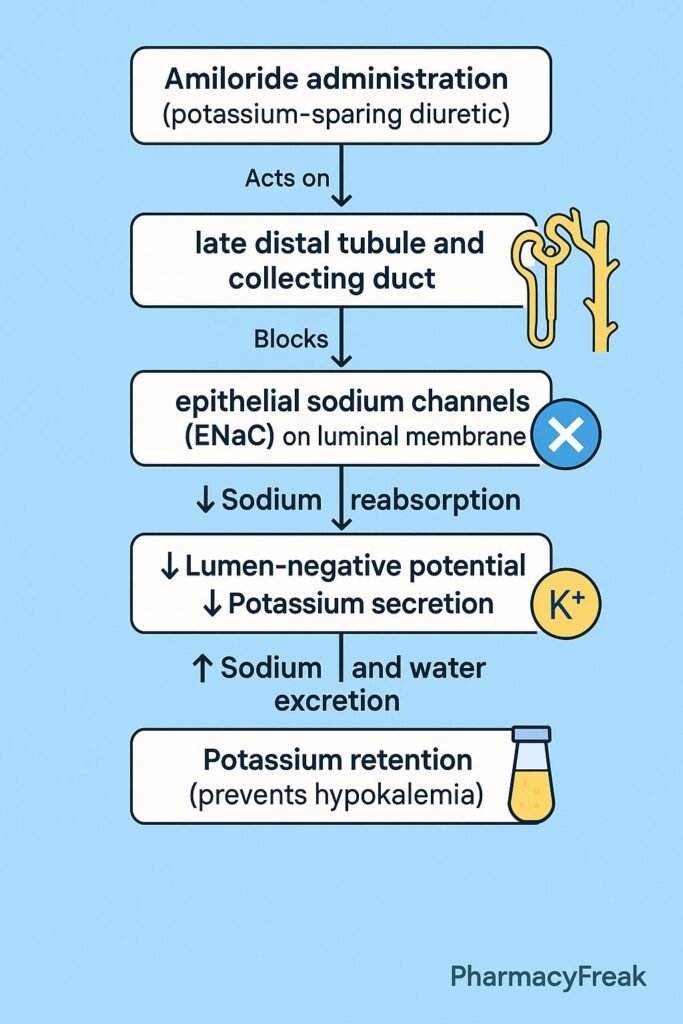
Amiloride is a potassium-sparing diuretic that acts on the distal nephron of the kidney to promote sodium excretion while conserving potassium. Mechanism of Action of Amiloride involves direct inhibition of epithelial sodium channels (ENaC) in the late distal tubule and collecting duct, leading to decreased sodium reabsorption and reduced potassium excretion. Unlike aldosterone antagonists such as spironolactone, amiloride acts independently of aldosterone. It is primarily used in the management of hypertension, heart failure, and edematous conditions, often in combination with thiazide or loop diuretics to prevent hypokalemia.
Mechanism of Action (Step-wise)
- Site of Action – Distal Nephron
- Amiloride acts on the luminal side of principal cells in the late distal convoluted tubule and collecting duct of the nephron.
- Blockade of Epithelial Sodium Channels (ENaC)
- It directly blocks ENaC channels, preventing sodium ions (Na⁺) from entering tubular epithelial cells from the tubular lumen.
- Reduced Sodium Reabsorption
- With ENaC blocked, less sodium is reabsorbed into the bloodstream.
- This decreases water reabsorption (since water follows sodium), promoting mild diuresis and natriuresis.
- Decreased Potassium Excretion
- Normally, sodium reabsorption through ENaC generates a negative luminal potential that drives potassium (K⁺) secretion into urine via ROMK channels.
- By inhibiting sodium entry, amiloride reduces this electrical gradient, leading to reduced K⁺ excretion and potassium retention.
- No Effect on Aldosterone
- Amiloride’s action is independent of aldosterone levels—it blocks sodium transport directly rather than altering receptor-mediated mechanisms.
- Overall Effect
- ↓ Na⁺ reabsorption → ↓ H₂O reabsorption → Mild diuresis
- ↓ K⁺ secretion → Potassium retention
- Maintains electrolyte balance while avoiding hypokalemia.
Pharmacokinetics
- Absorption: ~50% orally bioavailable.
- Onset of action: Within 2 hours of oral dose.
- Distribution: Concentrated in renal tubular cells.
- Metabolism: Not significantly metabolized.
- Excretion: Primarily excreted unchanged in urine.
- Half-life: 6–9 hours (may extend up to 20 hours in renal impairment).
Clinical Uses
- Edema and hypertension: Usually in combination with thiazide or loop diuretics.
- Heart failure: To prevent potassium loss during diuretic therapy.
- Liddle’s syndrome: Effective due to direct ENaC inhibition.
- Cystic fibrosis (experimental use): Reduces airway sodium absorption.
- Prevention of diuretic-induced hypokalemia.
Adverse Effects
- Common: Nausea, vomiting, headache, mild dizziness.
- Serious: Hyperkalemia (especially in renal impairment or when combined with ACE inhibitors or potassium supplements).
- Rare: Hyponatremia, metabolic acidosis, rash.
- Contraindications:
- Renal failure or anuria
- Pre-existing hyperkalemia
- Concurrent use with potassium supplements or other potassium-sparing agents
Comparative Analysis
| Feature | Amiloride | Spironolactone | Triamterene |
|---|---|---|---|
| Mechanism | ENaC channel blocker | Aldosterone receptor antagonist | ENaC channel blocker |
| Site of action | Collecting duct | Collecting duct | Collecting duct |
| Potassium effect | Potassium-sparing | Potassium-sparing | Potassium-sparing |
| Aldosterone dependence | Independent | Dependent | Independent |
| Major adverse effect | Hyperkalemia | Gynecomastia (due to steroid structure) | Hyperkalemia |
MCQs
1. Amiloride acts on which part of the nephron?
a) Proximal convoluted tubule
b) Loop of Henle
c) Distal convoluted tubule and collecting duct
d) Glomerulus
Answer: c) Distal convoluted tubule and collecting duct
2. The main mechanism of amiloride is:
a) Inhibition of aldosterone synthesis
b) Blockade of ENaC channels
c) Inhibition of Na⁺/K⁺-ATPase
d) Osmotic diuresis
Answer: b) Blockade of ENaC channels
3. Amiloride is classified as:
a) Thiazide diuretic
b) Loop diuretic
c) Potassium-sparing diuretic
d) Osmotic diuretic
Answer: c) Potassium-sparing diuretic
4. Amiloride prevents loss of which ion?
a) Sodium
b) Calcium
c) Potassium
d) Chloride
Answer: c) Potassium
5. Amiloride differs from spironolactone because it:
a) Acts on ENaC channels directly
b) Requires aldosterone for action
c) Causes gynecomastia
d) Is metabolized hepatically
Answer: a) Acts on ENaC channels directly
6. A major adverse effect of amiloride is:
a) Hypokalemia
b) Hyperkalemia
c) Hypernatremia
d) Hypocalcemia
Answer: b) Hyperkalemia
7. Amiloride should not be used with:
a) Loop diuretics
b) ACE inhibitors
c) Thiazides
d) Calcium channel blockers
Answer: b) ACE inhibitors
8. Amiloride’s diuretic effect is described as:
a) Potent
b) Moderate
c) Mild
d) Osmotic
Answer: c) Mild
9. Which of the following is an aldosterone-independent diuretic?
a) Spironolactone
b) Amiloride
c) Eplerenone
d) Both a and c
Answer: b) Amiloride
10. Amiloride reduces potassium loss by:
a) Blocking Na⁺ reabsorption
b) Blocking K⁺ channels directly
c) Inhibiting aldosterone synthesis
d) Enhancing Na⁺/K⁺-ATPase activity
Answer: a) Blocking Na⁺ reabsorption
FAQs
Q1. What type of diuretic is amiloride?
Amiloride is a potassium-sparing diuretic that inhibits epithelial sodium channels (ENaC).
Q2. How is amiloride different from spironolactone?
Amiloride acts directly on sodium channels, while spironolactone antagonizes aldosterone receptors.
Q3. Why is amiloride often given with thiazides?
To counteract hypokalemia caused by thiazides while maintaining diuretic efficacy.
Q4. What is the most dangerous side effect of amiloride?
Hyperkalemia, which can lead to cardiac arrhythmias.
Q5. Is amiloride effective in Liddle’s syndrome?
Yes, it is the drug of choice as it blocks overactive ENaC channels.
Q6. Can amiloride be used alone in hypertension?
It provides only mild diuresis, so it is mainly used as add-on therapy.
References
- Goodman & Gilman’s The Pharmacological Basis of Therapeutics
- Katzung’s Basic and Clinical Pharmacology
- Harrison’s Principles of Internal Medicine
- Brenner & Rector’s The Kidney
Related Internal Links

I am pursuing MBA in pharmaceutical management from NIPER Hyderabad with a strong academic record and proven success in national-level pharmacy entrance exams. I secured AIR 61 in NIPER 2024 (MS/M.Pharm) and AIR 27 in NIPER MBA, along with AIR 147 in GPAT 2024 and AIR 907 in GPAT 2023. I also achieved AIR 6 in AIIMS CRE-2025 for Drug Store Keeper and was selected as a Pharmacist (AIR 61) for ESIC. Additionally, I was the Runner-Up in Round 2 of the EY Case Study Competition.
At PharmacyFreak.com, I aim to guide future pharmacists through expert content, exam strategies, and insightful resources based on real experience and academic excellence.
Mail- harsh@pharmacyfreak.com