Table of Contents
Introduction
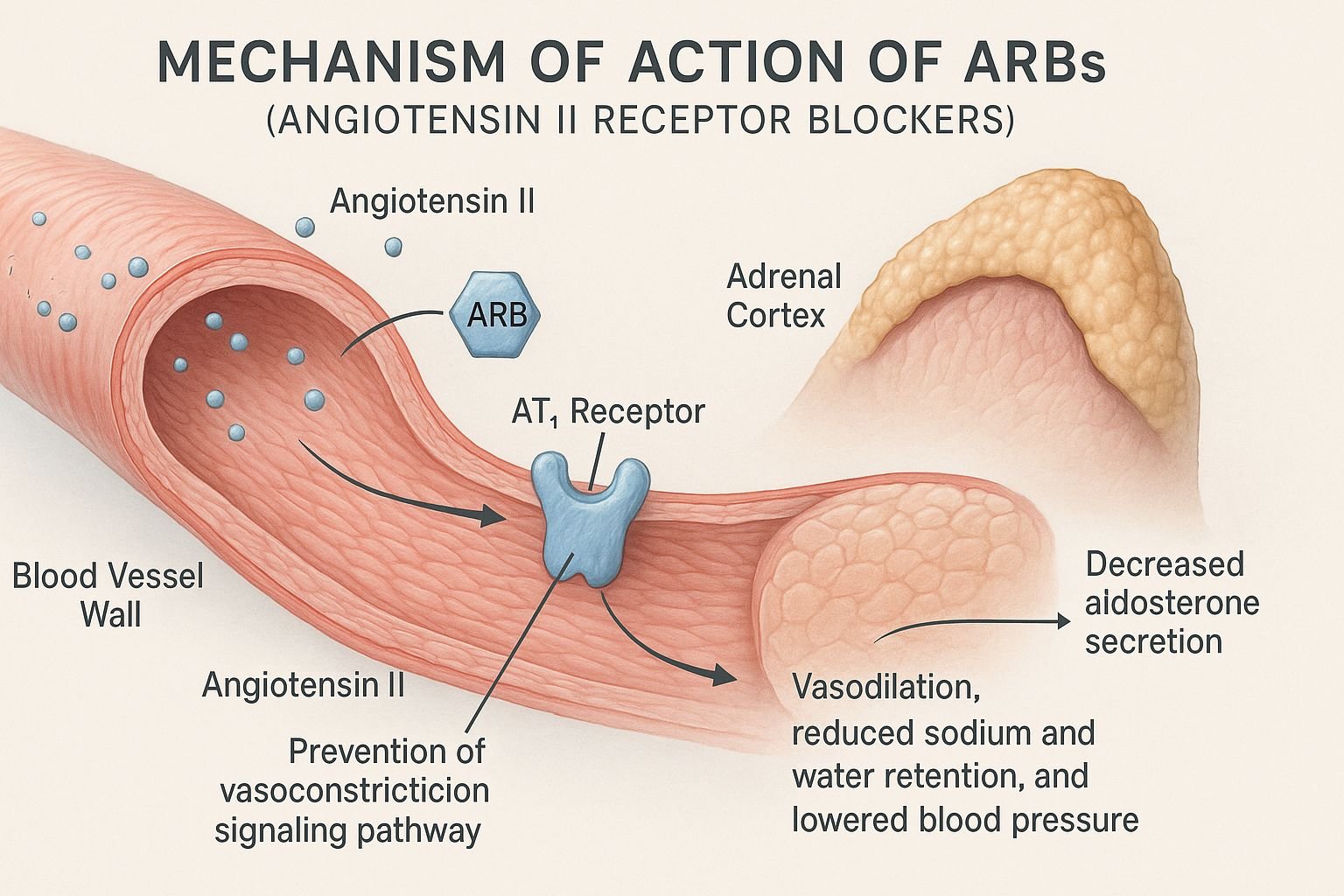
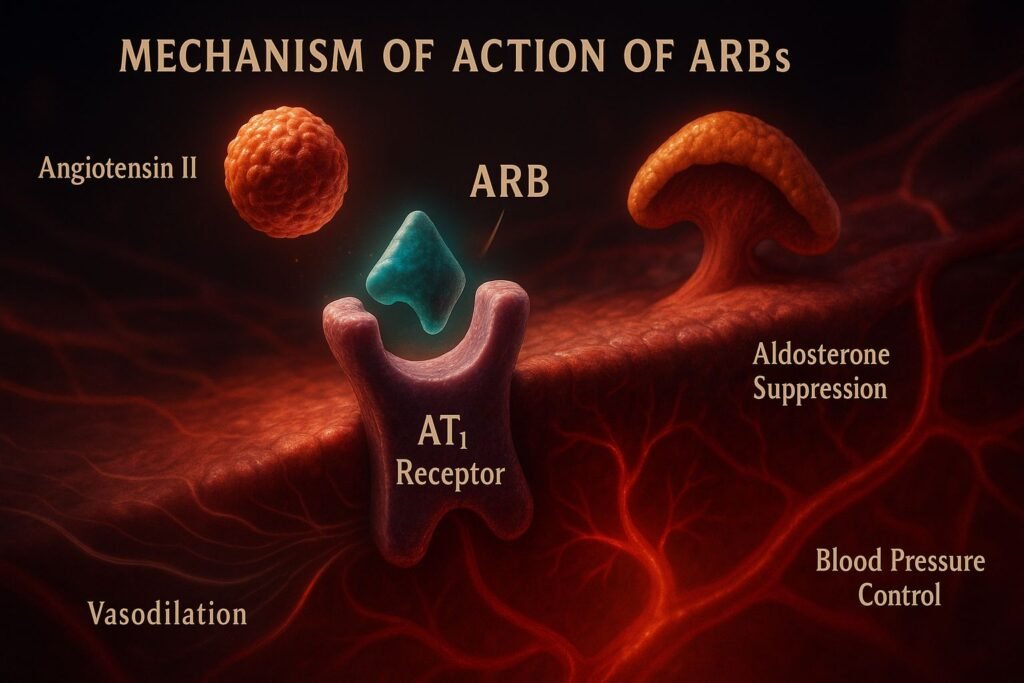
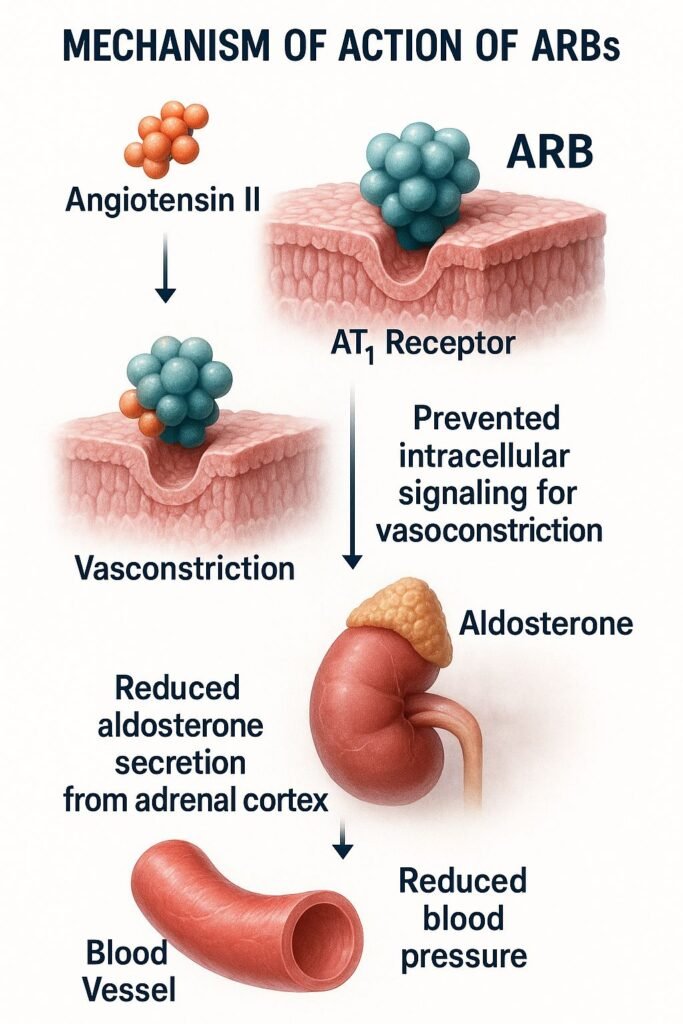
Angiotensin Receptor Blockers (ARBs) are a class of drugs primarily used in the management of hypertension, heart failure, and diabetic nephropathy. They selectively inhibit the binding of angiotensin II to the angiotensin type 1 (AT₁) receptor, providing an alternative to ACE inhibitors with fewer adverse effects like cough and angioedema.
Mechanism of Action (Stepwise)
- Angiotensin II Formation
- Angiotensinogen is converted to angiotensin I by renin.
- Angiotensin I is converted to angiotensin II by ACE.
- Blockade at AT₁ Receptors
- ARBs competitively inhibit angiotensin II from binding to AT₁ receptors located in vascular smooth muscle, adrenal glands, kidneys, and heart.
- Vasodilation
- By blocking vasoconstrictive action of angiotensin II, ARBs induce systemic and renal vasodilation.
- Reduced Aldosterone Secretion
- Blockade leads to decreased aldosterone release, lowering sodium and water retention.
- Preservation of Bradykinin Pathway
- Unlike ACE inhibitors, ARBs do not interfere with bradykinin metabolism, reducing side effects like cough.
Pharmacokinetics
- Absorption: Oral bioavailability varies (13% for losartan to 60% for irbesartan).
- Distribution: Highly plasma protein-bound (more than 90%).
- Metabolism: Hepatic metabolism, primarily by CYP2C9 and CYP3A4 enzymes.
- Half-life: Varies by agent; telmisartan has the longest (~24 hours).
- Excretion: Eliminated via urine and feces.
Clinical Uses
- Hypertension (first-line treatment)
- Heart failure (especially valsartan)
- Diabetic nephropathy (particularly losartan, irbesartan)
- Left ventricular dysfunction post-MI
- Chronic kidney disease with proteinuria
Adverse Effects
- Common: Dizziness, hyperkalemia, fatigue.
- Rare: Angioedema (less than ACEIs), renal dysfunction.
- Contraindicated in pregnancy and bilateral renal artery stenosis.
Comparative Analysis
| Feature | ARBs | ACE Inhibitors |
|---|---|---|
| Mechanism | AT₁ receptor blockade | ACE inhibition |
| Bradykinin effect | No accumulation | Increases bradykinin |
| Cough | Rare | Common |
| Angioedema | Less frequent | More common |
| Hyperkalemia | Possible | Possible |
| Use in Heart Failure | Yes | Yes |
ARBs are often preferred in patients who are intolerant to ACE inhibitors due to cough or angioedema.
Multiple Choice Questions
- ARBs block:
- A. ACE enzyme
- B. AT₁ receptor
- C. AT₂ receptor
- D. Aldosterone
- Answer: B. AT₁ receptor
- Which of the following is least likely with ARBs?
- A. Hyperkalemia
- B. Dry cough
- C. Hypotension
- D. Renal impairment
- Answer: B. Dry cough
- Which ARB is preferred in diabetic nephropathy?
- A. Losartan
- B. Telmisartan
- C. Valsartan
- D. Candesartan
- Answer: A. Losartan
- ARBs do not affect:
- A. Renin secretion
- B. Aldosterone levels
- C. Bradykinin metabolism
- D. Angiotensin II production
- Answer: C. Bradykinin metabolism
- Which ARB has the longest half-life?
- A. Losartan
- B. Irbesartan
- C. Telmisartan
- D. Valsartan
- Answer: C. Telmisartan
- Which drug is a combination of ARB and thiazide diuretic?
- Why are ARBs less likely to cause cough?
- A. They increase nitric oxide
- B. They block aldosterone
- C. They do not inhibit bradykinin breakdown
- D. They increase dopamine levels
- Answer: C. They do not inhibit bradykinin breakdown
- Which of the following is not an ARB?
- A. Candesartan
- B. Irbesartan
- C. Enalapril
- D. Olmesartan
- Answer: C. Enalapril
- What is the mechanism by which ARBs lower blood pressure?
- A. Vasodilation and sodium retention
- B. Vasodilation and reduced aldosterone
- C. Bradykinin accumulation
- D. Increased heart rate
- Answer: B. Vasodilation and reduced aldosterone
- Which ARB is most commonly used in stroke prevention?
- A. Telmisartan
- B. Valsartan
- C. Losartan
- D. Candesartan
- Answer: A. Telmisartan
FAQs
Q1. Can ARBs be combined with ACE inhibitors?
No, dual blockade is not recommended due to increased risk of renal failure and hyperkalemia.
Q2. Are ARBs safe in pregnancy?
No, they are contraindicated, particularly in the second and third trimesters.
Q3. Do ARBs reduce proteinuria?
Yes, especially useful in diabetic and non-diabetic CKD.
Q4. Do all ARBs have equal efficacy?
While all block AT₁, pharmacokinetics differ. Telmisartan has the longest duration.
Q5. Can ARBs be used in combination with diuretics?
Yes, ARBs are often combined with thiazide diuretics (e.g., losartan + hydrochlorothiazide) to enhance blood pressure-lowering effects through complementary mechanisms.
Q6. Do ARBs have cardioprotective effects?
Yes. ARBs reduce left ventricular hypertrophy and improve cardiovascular outcomes in patients with heart failure and post-myocardial infarction.
Q7. What is the role of ARBs in stroke prevention?
ARBs reduce the risk of stroke, especially in patients with hypertension and left ventricular hypertrophy. Telmisartan has shown cerebrovascular protective effects.
Q8. Are ARBs effective in African descent populations?
They may be less effective as monotherapy due to lower renin levels but still play a role, especially in combination therapy.
Q9. What is the importance of the AT2 receptor?
ARBs selectively block AT1, leaving AT2 receptors unblocked. AT2 activation may have vasodilatory and anti-inflammatory effects, contributing to a beneficial profile.
References
- Goodman & Gilman’s: The Pharmacological Basis of Therapeutics, 12th Edition
- KD Tripathi: Essentials of Medical Pharmacology, 7th Edition
- Harrison’s Principles of Internal Medicine
- Clinical Practice Guidelines – JNC 8 & ESC 2021

I am pursuing MBA in pharmaceutical management from NIPER Hyderabad with a strong academic record and proven success in national-level pharmacy entrance exams. I secured AIR 61 in NIPER 2024 (MS/M.Pharm) and AIR 27 in NIPER MBA, along with AIR 147 in GPAT 2024 and AIR 907 in GPAT 2023. I also achieved AIR 6 in AIIMS CRE-2025 for Drug Store Keeper and was selected as a Pharmacist (AIR 61) for ESIC. Additionally, I was the Runner-Up in Round 2 of the EY Case Study Competition.
At PharmacyFreak.com, I aim to guide future pharmacists through expert content, exam strategies, and insightful resources based on real experience and academic excellence.
Mail- harsh@pharmacyfreak.com