Table of Contents
Introduction
Escitalopram is a selective serotonin reuptake inhibitor (SSRI) widely prescribed for depressive and anxiety disorders. It is the S-enantiomer of citalopram and represents one of the most selective SSRIs available. Its clinical importance lies in its high efficacy, favorable tolerability, and minimal drug–drug interactions compared with older antidepressants. For medical and pharmacy examinations, escitalopram is a high-yield drug due to its precise molecular target, improved selectivity, and role in first-line psychiatric therapy.
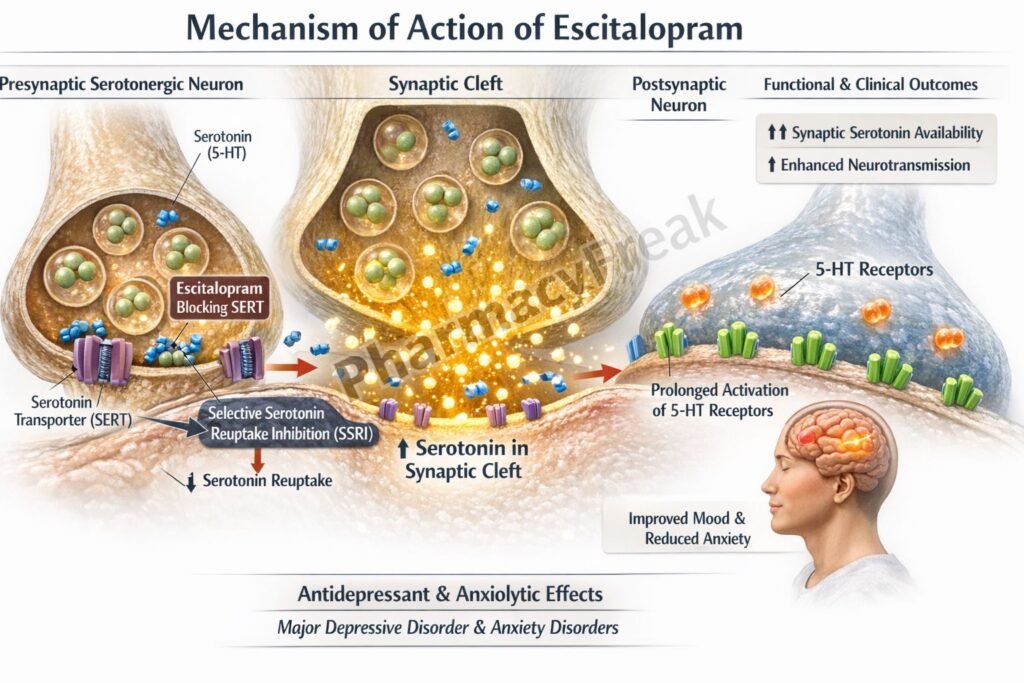
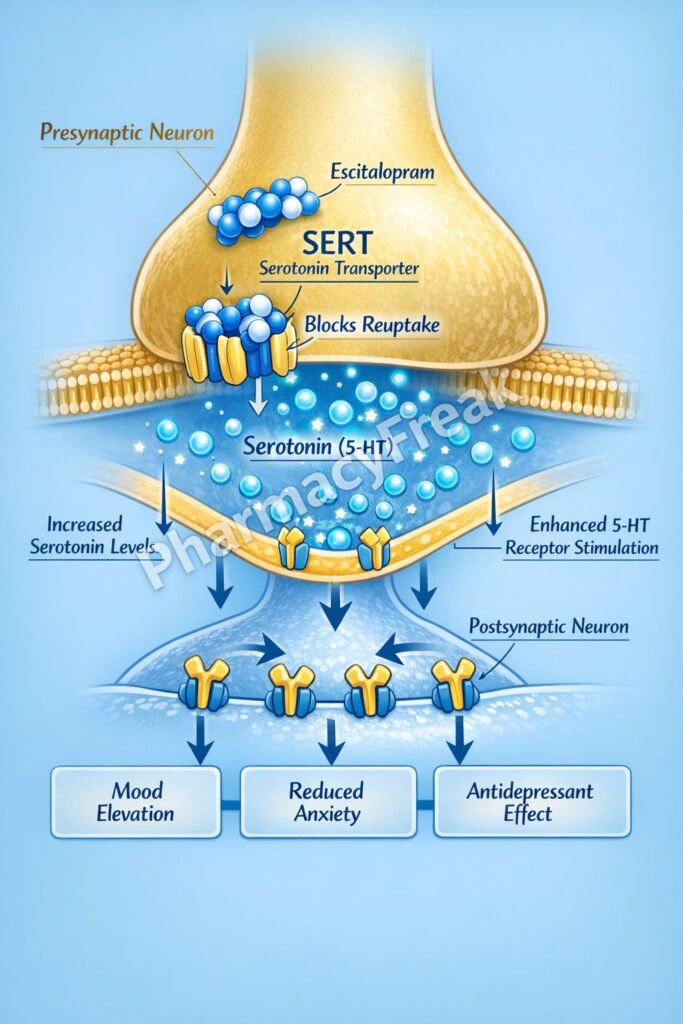
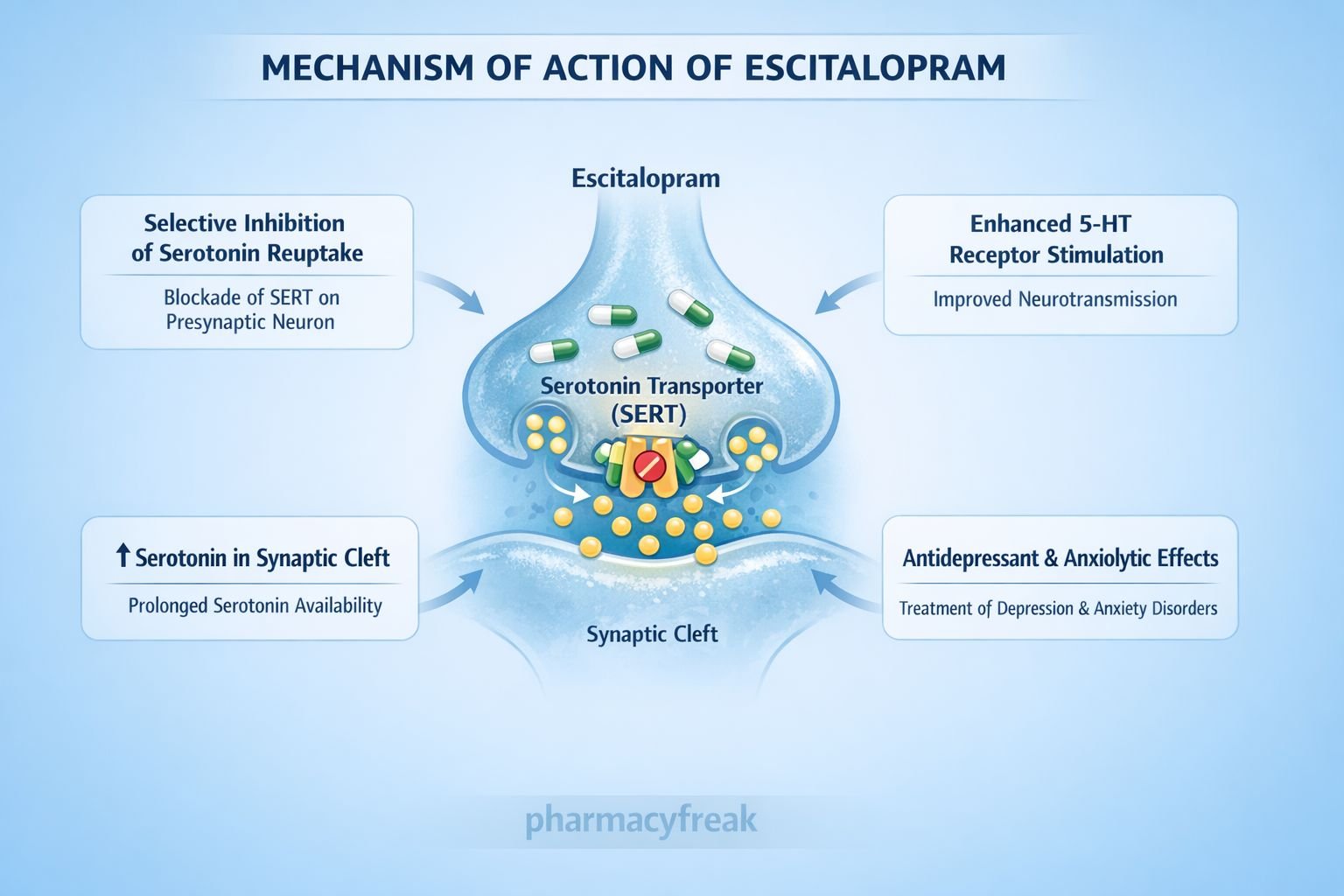
Mechanism of Action (Step-wise)
Escitalopram enhances serotonergic neurotransmission in the central nervous system through selective inhibition of serotonin reuptake.
Step 1: Targeting serotonergic neurons
Escitalopram acts at serotonergic nerve terminals in the brain, particularly within the limbic system and cerebral cortex.
Step 2: Inhibition of serotonin transporter (SERT)
It selectively binds to and inhibits the serotonin transporter (SERT) located on the presynaptic neuronal membrane.
Step 3: Reduced reuptake of serotonin (5-HT)
Inhibition of SERT prevents reabsorption of serotonin into the presynaptic neuron.
Step 4: Increased synaptic serotonin levels
Accumulation of serotonin in the synaptic cleft enhances stimulation of postsynaptic 5-HT receptors.
Step 5: Adaptive receptor and neuronal changes
Chronic use leads to downregulation of presynaptic autoreceptors (5-HT₁A), resulting in sustained antidepressant and anxiolytic effects.
Pharmacokinetics
- Route of administration: Oral
- Bioavailability: ~80%
- Protein binding: Low (~56%)
- Distribution: Extensive CNS penetration
- Metabolism: Hepatic (CYP2C19, CYP3A4, CYP2D6)
- Half-life: ~27–32 hours
- Excretion: Urine and feces as metabolites
- Onset of clinical effect: 1–2 weeks (full effect in 4–6 weeks)
Clinical Uses
- Major depressive disorder (first-line)
- Generalized anxiety disorder
- Panic disorder
- Social anxiety disorder
- Obsessive–compulsive disorder (off-label in some regions)
- Post-traumatic stress disorder (adjunctive use)
Escitalopram is preferred when long-term treatment and tolerability are priorities.
Adverse Effects
Common:
- Nausea
- Headache
- Insomnia or somnolence
- Sexual dysfunction (decreased libido, delayed ejaculation)
Central nervous system:
- Anxiety (initial phase)
- Restlessness
Cardiac:
- QT interval prolongation (dose-related, less than citalopram)
Serious (rare):
- Serotonin syndrome (with other serotonergic drugs)
- Hyponatremia (SIADH, especially in elderly)
Comparative Analysis
Escitalopram vs Fluoxetine vs Sertraline
| Feature | Escitalopram | Fluoxetine | Sertraline |
|---|---|---|---|
| SSRI selectivity | Very high | Moderate | High |
| Half-life | Moderate | Very long | Moderate |
| CYP inhibition | Minimal | Strong (CYP2D6) | Mild |
| Drug interactions | Low | High | Moderate |
| Tolerability | Excellent | Moderate | Good |
Explanation:
Escitalopram’s superior selectivity for SERT accounts for its enhanced tolerability and reduced drug–drug interactions. Fluoxetine’s long half-life increases interaction risk, while sertraline occupies an intermediate position in efficacy and safety.
MCQs
- Escitalopram primarily inhibits:
a) Dopamine transporter
b) Norepinephrine transporter
c) Serotonin transporter
d) Monoamine oxidase
Answer: c) Serotonin transporter
- Therapeutic effects of escitalopram are mainly due to increased:
a) Dopamine
b) GABA
c) Serotonin
d) Acetylcholine
Answer: c) Serotonin
- Escitalopram is the active:
a) R-enantiomer of citalopram
b) S-enantiomer of citalopram
c) Metabolite of fluoxetine
d) Prodrug of sertraline
Answer: b) S-enantiomer of citalopram
- Time required for full antidepressant effect is typically:
a) 24 hours
b) 2–3 days
c) 1 week
d) 4–6 weeks
Answer: d) 4–6 weeks
- Sexual dysfunction with escitalopram is due to:
a) Dopamine blockade
b) Excess serotonin
c) Anticholinergic effect
d) GABA inhibition
Answer: b) Excess serotonin
- Which adverse effect is dose-related with escitalopram?
a) Hepatotoxicity
b) QT prolongation
c) Nephrotoxicity
d) Agranulocytosis
Answer: b) QT prolongation
- Escitalopram has fewer interactions because it:
a) Is renally excreted unchanged
b) Strongly induces CYP enzymes
c) Minimally inhibits CYP enzymes
d) Blocks MAO
Answer: c) Minimally inhibits CYP enzymes
- Risk of serotonin syndrome increases when combined with:
a) NSAIDs
b) Benzodiazepines
c) Triptans
d) Beta blockers
Answer: c) Triptans
- Initial anxiety seen with escitalopram is due to:
a) Dopamine excess
b) Acute serotonergic stimulation
c) Antimuscarinic effect
d) GABA blockade
Answer: b) Acute serotonergic stimulation
- Preferred SSRI for long-term anxiety treatment is often:
a) Fluoxetine
b) Paroxetine
c) Escitalopram
d) Fluvoxamine
Answer: c) Escitalopram
FAQs
1. Why is escitalopram better tolerated than citalopram?
Because it contains only the active S-enantiomer.
2. Does escitalopram cause sedation?
It is generally neutral but may cause mild somnolence or insomnia.
3. Can escitalopram be used in elderly patients?
Yes, with dose adjustment and monitoring for hyponatremia.
4. Why is onset of action delayed?
Due to time required for receptor adaptation and neuronal plasticity.
5. Is escitalopram addictive?
No, it does not produce dependence.
References
- Goodman & Gilman’s The Pharmacological Basis of Therapeutics
https://accesspharmacy.mhmedical.com - Katzung BG. Basic and Clinical Pharmacology
https://accessmedicine.mhmedical.com - Tripathi KD. Essentials of Medical Pharmacology
- Harrison’s Principles of Internal Medicine
https://accessmedicine.mhmedical.com

I am pursuing MBA in pharmaceutical management from NIPER Hyderabad with a strong academic record and proven success in national-level pharmacy entrance exams. I secured AIR 61 in NIPER 2024 (MS/M.Pharm) and AIR 27 in NIPER MBA, along with AIR 147 in GPAT 2024 and AIR 907 in GPAT 2023. I also achieved AIR 6 in AIIMS CRE-2025 for Drug Store Keeper and was selected as a Pharmacist (AIR 61) for ESIC. Additionally, I was the Runner-Up in Round 2 of the EY Case Study Competition.
At PharmacyFreak.com, I aim to guide future pharmacists through expert content, exam strategies, and insightful resources based on real experience and academic excellence.
Mail- harsh@pharmacyfreak.com