Table of Contents
Introduction
Paracetamol (also known as Acetaminophen) is one of the most commonly used drugs for fever and mild-to-moderate pain. Unlike NSAIDs, it has minimal anti-inflammatory action and does not cause gastric irritation.
It is classified as:
- An analgesic and antipyretic
- Belonging to the para-aminophenol derivative class
Despite its widespread use, its exact mechanism of action has long been debated and is often misunderstood—making it a favorite question in exams like GPAT, NEET-PG, NIPER, MBBS, and NCLEX.
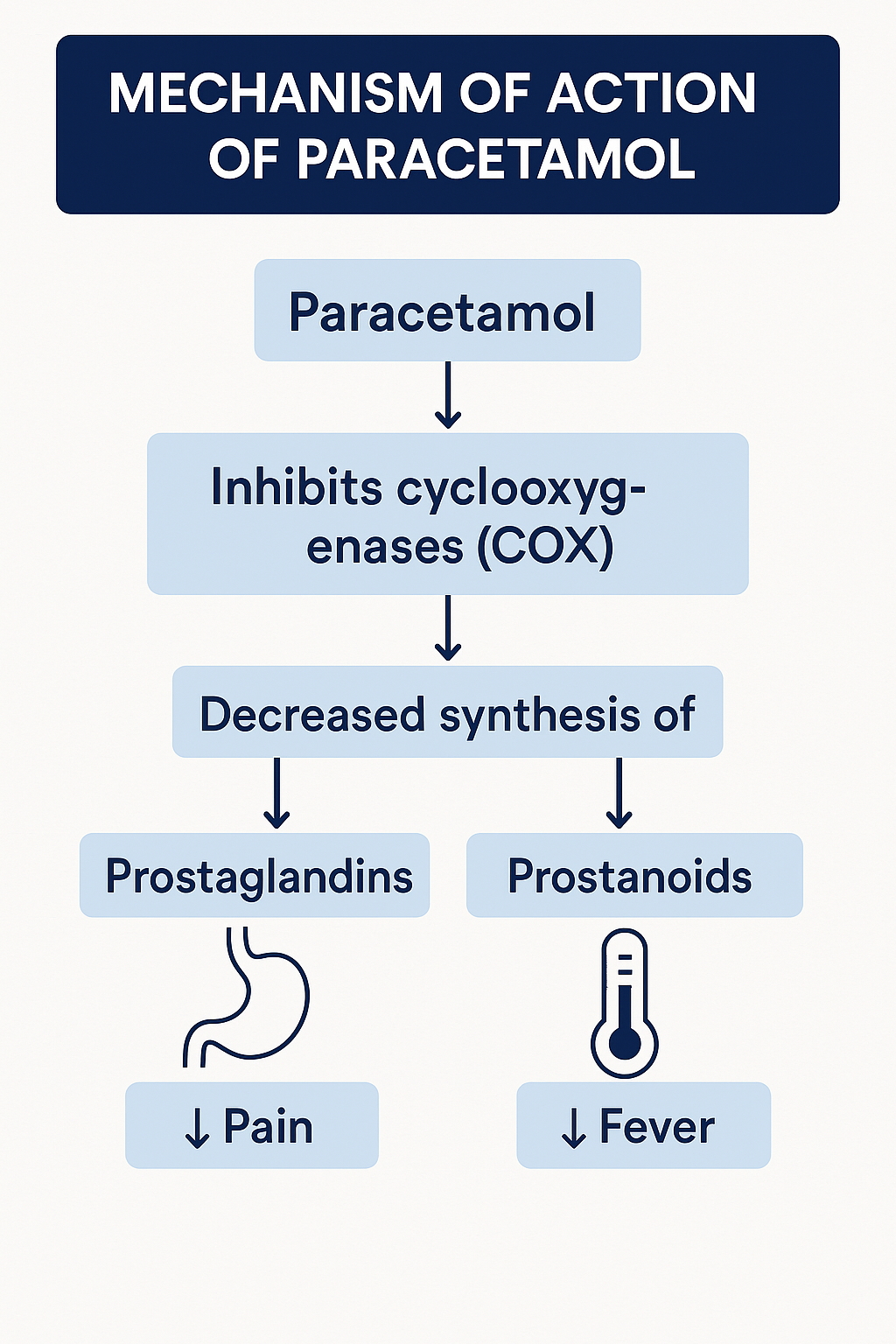
Stepwise Mechanism of Action of Paracetamol
- Central COX Inhibition (COX-3 Hypothesis):
Paracetamol acts predominantly in the central nervous system (CNS). It inhibits cyclooxygenase (COX) enzymes, especially a brain-specific COX variant (possibly COX-3), leading to reduced synthesis of prostaglandins in the hypothalamus. - Antipyretic Effect via Hypothalamus:
By inhibiting prostaglandin E₂ (PGE₂) in the preoptic area of the hypothalamus, it lowers the set-point for body temperature → antipyretic effect. - Analgesic Action (Spinal and Supraspinal Sites):
Decreased central prostaglandin levels also reduce the activation of pain receptors → analgesic effect. - No Peripheral Anti-inflammatory Effect:
In peripheral tissues, high levels of peroxides in inflamed areas limit paracetamol’s COX inhibition, explaining its poor anti-inflammatory action. - TRPV1 & Serotonin Modulation (Additional):
Emerging evidence suggests that paracetamol’s metabolites (like AM404) may also activate TRPV1 receptors and enhance serotoninergic descending pain pathways—contributing to analgesia.

Pharmacokinetic Parameters of Paracetamol
| Parameter | Value |
|---|---|
| Bioavailability | 60–90% (oral) |
| Onset of Action | 30–60 minutes |
| Half-life | 2–3 hours |
| Protein Binding | 20–25% |
| Metabolism | Liver (Phase I & II – glucuronidation, sulfation) |
| Excretion | Renal (as conjugates) |
At high doses, metabolism shifts to CYP2E1 pathway, producing the toxic metabolite NAPQI → hepatotoxicity risk.
Clinical Uses of Paracetamol
- Fever (any age group, preferred antipyretic in children)
- Mild to moderate pain: headache, muscle pain, dental pain
- Osteoarthritis (preferred in patients with GI risk)
- Safe option in gastritis or peptic ulcer disease
- Can be used in pregnancy
Adverse Effects of Paracetamol
- Hepatotoxicity in overdose due to NAPQI accumulation
- Rare: skin reactions (Stevens-Johnson syndrome), anemia
- Usually safe at therapeutic doses
🛡️ Antidote: N-acetylcysteine (NAC) – restores hepatic glutathione and detoxifies NAPQI.
Comparative Analysis: Paracetamol vs Ibuprofen
| Feature | Paracetamol | Ibuprofen |
|---|---|---|
| Anti-inflammatory | Minimal | Strong |
| Antipyretic | Yes | Yes |
| Gastric irritation | Rare | Common (COX-1 inhibition) |
| Platelet effect | None | Mild, reversible inhibition |
| Preferred in children | Yes | Yes (but avoid long-term use) |
| Liver toxicity risk | Yes (overdose) | Minimal |
| Kidney safety | Safer (unless prolonged/high dose) | Nephrotoxic risk in dehydration |
Practice MCQs
Q1. The primary mechanism of paracetamol’s antipyretic effect is:
A. COX-1 inhibition in peripheral tissues
B. Inhibition of PGE₂ synthesis in hypothalamus ✅
C. Activation of opioid receptors
D. Suppression of histamine release
Q2. Which organ is primarily affected in paracetamol toxicity?
A. Kidney
B. Liver ✅
C. Brain
D. Heart
Q3. The antidote for acute paracetamol poisoning is:
A. Atropine
B. Naloxone
C. N-acetylcysteine ✅
D. Activated charcoal
Q4. Why does paracetamol lack anti-inflammatory action?
A. It inhibits prostacyclin only
B. It acts only on peripheral COX
C. It’s a weak inhibitor of COX-2
D. Peroxide-rich environments reduce its efficacy ✅
Q5. Paracetamol is safe in which of the following conditions?
A. Severe liver disease
B. Peptic ulcer disease ✅
C. Chronic alcoholism
D. Uncontrolled diabetes
Q6. The toxic metabolite responsible for liver injury in overdose is:
A. Acetylsalicylate
B. AM404
C. NAPQI ✅
D. Serotonin
Q7. Which phase of metabolism converts paracetamol to safe conjugates?
A. Phase 0
B. Phase I oxidation
C. Phase II glucuronidation & sulfation ✅
D. CYP3A4 hydroxylation
Q8. The TRPV1 receptor involvement in paracetamol MOA is linked to:
A. Fever reduction
B. Analgesic effect ✅
C. Vasodilation
D. Platelet inhibition
Q9. Which statement is FALSE about paracetamol?
A. It can be given to infants
B. It is a good anti-inflammatory agent ✅
C. It acts centrally
D. It is safer for gastric patients
Q10. Which statement is TRUE?
A. Paracetamol causes GI bleeding like aspirin
B. It irreversibly inhibits COX-2
C. It works via prostaglandin suppression in CNS ✅
D. It enhances serotonin breakdown
FAQs
Q1: Can paracetamol be used in pregnancy?
Yes, it is considered safe when used in recommended doses.
Q2: Is paracetamol an NSAID?
No, it lacks significant anti-inflammatory properties and does not affect platelets or gastric mucosa like traditional NSAIDs.
Q3: What happens in paracetamol overdose?
It leads to the accumulation of NAPQI, a hepatotoxic metabolite, causing potential liver failure.
Q4: How soon should N-acetylcysteine be given after overdose?
Best within 8 hours of ingestion for maximum effectiveness.
References
- KD Tripathi – Essentials of Medical Pharmacology, 8th Edition
- Goodman & Gilman – The Pharmacological Basis of Therapeutics
- Review of Pharmacology by Sparsh Gupta

I am pursuing MBA in pharmaceutical management from NIPER Hyderabad with a strong academic record and proven success in national-level pharmacy entrance exams. I secured AIR 61 in NIPER 2024 (MS/M.Pharm) and AIR 27 in NIPER MBA, along with AIR 147 in GPAT 2024 and AIR 907 in GPAT 2023. I also achieved AIR 6 in AIIMS CRE-2025 for Drug Store Keeper and was selected as a Pharmacist (AIR 61) for ESIC. Additionally, I was the Runner-Up in Round 2 of the EY Case Study Competition.
At PharmacyFreak.com, I aim to guide future pharmacists through expert content, exam strategies, and insightful resources based on real experience and academic excellence.
Mail- harsh@pharmacyfreak.com

I FREAKING LOOOVEEEEEE UUUU @PHARMACYFREAK 🩷🩷🩷🥹website fr fr…. idk why I didn’t discovered this website sooner 😭😭 Anyways, after discovering it 1 day before exam, I am still thankful 🫶🏻🫶🏻🫶🏻
Thank You