Table of Contents
Introduction
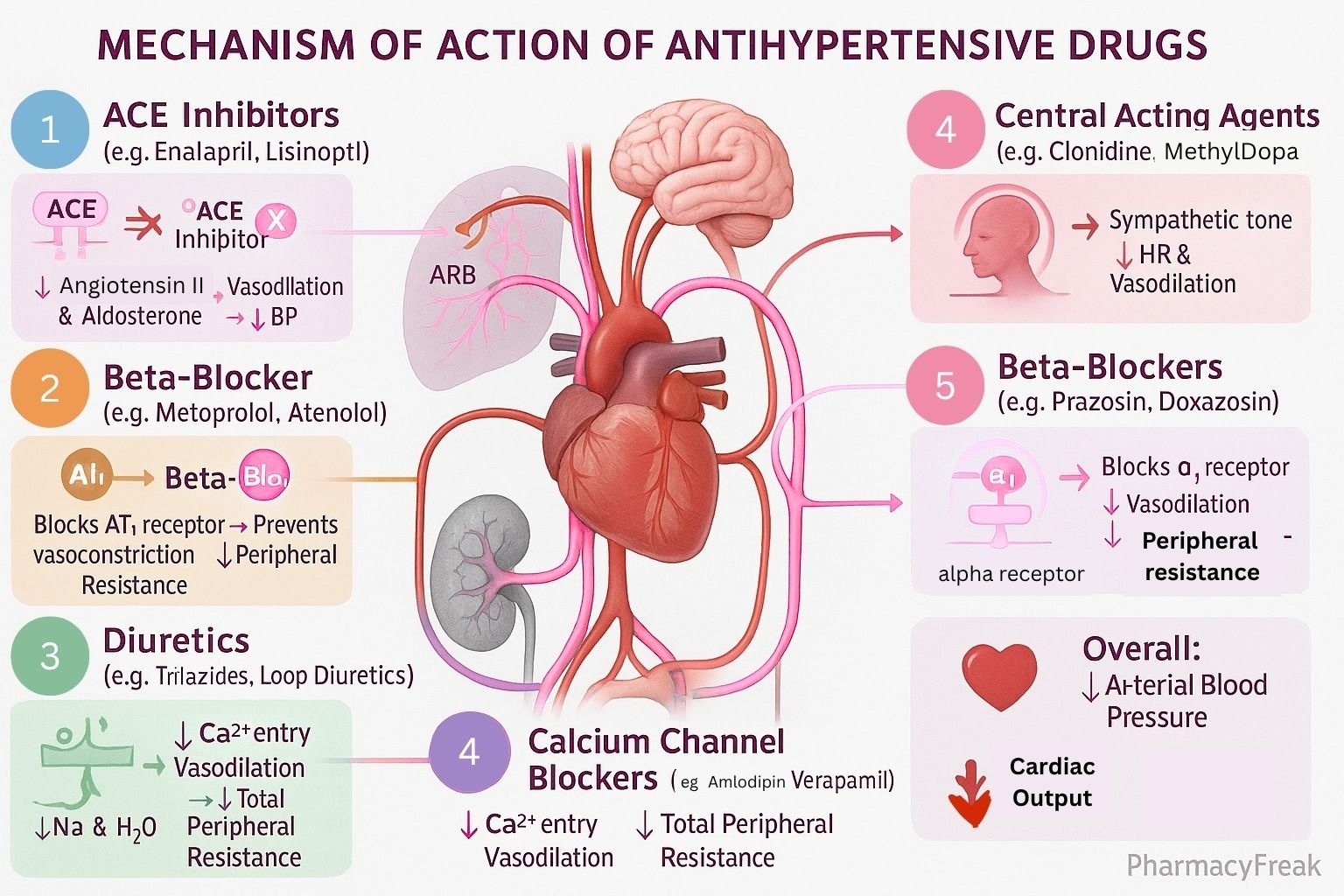
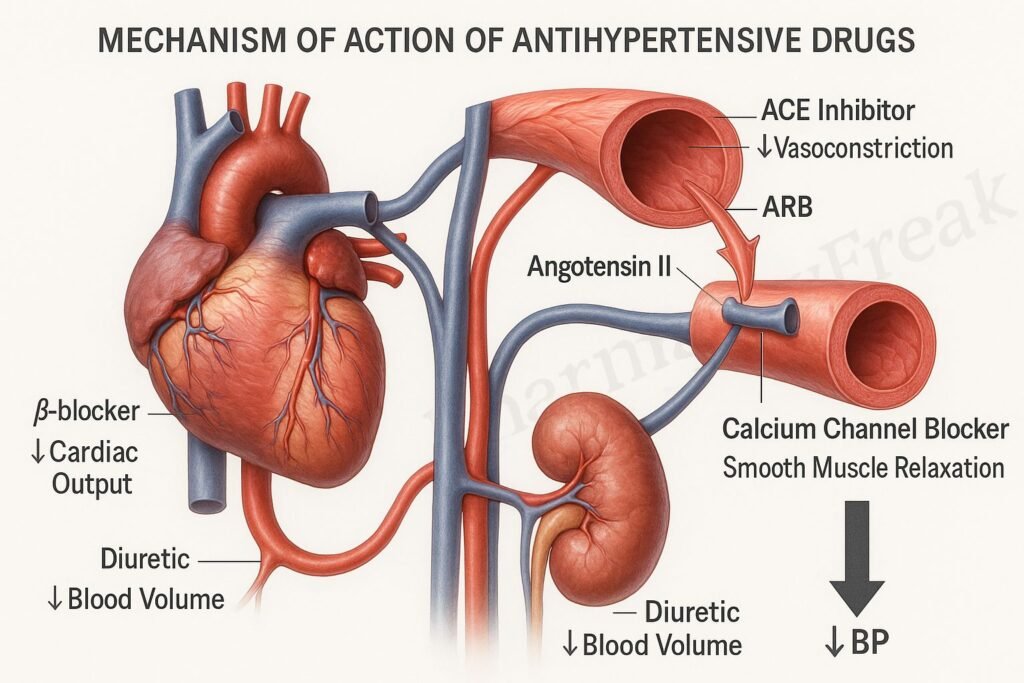
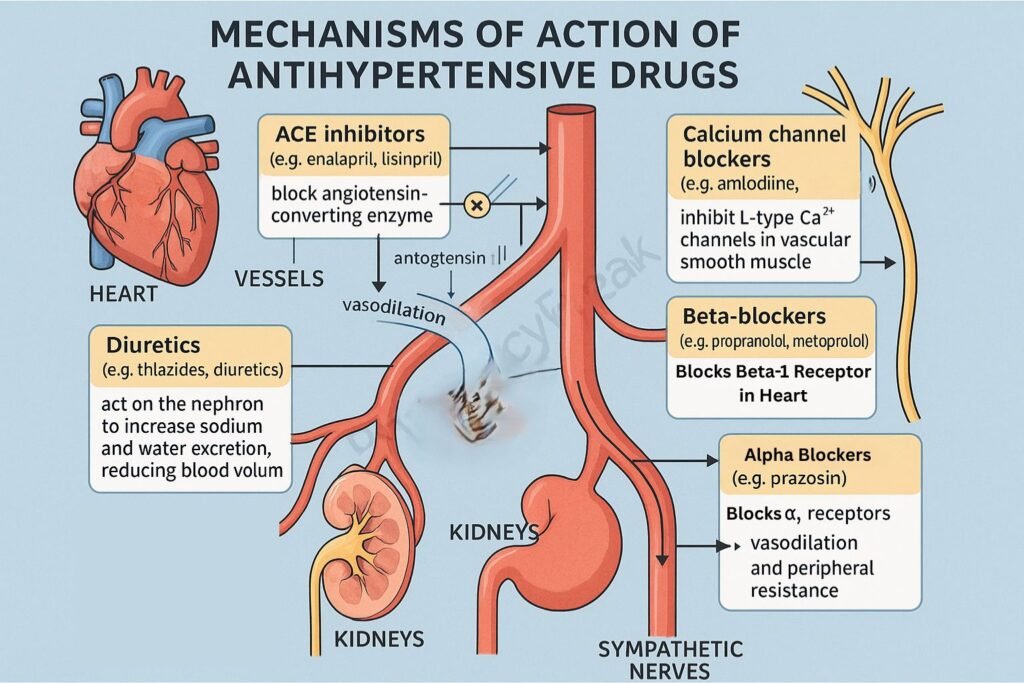
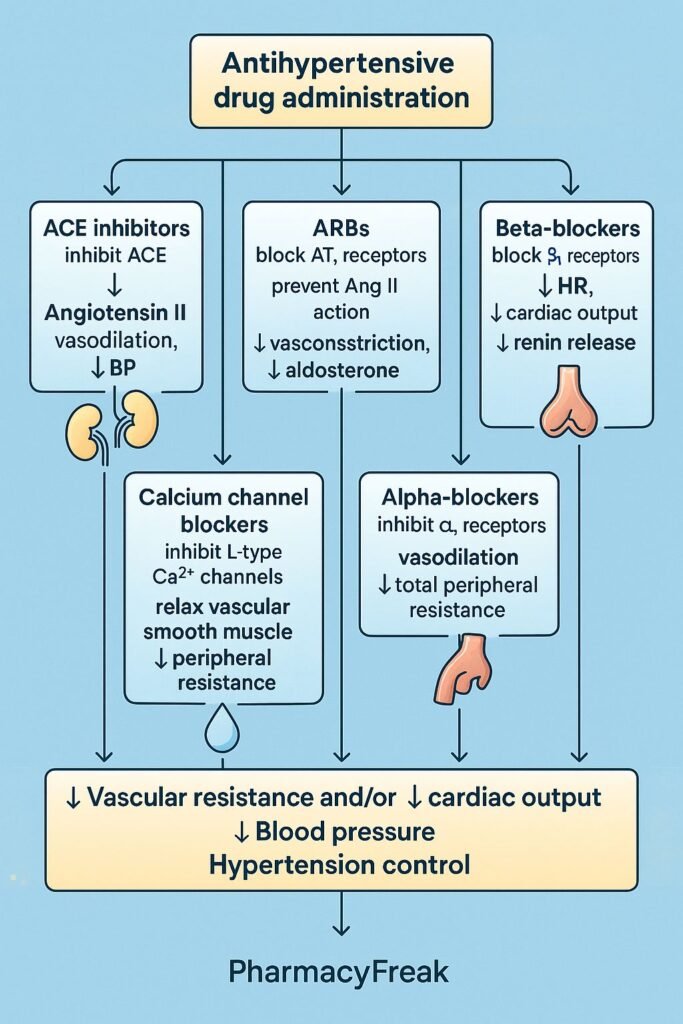
Antihypertensive drugs are pharmacological agents used to lower elevated blood pressure and prevent complications such as stroke, heart failure, myocardial infarction, and renal disease. Mechanism of Action of Antihypertensive Drugs involves reducing vascular resistance, cardiac output, or blood volume, targeting multiple physiological systems including the sympathetic nervous system, renin–angiotensin–aldosterone system (RAAS), and renal function.
These drugs are classified into several groups based on their site and mechanism of action: diuretics, sympatholytics, vasodilators, and agents acting on the RAAS.
Mechanism of Action (Step-wise)
Antihypertensive agents act at different levels of cardiovascular regulation, ultimately reducing arterial pressure.
1. Diuretics
- Mechanism:
- Promote renal excretion of sodium and water, leading to decreased blood volume and cardiac output.
- Chronic use also causes vasodilation, reducing peripheral resistance.
- Examples: Hydrochlorothiazide, Furosemide, Spironolactone, Chlorthalidone.
- Effect: Reduction in plasma volume → ↓ preload → ↓ blood pressure.
2. Beta-Adrenergic Blockers (β-Blockers)
- Mechanism:
- Block β₁-adrenergic receptors in the heart → ↓ heart rate and contractility → ↓ cardiac output.
- Inhibit renin release from the kidney, reducing angiotensin II formation.
- Examples: Propranolol, Atenolol, Metoprolol, Bisoprolol, Nebivolol.
- Effect: Reduced cardiac workload and inhibition of RAAS activity.
3. Calcium Channel Blockers (CCBs)
- Mechanism:
- Inhibit L-type calcium channels in vascular smooth muscle → ↓ intracellular Ca²⁺ → vasodilation.
- Some also act on the heart to reduce contractility and heart rate.
- Examples:
- Dihydropyridines: Amlodipine, Nifedipine.
- Non-dihydropyridines: Verapamil, Diltiazem.
- Effect: Decreased total peripheral resistance (TPR) and blood pressure.
4. Angiotensin-Converting Enzyme (ACE) Inhibitors
- Mechanism:
- Block conversion of angiotensin I → angiotensin II, a potent vasoconstrictor.
- Decrease aldosterone secretion, leading to sodium and water loss.
- Increase bradykinin levels, enhancing vasodilation.
- Examples: Enalapril, Lisinopril, Captopril, Ramipril.
- Effect: Vasodilation, reduced fluid retention, and improved cardiac function.
5. Angiotensin II Receptor Blockers (ARBs)
- Mechanism:
- Block angiotensin II binding to AT₁ receptors, preventing vasoconstriction and aldosterone release.
- Similar end effects to ACE inhibitors but without bradykinin-mediated cough.
- Examples: Losartan, Valsartan, Telmisartan, Olmesartan.
- Effect: Vasodilation and decreased blood volume.
6. Alpha-Adrenergic Blockers (α₁-Blockers)
- Mechanism:
- Block α₁-adrenergic receptors on vascular smooth muscle → inhibition of vasoconstriction → decreased systemic vascular resistance.
- Examples: Prazosin, Doxazosin, Terazosin.
- Effect: Vasodilation and reduction in arterial pressure.
7. Central Sympatholytics
- Mechanism:
- Stimulate α₂-adrenergic receptors in the medulla → inhibit sympathetic outflow → reduce heart rate, contractility, and peripheral resistance.
- Examples: Clonidine, Methyldopa, Guanfacine.
- Effect: Decreased sympathetic tone and lowered blood pressure.
8. Direct Vasodilators
- Mechanism:
- Relax vascular smooth muscle directly by increasing nitric oxide (NO) or opening K⁺ channels, leading to hyperpolarization and relaxation.
- Examples: Hydralazine, Minoxidil, Sodium Nitroprusside.
- Effect: Decreased afterload and peripheral vascular resistance.
9. Renin Inhibitors
- Mechanism:
- Directly inhibit renin enzyme activity, blocking conversion of angiotensinogen to angiotensin I → reduced RAAS activation.
- Example: Aliskiren.
- Effect: Lowered angiotensin II and aldosterone levels → vasodilation and natriuresis.
10. Aldosterone Antagonists
- Mechanism:
- Block aldosterone receptors in the distal nephron → prevent sodium and water reabsorption → promote diuresis.
- Examples: Spironolactone, Eplerenone.
- Effect: Decreased intravascular volume and reduced cardiac remodeling.
Summary Table: Major Antihypertensive Drug Classes
| Class | Mechanism | Physiological Effect | Example Drugs |
|---|---|---|---|
| Diuretics | ↑ Na⁺ and water excretion | ↓ Blood volume | Furosemide, HCTZ |
| β-Blockers | Block β₁ receptors | ↓ HR, ↓ renin | Atenolol, Metoprolol |
| CCBs | Block Ca²⁺ influx | Vasodilation | Amlodipine, Verapamil |
| ACE Inhibitors | Inhibit Ang I → Ang II | ↓ Vasoconstriction | Enalapril, Lisinopril |
| ARBs | Block AT₁ receptors | ↓ Aldosterone | Losartan, Valsartan |
| α₁-Blockers | Block α₁ receptors | Vasodilation | Prazosin, Doxazosin |
| Central Agents | Stimulate α₂ receptors | ↓ Sympathetic tone | Clonidine, Methyldopa |
| Vasodilators | Relax smooth muscle | ↓ Peripheral resistance | Hydralazine, Minoxidil |
| Renin Inhibitors | Inhibit renin enzyme | ↓ RAAS activity | Aliskiren |
| Aldosterone Antagonists | Block aldosterone receptors | ↓ Fluid retention | Spironolactone, Eplerenone |
MCQs
1. ACE inhibitors lower BP by:
a) Blocking α-receptors
b) Inhibiting Angiotensin II formation
c) Stimulating renin
d) Increasing sodium retention
Answer: b) Inhibiting Angiotensin II formation
2. ARBs act by blocking:
a) β₁ receptors
b) Angiotensin II at AT₁ receptors
c) Calcium channels
d) α₁ receptors
Answer: b) Angiotensin II at AT₁ receptors
3. Beta-blockers decrease BP by:
a) Increasing cardiac output
b) Reducing renin release and heart rate
c) Increasing vasoconstriction
d) Blocking α₂ receptors
Answer: b) Reducing renin release and heart rate
4. Which antihypertensive increases NO availability?
a) Hydralazine
b) Clonidine
c) Losartan
d) Metoprolol
Answer: a) Hydralazine
5. The drug that acts directly on renin is:
a) Aliskiren
b) Lisinopril
c) Losartan
d) Spironolactone
Answer: a) Aliskiren
6. Calcium channel blockers cause:
a) Vasoconstriction
b) Vasodilation
c) Increased heart rate
d) Increased renin release
Answer: b) Vasodilation
7. Methyldopa acts by:
a) Central α₂ receptor stimulation
b) Peripheral α₁ receptor blockade
c) Calcium channel inhibition
d) Direct NO release
Answer: a) Central α₂ receptor stimulation
8. Spironolactone lowers BP by:
a) Blocking aldosterone receptors
b) Blocking β₁ receptors
c) Reducing sympathetic tone
d) Inhibiting Ang II formation
Answer: a) Blocking aldosterone receptors
9. The main adverse effect of ACE inhibitors is:
a) Bradycardia
b) Cough and hyperkalemia
c) Hypokalemia
d) Gynecomastia
Answer: b) Cough and hyperkalemia
10. Minoxidil primarily acts on:
a) Calcium channels
b) Potassium channels in vascular smooth muscle
c) Renin enzyme
d) α₁ receptors
Answer: b) Potassium channels in vascular smooth muscle
FAQs
Q1. What are antihypertensive drugs?
They are medications used to lower high blood pressure and prevent end-organ damage.
Q2. Which class is preferred in diabetic hypertension?
ACE inhibitors or ARBs for renal protection.
Q3. Why do ACE inhibitors cause cough?
Due to accumulation of bradykinin in the lungs.
Q4. Which antihypertensive should be avoided in pregnancy?
ACE inhibitors, ARBs, and Aliskiren (fetotoxic).
Q5. What drugs are first-line for essential hypertension?
Thiazide diuretics, ACE inhibitors, ARBs, or CCBs.
Q6. Which drug causes reflex tachycardia?
Hydralazine and Minoxidil (due to baroreceptor activation).
References
- Goodman & Gilman’s The Pharmacological Basis of Therapeutics
- Katzung BG. Basic and Clinical Pharmacology
- Tripathi KD. Essentials of Medical Pharmacology
- Harrison’s Principles of Internal Medicine
Related Internal Links

I am pursuing MBA in pharmaceutical management from NIPER Hyderabad with a strong academic record and proven success in national-level pharmacy entrance exams. I secured AIR 61 in NIPER 2024 (MS/M.Pharm) and AIR 27 in NIPER MBA, along with AIR 147 in GPAT 2024 and AIR 907 in GPAT 2023. I also achieved AIR 6 in AIIMS CRE-2025 for Drug Store Keeper and was selected as a Pharmacist (AIR 61) for ESIC. Additionally, I was the Runner-Up in Round 2 of the EY Case Study Competition.
At PharmacyFreak.com, I aim to guide future pharmacists through expert content, exam strategies, and insightful resources based on real experience and academic excellence.
Mail- harsh@pharmacyfreak.com