Table of Contents
Introduction
Rivaroxaban is an oral anticoagulant belonging to the class of direct Factor Xa inhibitors. It is commonly prescribed for the prevention and treatment of thromboembolic disorders such as deep vein thrombosis (DVT), pulmonary embolism (PE), and stroke prevention in non-valvular atrial fibrillation. Unlike warfarin, rivaroxaban has a predictable pharmacokinetic profile and does not require routine coagulation monitoring.
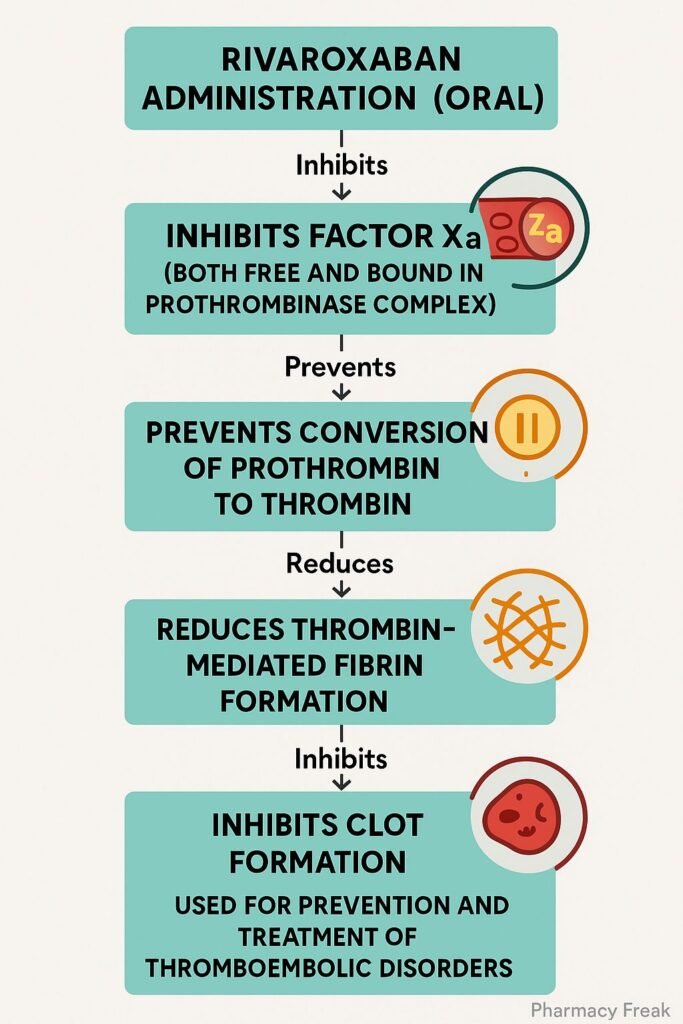
Mechanism of Action (Step-wise)
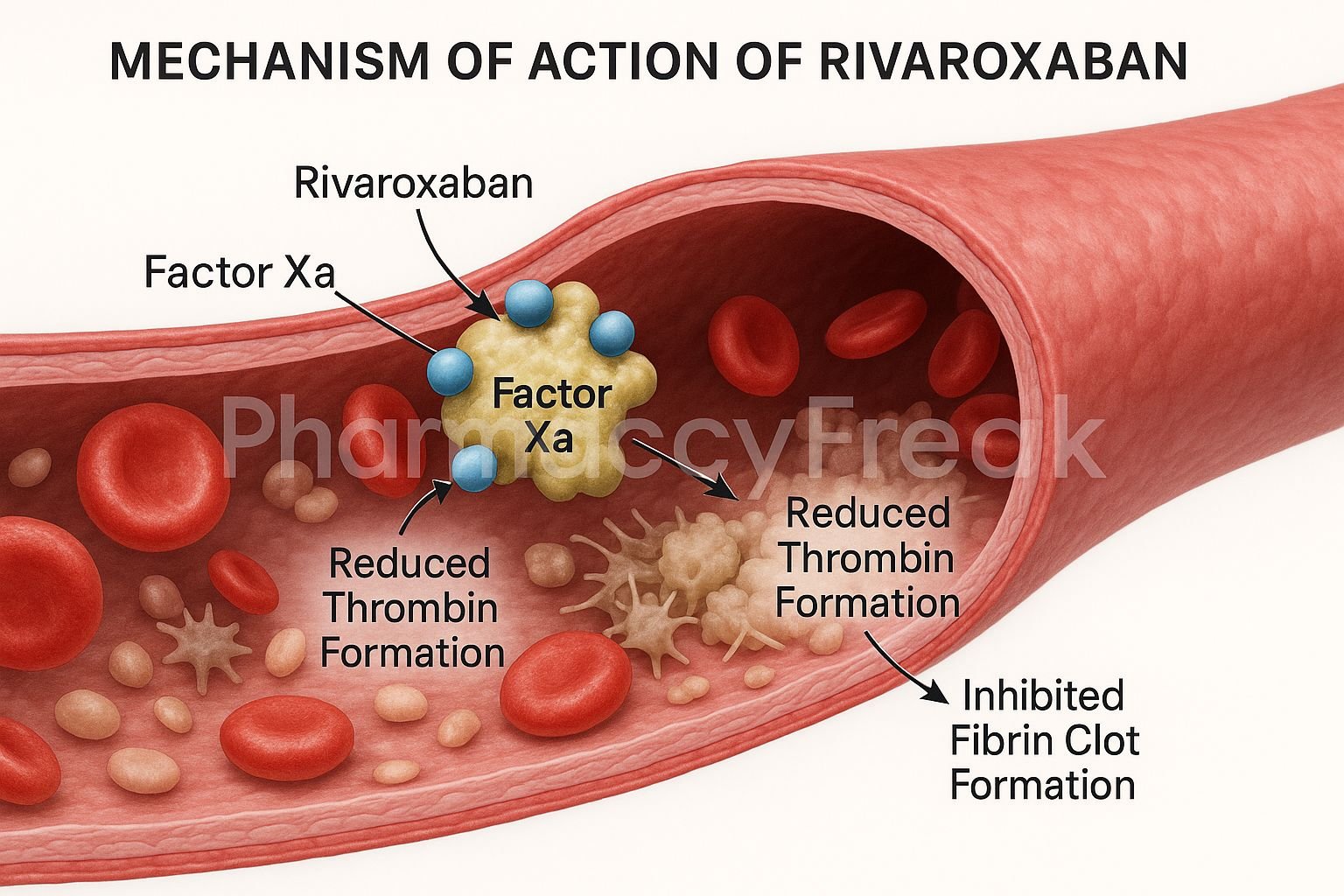
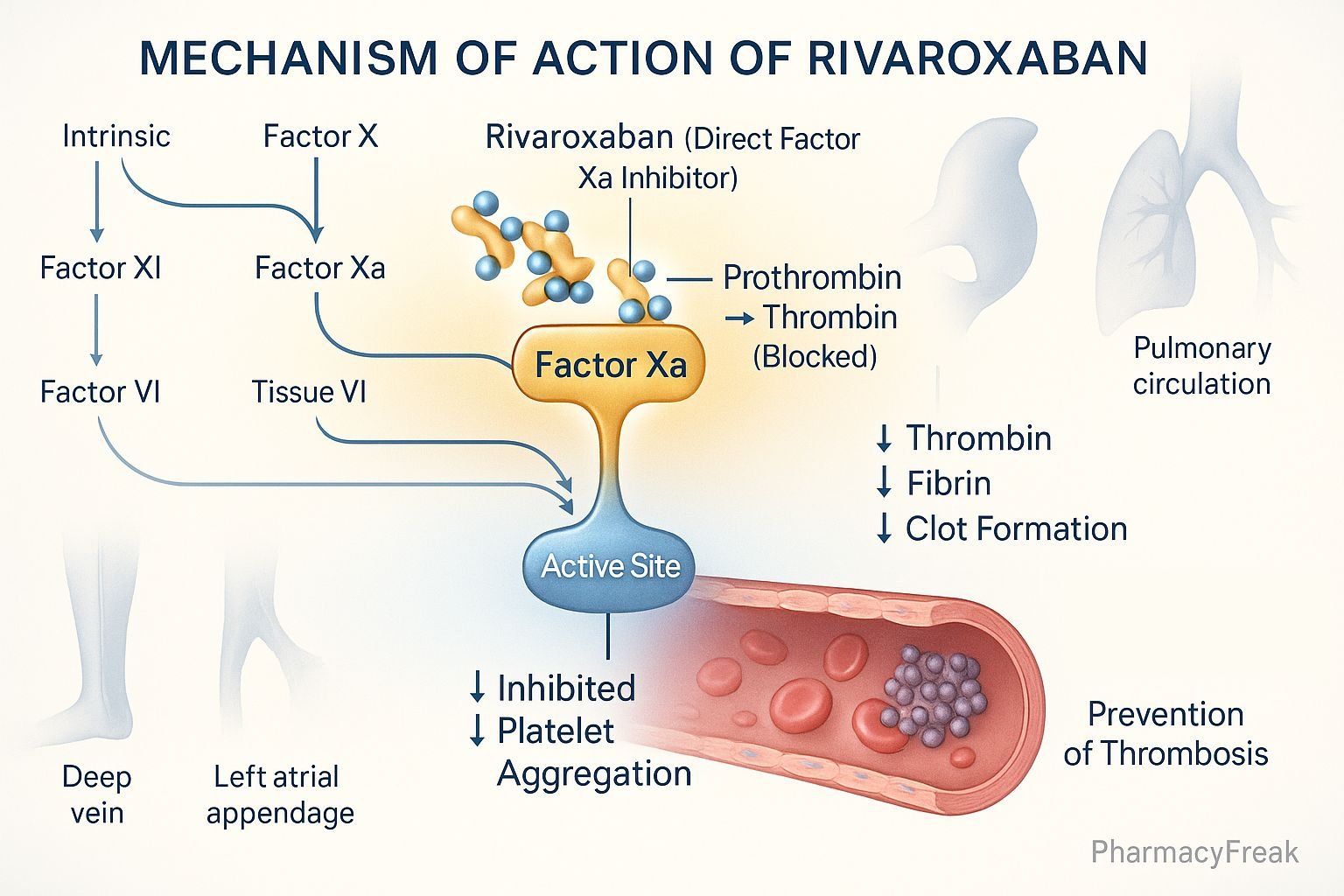
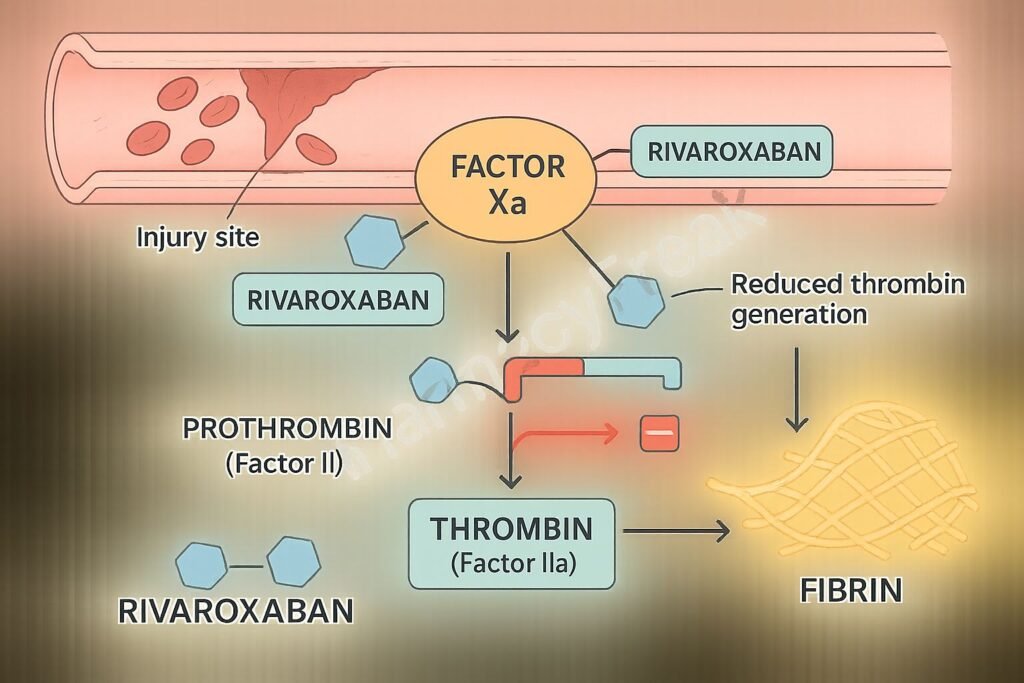
1. Direct Inhibition of Factor Xa
Rivaroxaban selectively and directly binds to the active site of Factor Xa, inhibiting both free Factor Xa and Factor Xa within the prothrombinase complex.
2. Prevention of Prothrombin Conversion
By inhibiting Factor Xa, rivaroxaban prevents the conversion of prothrombin to thrombin, a key enzyme required for fibrin clot formation.
3. Reduced Thrombin Generation
With lower thrombin levels, the amplification of the coagulation cascade is interrupted, reducing clot formation.
4. Antithrombotic Effect Without Antithrombin III
Rivaroxaban exerts its anticoagulant effect independently of antithrombin III, differing from heparins which require this cofactor.
5. No Direct Effect on Platelets
Rivaroxaban does not affect platelet aggregation directly but reduces thrombin-mediated platelet activation.
Pharmacokinetics
- Route of Administration: Oral
- Bioavailability: Approximately 80–100% with food (10 mg dose)
- Peak Plasma Time: 2–4 hours post-dose
- Half-Life: 5–9 hours in healthy individuals; 11–13 hours in elderly
- Metabolism: Hepatic, primarily via CYP3A4/5 and CYP2J2
- Excretion: Renal (66%) and fecal (33%) pathways
Clinical Uses
- Stroke prevention in non-valvular atrial fibrillation
- Treatment and secondary prevention of DVT and PE
- Primary prevention of venous thromboembolism (VTE) post-hip or knee replacement
- Prevention of cardiovascular events in patients with chronic coronary artery disease (CAD) or peripheral artery disease (PAD)
Adverse Effects
- Bleeding: Major or minor hemorrhagic events including gastrointestinal and intracranial bleeding
- Anemia: Due to occult blood loss
- Elevated liver enzymes: Mild and transient in some cases
- Contraindications: Active pathological bleeding, severe hepatic impairment with coagulopathy, pregnancy
Comparative Analysis
| Parameter | Rivaroxaban | Warfarin |
|---|---|---|
| Mechanism | Direct Factor Xa inhibitor | Vitamin K antagonist |
| Monitoring Required | No | Yes (INR) |
| Onset of Action | Rapid (2–4 hours) | Delayed (36–72 hours) |
| Food Interactions | Minimal | Significant |
| Half-Life | 5–13 hours | 36–42 hours |
| Antidote Available | Yes (Andexanet alfa) | Yes (Vitamin K) |
Multiple Choice Questions (MCQs)
1. Rivaroxaban primarily inhibits which coagulation factor?
a) Factor IIa
b) Factor IXa
c) Factor Xa
d) Factor XIIIa
Answer: c) Factor Xa
2. What is the role of rivaroxaban in the coagulation cascade?
a) Enhances thrombin production
b) Inhibits thrombin degradation
c) Inhibits conversion of fibrinogen to fibrin
d) Inhibits prothrombin conversion to thrombin
Answer: d) Inhibits prothrombin conversion to thrombin
3. Which pathway does rivaroxaban affect most?
a) Extrinsic
b) Intrinsic
c) Common pathway
d) Platelet aggregation pathway
Answer: c) Common pathway
4. Does rivaroxaban require antithrombin III to function?
a) Yes
b) No
Answer: b) No
5. Which of the following is a contraindication for rivaroxaban?
a) Controlled hypertension
b) Diabetes mellitus
c) Active bleeding
d) Iron deficiency anemia
Answer: c) Active bleeding
FAQs
Q1. How does rivaroxaban differ from warfarin?
Rivaroxaban directly inhibits Factor Xa without affecting vitamin K-dependent clotting factors, and it does not require routine INR monitoring.
Q2. Can rivaroxaban be reversed?
Yes, with Andexanet alfa, a specific reversal agent for Factor Xa inhibitors.
Q3. Is food necessary for rivaroxaban absorption?
Food increases absorption, especially for doses higher than 10 mg.
Q4. What is the main risk associated with rivaroxaban?
Bleeding, particularly in patients with renal impairment or concurrent use of other anticoagulants.
Q5. Is rivaroxaban safe in pregnancy?
It is contraindicated due to potential fetal risk.
References
- Goodman & Gilman’s The Pharmacological Basis of Therapeutics, 12th Edition
- KD Tripathi, Essentials of Medical Pharmacology, 7th Edition
- FDA Drug Label for Rivaroxaban
- Clinical guidelines on anticoagulant therapy
- Comparative anticoagulation studies
Related Internal Links

I am pursuing MBA in pharmaceutical management from NIPER Hyderabad with a strong academic record and proven success in national-level pharmacy entrance exams. I secured AIR 61 in NIPER 2024 (MS/M.Pharm) and AIR 27 in NIPER MBA, along with AIR 147 in GPAT 2024 and AIR 907 in GPAT 2023. I also achieved AIR 6 in AIIMS CRE-2025 for Drug Store Keeper and was selected as a Pharmacist (AIR 61) for ESIC. Additionally, I was the Runner-Up in Round 2 of the EY Case Study Competition.
At PharmacyFreak.com, I aim to guide future pharmacists through expert content, exam strategies, and insightful resources based on real experience and academic excellence.
Mail- harsh@pharmacyfreak.com