Table of Contents
Introduction
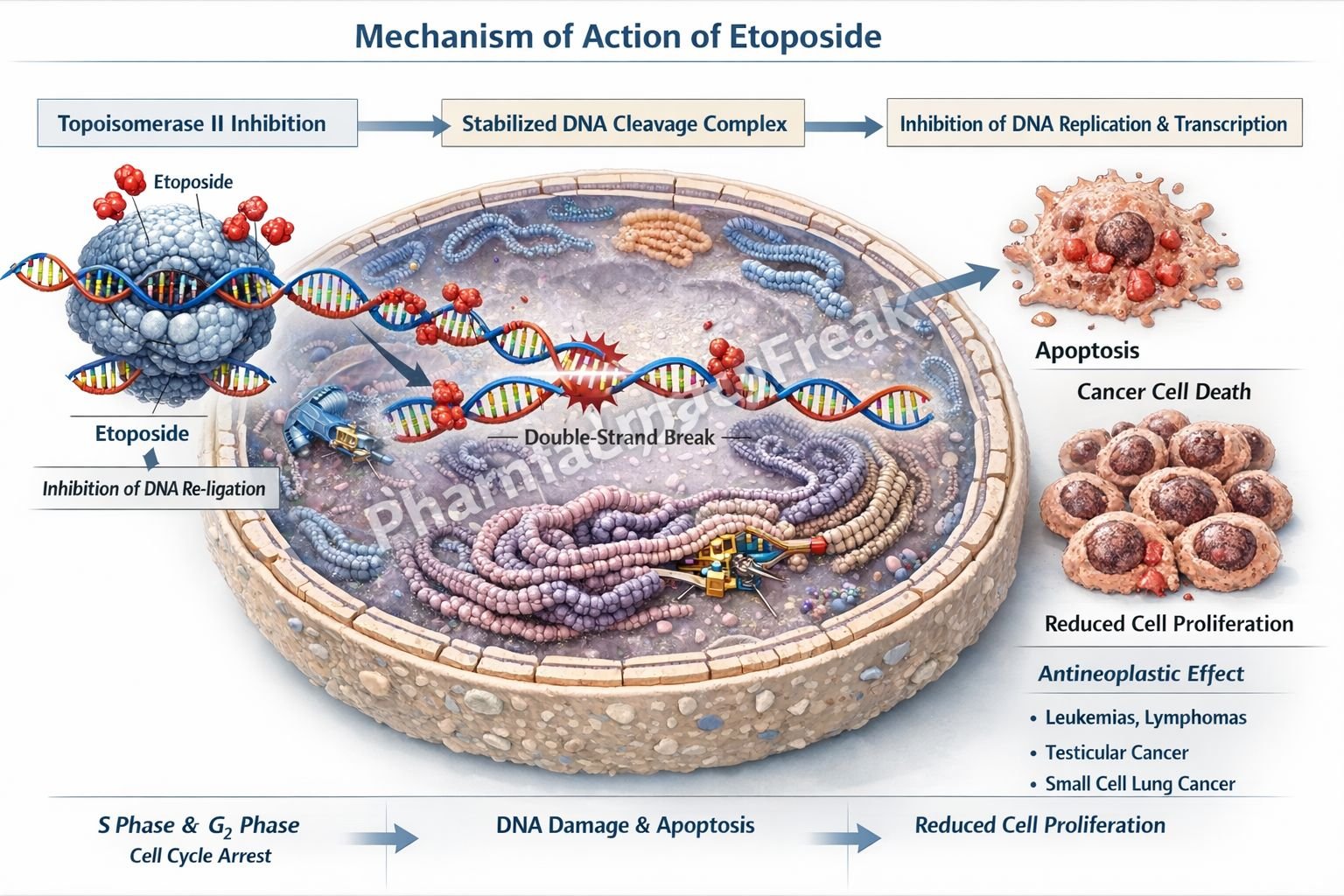
Etoposide is a semisynthetic podophyllotoxin derivative widely used as an antineoplastic agent in the treatment of various solid tumors and hematological malignancies. It is a cell cycle–specific drug, acting primarily during the S and G₂ phases. Etoposide is high-yield for pharmacology and oncology examinations due to its unique enzyme target, characteristic DNA damage mechanism, and dose-limiting myelosuppression.
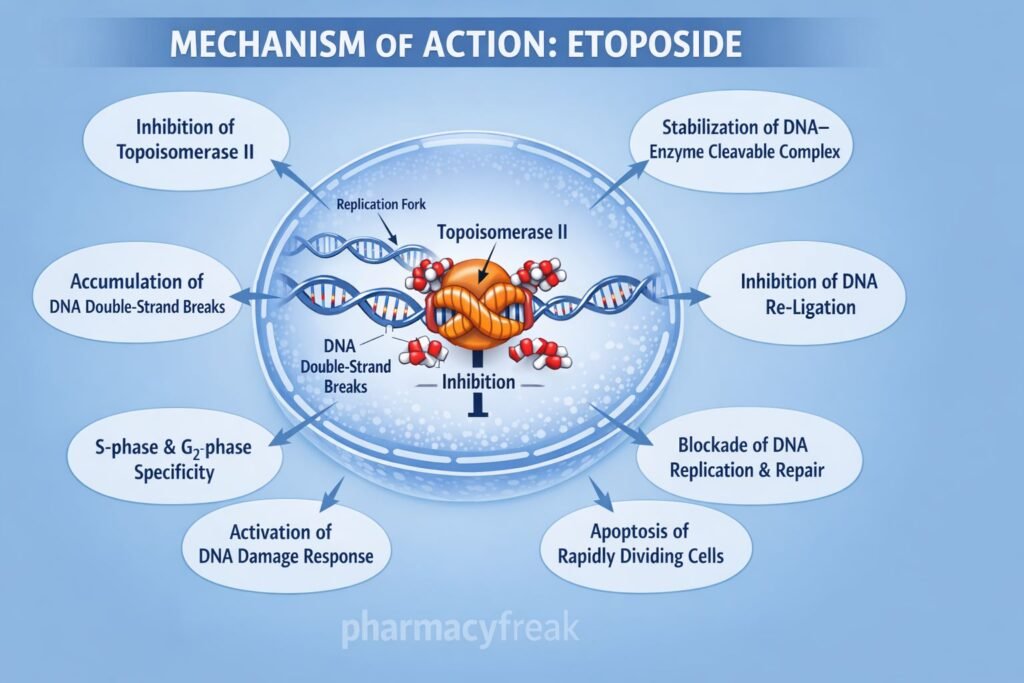
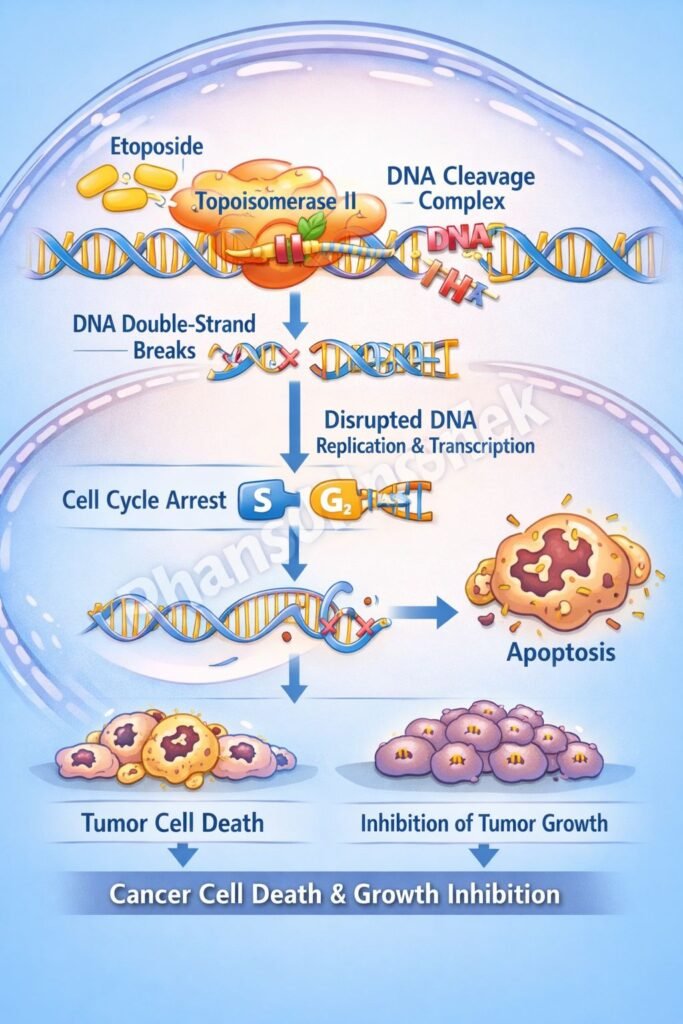
Mechanism of Action (Step-wise)
Etoposide induces cytotoxicity by interfering with DNA replication and repair.
Step 1: Entry into proliferating cells
Etoposide preferentially affects rapidly dividing cells undergoing DNA synthesis.
Step 2: Targeting topoisomerase II
It binds to and inhibits topoisomerase II, an enzyme responsible for relieving torsional strain in DNA by creating transient double-strand breaks.
Step 3: Stabilization of DNA–enzyme complex
Etoposide stabilizes the cleavable complex formed between topoisomerase II and DNA.
Step 4: Prevention of DNA re-ligation
The drug prevents re-ligation of double-strand DNA breaks created by topoisomerase II.
Step 5: Accumulation of DNA damage
Persistent DNA strand breaks lead to inhibition of DNA replication and transcription.
Step 6: Cell cycle arrest and apoptosis
DNA damage triggers cell cycle arrest in the S and G₂ phases, followed by apoptosis.
Exam pearl:
Etoposide causes double-strand DNA breaks, unlike topoisomerase I inhibitors which cause single-strand breaks.
Pharmacokinetics
- Route of administration: Oral, IV
- Oral bioavailability: ~50% (variable)
- Protein binding: ~95%
- Distribution: Widely distributed; limited CNS penetration
- Metabolism: Hepatic (partly via CYP3A4)
- Half-life: 6–12 hours
- Excretion: Renal and biliary
- Dose adjustment: Required in renal impairment
Clinical Uses
- Testicular cancer (part of BEP regimen)
- Small cell lung cancer
- Lymphomas (Hodgkin and non-Hodgkin)
- Acute myeloid leukemia (selected regimens)
- Ovarian cancer
- Ewing sarcoma and other solid tumors
Etoposide is commonly used in combination chemotherapy to enhance efficacy and reduce resistance.
Adverse Effects
Hematological (dose-limiting):
- Myelosuppression (leukopenia > thrombocytopenia)
Gastrointestinal:
- Nausea
- Vomiting
- Mucositis
Dermatological:
- Alopecia
Cardiovascular:
- Hypotension (rapid IV infusion)
Long-term risk:
- Secondary acute leukemia (therapy-related AML)
Comparative Analysis
Etoposide vs Doxorubicin vs Irinotecan
| Feature | Etoposide | Doxorubicin | Irinotecan |
|---|---|---|---|
| Primary target | Topoisomerase II | Topoisomerase II + free radicals | Topoisomerase I |
| DNA damage | Double-strand breaks | Double-strand breaks | Single-strand breaks |
| Cell cycle specificity | S, G₂ phase | Cell cycle–nonspecific | S phase |
| Major toxicity | Myelosuppression | Cardiotoxicity | Diarrhea |
| Secondary leukemia risk | Yes | Yes | No |
Explanation:
Etoposide selectively inhibits topoisomerase II, causing irreversible DNA double-strand breaks. Irinotecan targets topoisomerase I, while doxorubicin additionally generates free radicals, explaining differences in toxicity profiles.
MCQs
- Etoposide primarily inhibits which enzyme?
a) DNA polymerase
b) Topoisomerase I
c) Topoisomerase II
d) RNA polymerase
Answer: c) Topoisomerase II
- DNA damage caused by etoposide involves:
a) Single-strand breaks
b) Double-strand breaks
c) DNA cross-linking
d) Base alkylation
Answer: b) Double-strand breaks
- Etoposide is most active in which cell cycle phases?
a) G₁ phase
b) S and G₂ phases
c) M phase
d) G₀ phase
Answer: b) S and G₂ phases
- Dose-limiting toxicity of etoposide is:
a) Nephrotoxicity
b) Neurotoxicity
c) Myelosuppression
d) Cardiotoxicity
Answer: c) Myelosuppression
- Etoposide is a derivative of:
a) Vinca alkaloids
b) Taxanes
c) Podophyllotoxin
d) Nitrosoureas
Answer: c) Podophyllotoxin
- Which malignancy commonly uses etoposide?
a) Breast cancer
b) Small cell lung cancer
c) Colon cancer
d) Thyroid cancer
Answer: b) Small cell lung cancer
- Risk of secondary leukemia with etoposide is due to:
a) Alkylation of DNA
b) DNA cross-linking
c) Chromosomal translocations
d) Folate depletion
Answer: c) Chromosomal translocations
- Rapid IV infusion of etoposide may cause:
a) Hypertension
b) Bradycardia
c) Hypotension
d) Arrhythmia
Answer: c) Hypotension
- Etoposide differs from irinotecan because it inhibits:
a) Topoisomerase I
b) Topoisomerase II
c) Microtubules
d) DNA methylation
Answer: b) Topoisomerase II
- Alopecia caused by etoposide is due to:
a) Neuronal toxicity
b) Bone marrow failure
c) Damage to rapidly dividing cells
d) Hormonal imbalance
Answer: c) Damage to rapidly dividing cells
FAQs
1. Why is etoposide cell cycle specific?
Because it acts during DNA synthesis and repair phases.
2. What type of DNA breaks does etoposide cause?
Double-strand DNA breaks.
3. Can etoposide cross the blood–brain barrier?
No, CNS penetration is limited.
4. Why is secondary leukemia a concern?
Due to chromosomal damage from topoisomerase II inhibition.
5. Is etoposide used alone?
Usually in combination chemotherapy regimens.
References
- Goodman & Gilman’s The Pharmacological Basis of Therapeutics
https://accesspharmacy.mhmedical.com - Katzung BG. Basic and Clinical Pharmacology
https://accessmedicine.mhmedical.com - Tripathi KD. Essentials of Medical Pharmacology
- Harrison’s Principles of Internal Medicine
https://accessmedicine.mhmedical.com

I am pursuing MBA in pharmaceutical management from NIPER Hyderabad with a strong academic record and proven success in national-level pharmacy entrance exams. I secured AIR 61 in NIPER 2024 (MS/M.Pharm) and AIR 27 in NIPER MBA, along with AIR 147 in GPAT 2024 and AIR 907 in GPAT 2023. I also achieved AIR 6 in AIIMS CRE-2025 for Drug Store Keeper and was selected as a Pharmacist (AIR 61) for ESIC. Additionally, I was the Runner-Up in Round 2 of the EY Case Study Competition.
At PharmacyFreak.com, I aim to guide future pharmacists through expert content, exam strategies, and insightful resources based on real experience and academic excellence.
Mail- harsh@pharmacyfreak.com