Table of Contents
Introduction
Ethosuximide is an antiepileptic drug primarily used in the management of absence (petit mal) seizures. It is considered the drug of choice for absence seizures, making it extremely high-yield for pharmacology and neurology examinations. Ethosuximide acts selectively on thalamic neurons involved in seizure generation and has a relatively narrow but clinically important spectrum of activity.
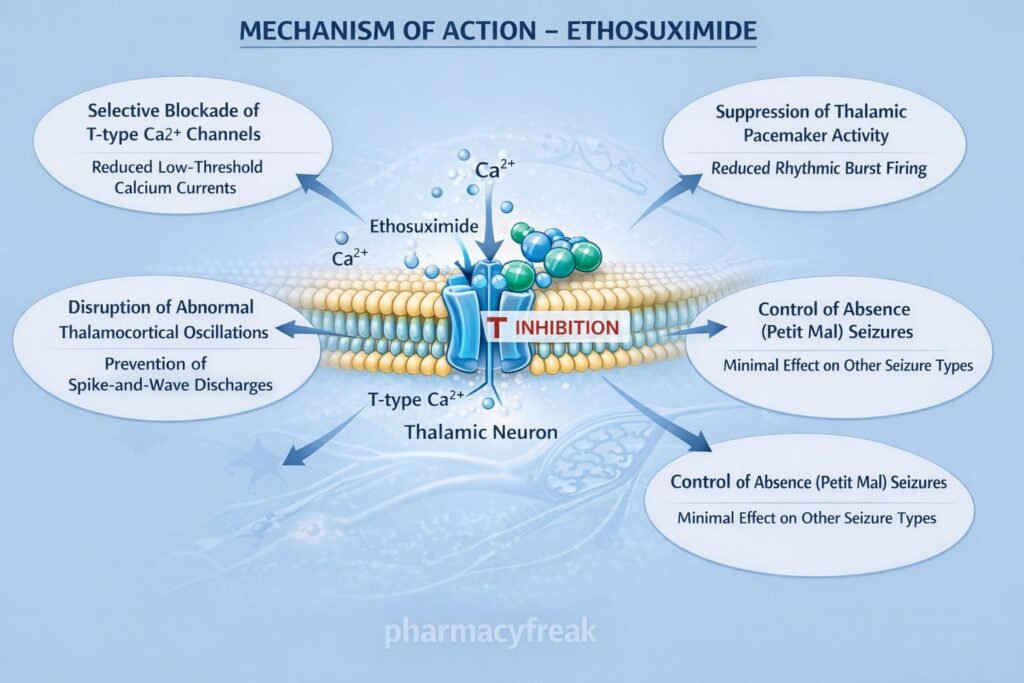
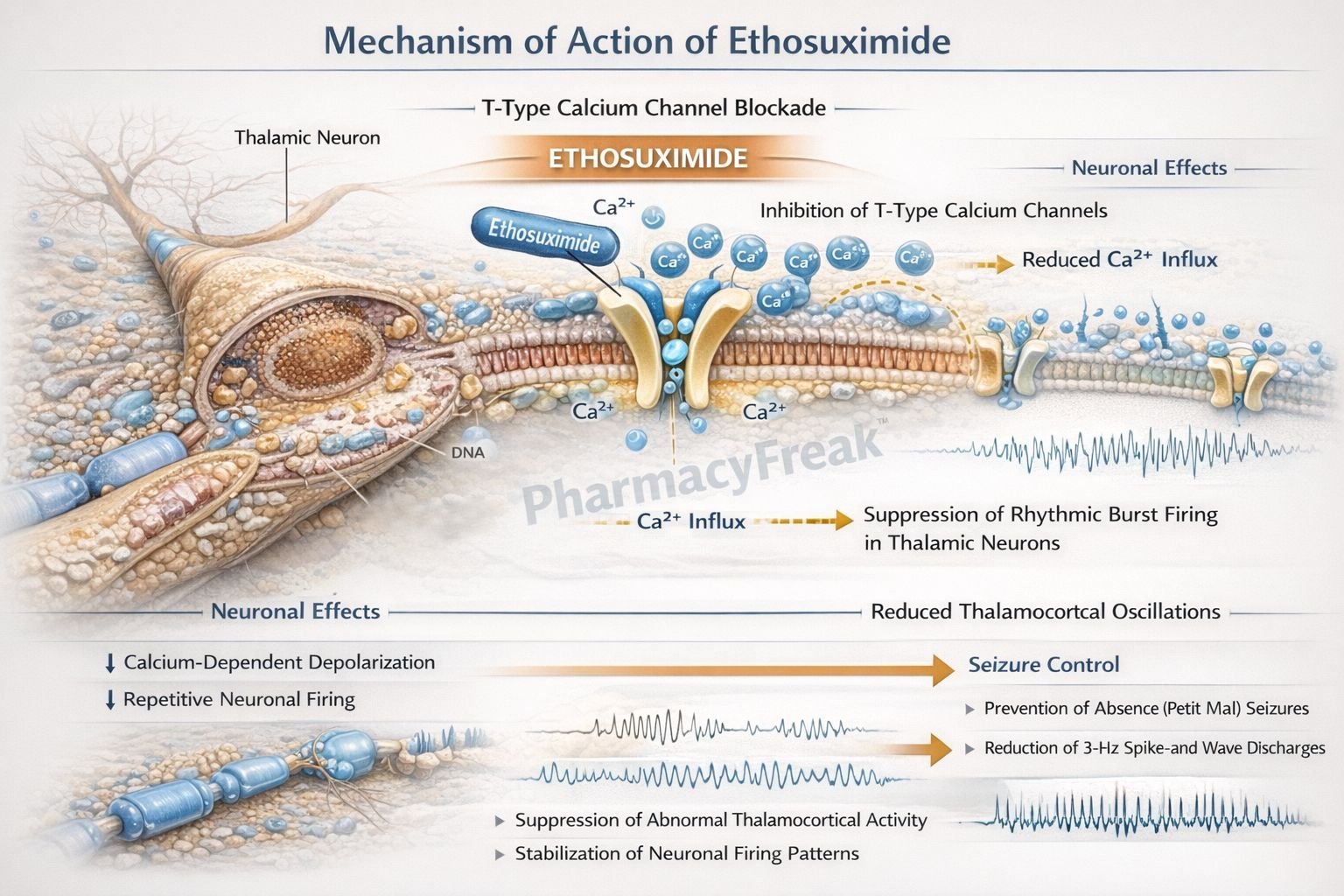
Mechanism of Action (Step-wise)
Ethosuximide suppresses absence seizures by inhibiting abnormal thalamocortical rhythmic activity.
Step 1: Targeting thalamic neurons
Ethosuximide acts predominantly on neurons in the thalamus, which play a key role in the generation of absence seizures.
Step 2: Inhibition of T-type calcium channels
It selectively blocks T-type (transient) voltage-gated calcium channels in thalamic neurons.
Step 3: Suppression of pacemaker currents
T-type calcium channels are responsible for rhythmic burst firing. Their inhibition reduces abnormal pacemaker activity.
Step 4: Reduction of thalamocortical oscillations
Blocking T-type calcium currents prevents synchronized thalamocortical discharges.
Step 5: Prevention of absence seizures
Suppression of spike-and-wave discharges (3 Hz) on EEG results in effective control of absence seizures.
Exam pearl:
Ethosuximide has no significant effect on sodium channels or GABA transmission.
Pharmacokinetics
- Route of administration: Oral
- Absorption: Complete and rapid
- Protein binding: Low
- Distribution: Widely distributed, including CNS
- Metabolism: Hepatic
- Half-life:
- Children: ~30 hours
- Adults: ~50–60 hours
- Excretion: Primarily renal (unchanged + metabolites)
- Dosing: Once or twice daily due to long half-life
Clinical Uses
- Absence seizures (first-line therapy)
- Childhood absence epilepsy
Ethosuximide is ineffective in focal seizures, tonic–clonic seizures, and myoclonic seizures.
Adverse Effects
Gastrointestinal (most common):
- Nausea
- Vomiting
- Abdominal pain
- Anorexia
Central nervous system:
- Fatigue
- Drowsiness
- Headache
- Dizziness
Psychiatric:
- Behavioral changes
- Irritability
- Rare psychosis
Hematological (rare):
- Leukopenia
- Thrombocytopenia
- Aplastic anemia
Dermatological:
- Stevens–Johnson syndrome (rare)
Classic exam mnemonic:
EFGHIJ – Ethosuximide causes Fatigue, GI distress, Headache, Itching, and Stevens–Johnson syndrome.
Comparative Analysis
Ethosuximide vs Valproate vs Phenytoin
| Feature | Ethosuximide | Valproate | Phenytoin |
|---|---|---|---|
| Primary seizure type | Absence | Broad-spectrum | Focal & GTCS |
| Main MOA | T-type Ca²⁺ block | Na⁺ block + GABA ↑ | Na⁺ channel block |
| EEG effect | ↓ 3 Hz spikes | ↓ multiple patterns | No effect on absence |
| Use in absence seizures | Drug of choice | Alternative | Ineffective |
| Major toxicity | GI distress | Hepatotoxicity | Gingival hyperplasia |
Explanation:
Ethosuximide is uniquely effective in absence seizures because it directly targets T-type calcium channels responsible for thalamic pacemaker activity. Valproate is an alternative when absence seizures coexist with other seizure types.
MCQs
- Ethosuximide is the drug of choice for:
a) Focal seizures
b) Tonic–clonic seizures
c) Absence seizures
d) Myoclonic seizures
Answer: c) Absence seizures
- Ethosuximide blocks which ion channel?
a) Sodium channel
b) L-type calcium channel
c) T-type calcium channel
d) Potassium channel
Answer: c) T-type calcium channel
- Site of action of ethosuximide is mainly the:
a) Hippocampus
b) Cerebellum
c) Thalamus
d) Brainstem
Answer: c) Thalamus
- Ethosuximide reduces which EEG abnormality?
a) Polyspike discharges
b) 3 Hz spike-and-wave pattern
c) Sharp waves
d) Burst suppression
Answer: b) 3 Hz spike-and-wave pattern
- Most common adverse effect of ethosuximide is:
a) Hepatotoxicity
b) Gingival hyperplasia
c) GI upset
d) Ataxia
Answer: c) GI upset
- Ethosuximide has no significant effect on:
a) Calcium channels
b) Sodium channels
c) Thalamic neurons
d) Absence seizures
Answer: b) Sodium channels
- Half-life of ethosuximide in adults is approximately:
a) 6 hours
b) 12 hours
c) 24 hours
d) 50–60 hours
Answer: d) 50–60 hours
- Which drug is preferred if absence seizures coexist with GTCS?
a) Ethosuximide
b) Carbamazepine
c) Valproate
d) Phenytoin
Answer: c) Valproate
- Ethosuximide adverse effect mnemonic EFGHIJ includes:
a) Hepatitis
b) Itching
c) Hypertension
d) Hypoglycemia
Answer: b) Itching
- Ethosuximide is ineffective in:
a) Absence seizures
b) Childhood epilepsy
c) Focal seizures
d) Thalamic seizures
Answer: c) Focal seizures
FAQs
1. Why is ethosuximide specific for absence seizures?
Because it blocks T-type calcium channels responsible for thalamic rhythmic firing.
2. Does ethosuximide affect sodium channels?
No, it has minimal effect on sodium channels.
3. What EEG abnormality does ethosuximide suppress?
The 3 Hz spike-and-wave pattern.
4. Can ethosuximide be used in tonic–clonic seizures?
No, it is ineffective.
5. What is the most common adverse effect?
Gastrointestinal distress.
References
- Goodman & Gilman’s The Pharmacological Basis of Therapeutics
https://accesspharmacy.mhmedical.com - Katzung BG. Basic and Clinical Pharmacology
https://accessmedicine.mhmedical.com - Tripathi KD. Essentials of Medical Pharmacology
- Harrison’s Principles of Internal Medicine
https://accessmedicine.mhmedical.com

I am pursuing MBA in pharmaceutical management from NIPER Hyderabad with a strong academic record and proven success in national-level pharmacy entrance exams. I secured AIR 61 in NIPER 2024 (MS/M.Pharm) and AIR 27 in NIPER MBA, along with AIR 147 in GPAT 2024 and AIR 907 in GPAT 2023. I also achieved AIR 6 in AIIMS CRE-2025 for Drug Store Keeper and was selected as a Pharmacist (AIR 61) for ESIC. Additionally, I was the Runner-Up in Round 2 of the EY Case Study Competition.
At PharmacyFreak.com, I aim to guide future pharmacists through expert content, exam strategies, and insightful resources based on real experience and academic excellence.
Mail- harsh@pharmacyfreak.com