Table of Contents
Introduction
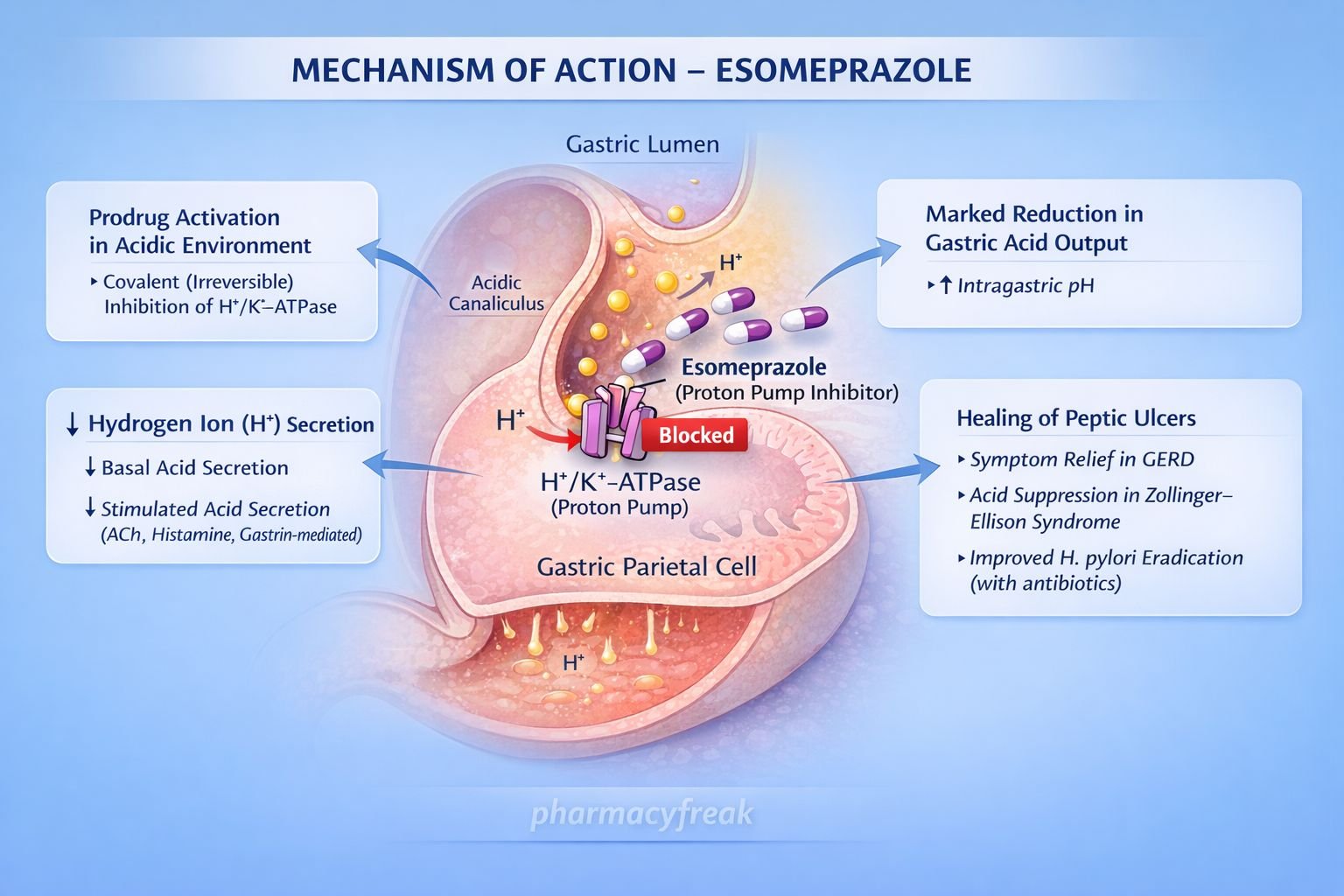
Esomeprazole is a proton pump inhibitor (PPI) used extensively in the treatment of acid-related gastrointestinal disorders. It is the S-isomer of omeprazole and offers improved pharmacokinetic consistency and acid suppression compared with the racemic mixture. Esomeprazole is a high-yield drug for pharmacology and clinical examinations due to its irreversible enzyme inhibition, acid-activated mechanism, and role in peptic ulcer disease and gastroesophageal reflux disease.
Mechanism of Action (Step-wise)
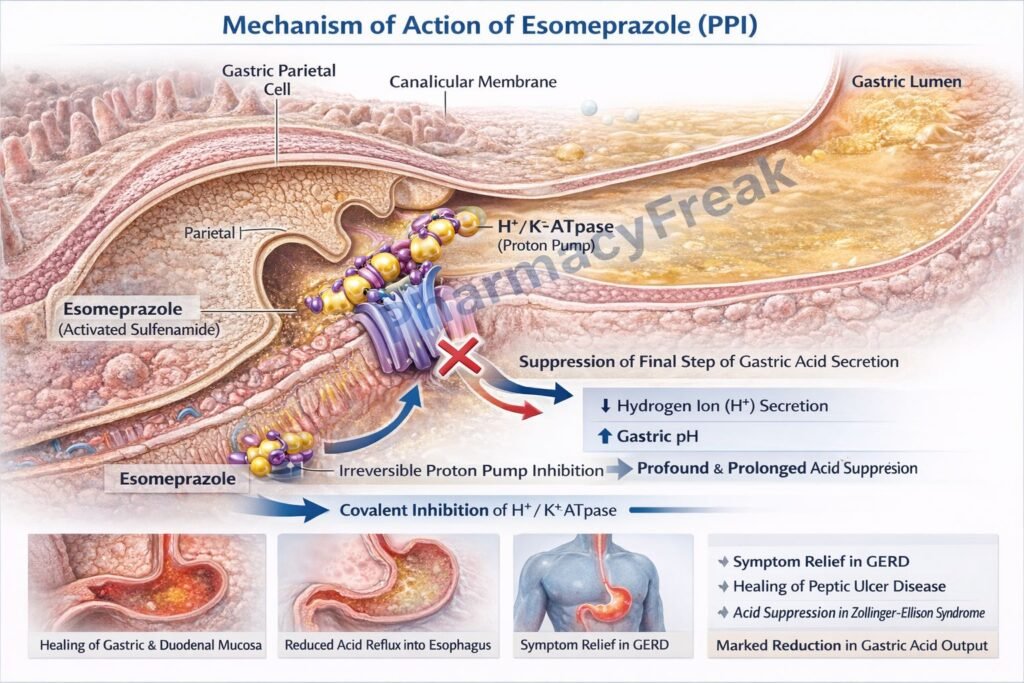
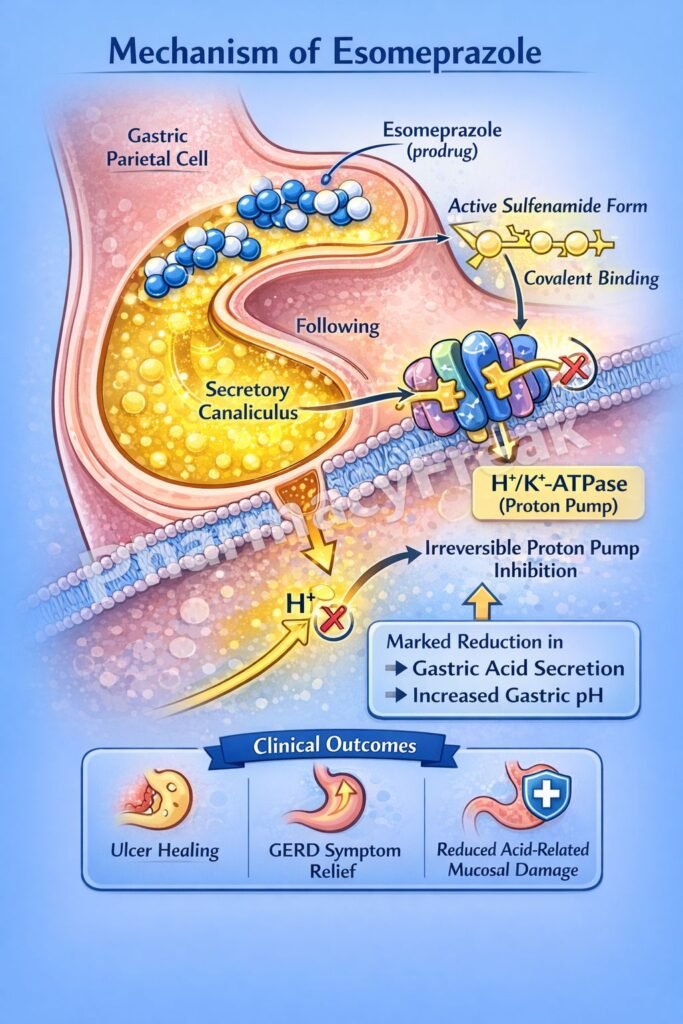
Esomeprazole suppresses gastric acid secretion by irreversible inhibition of the proton pump in gastric parietal cells.
Step 1: Prodrug administration
Esomeprazole is administered orally as an acid-labile prodrug protected by an enteric coating.
Step 2: Absorption and systemic distribution
After absorption in the small intestine, esomeprazole enters the systemic circulation and is delivered to gastric parietal cells.
Step 3: Activation in acidic environment
Within the acidic secretory canaliculi of parietal cells, esomeprazole is protonated and converted to its active sulfenamide form.
Step 4: Irreversible inhibition of H⁺/K⁺-ATPase
The activated drug covalently binds to sulfhydryl groups of the H⁺/K⁺-ATPase (proton pump) on the luminal surface of parietal cells.
Step 5: Suppression of gastric acid secretion
Inhibition of the final common pathway of acid secretion results in profound and long-lasting reduction of basal and stimulated gastric acid output.
Pharmacokinetics
- Route of administration: Oral, IV
- Bioavailability: ~60% (increases with repeated dosing)
- Protein binding: ~97%
- Distribution: Concentrates in parietal cells
- Metabolism: Hepatic (CYP2C19 and CYP3A4)
- Half-life: 1–1.5 hours
- Duration of action: 24–48 hours (due to irreversible enzyme inhibition)
- Excretion: Urine and feces as inactive metabolites
Clinical Uses
- Gastroesophageal reflux disease (GERD)
- Erosive esophagitis
- Peptic ulcer disease
- Helicobacter pylori eradication (in combination therapy)
- Zollinger–Ellison syndrome
- NSAID-induced ulcer prophylaxis
- Stress ulcer prophylaxis (IV use in hospitalized patients)
Adverse Effects
Common:
- Headache
- Nausea
- Diarrhea
- Abdominal pain
Long-term use:
- Vitamin B₁₂ deficiency
- Hypomagnesemia
- Increased risk of fractures
- Increased risk of Clostridioides difficile infection
Renal:
- Acute interstitial nephritis (rare)
Gastric:
- Hypergastrinemia
- Rebound acid hypersecretion after withdrawal
Comparative Analysis
Esomeprazole vs Omeprazole vs Pantoprazole
| Feature | Esomeprazole | Omeprazole | Pantoprazole |
|---|---|---|---|
| Isomer | S-isomer | Racemic | Single compound |
| Acid suppression | Strong | Moderate | Moderate |
| CYP2C19 variability | Less | More | Minimal |
| Drug interactions | Moderate | Higher | Low |
| Duration of effect | Long | Long | Long |
Explanation:
Esomeprazole provides more consistent acid suppression than omeprazole due to reduced first-pass metabolism variability. Pantoprazole has fewer drug interactions, making it preferable in patients receiving multiple medications.
MCQs
- Esomeprazole inhibits gastric acid secretion by blocking:
a) H₂ receptors
b) Carbonic anhydrase
c) H⁺/K⁺-ATPase
d) Na⁺/K⁺-ATPase
Answer: c) H⁺/K⁺-ATPase
- Esomeprazole is activated in the:
a) Liver
b) Blood
c) Acidic canaliculi of parietal cells
d) Intestinal lumen
Answer: c) Acidic canaliculi of parietal cells
- Nature of enzyme inhibition by esomeprazole is:
a) Competitive
b) Non-competitive
c) Reversible
d) Irreversible
Answer: d) Irreversible
- Duration of action of esomeprazole exceeds its plasma half-life because of:
a) High protein binding
b) Active metabolites
c) Irreversible proton pump inhibition
d) Slow renal excretion
Answer: c) Irreversible proton pump inhibition
- Esomeprazole primarily reduces:
a) Histamine release
b) Gastrin secretion
c) Final step of acid secretion
d) Pepsin production
Answer: c) Final step of acid secretion
- Long-term PPI use is associated with deficiency of:
a) Iron
b) Vitamin B₁₂
c) Folate
d) Vitamin K
Answer: b) Vitamin B₁₂
- Esomeprazole is best taken:
a) With meals
b) At bedtime
c) Before meals
d) After meals
Answer: c) Before meals
- Esomeprazole metabolism mainly involves:
a) CYP1A2
b) CYP2C19
c) MAO
d) COMT
Answer: b) CYP2C19
- Rebound acid hypersecretion occurs due to:
a) Reduced gastrin levels
b) Increased parietal cell mass
c) Enzyme induction
d) Reduced drug absorption
Answer: b) Increased parietal cell mass
- Preferred indication for IV esomeprazole is:
a) Functional dyspepsia
b) Stress ulcer prophylaxis
c) Motion sickness
d) IBS
Answer: b) Stress ulcer prophylaxis
FAQs
1. Why is esomeprazole more effective than omeprazole?
It is the active S-isomer with more predictable pharmacokinetics.
2. Why does esomeprazole have a long duration of action?
Because it irreversibly inhibits the proton pump.
3. Can esomeprazole be used long term?
Yes, but monitoring for nutrient deficiencies is recommended.
4. Why should esomeprazole be taken before meals?
Proton pumps are most active after food intake.
5. Does esomeprazole affect calcium absorption?
Yes, long-term use may reduce calcium absorption.
References
- Goodman & Gilman’s The Pharmacological Basis of Therapeutics
https://accesspharmacy.mhmedical.com - Katzung BG. Basic and Clinical Pharmacology
https://accessmedicine.mhmedical.com - Tripathi KD. Essentials of Medical Pharmacology
- Harrison’s Principles of Internal Medicine
https://accessmedicine.mhmedical.com

I am pursuing MBA in pharmaceutical management from NIPER Hyderabad with a strong academic record and proven success in national-level pharmacy entrance exams. I secured AIR 61 in NIPER 2024 (MS/M.Pharm) and AIR 27 in NIPER MBA, along with AIR 147 in GPAT 2024 and AIR 907 in GPAT 2023. I also achieved AIR 6 in AIIMS CRE-2025 for Drug Store Keeper and was selected as a Pharmacist (AIR 61) for ESIC. Additionally, I was the Runner-Up in Round 2 of the EY Case Study Competition.
At PharmacyFreak.com, I aim to guide future pharmacists through expert content, exam strategies, and insightful resources based on real experience and academic excellence.
Mail- harsh@pharmacyfreak.com