Mechanism of Action of Drugs
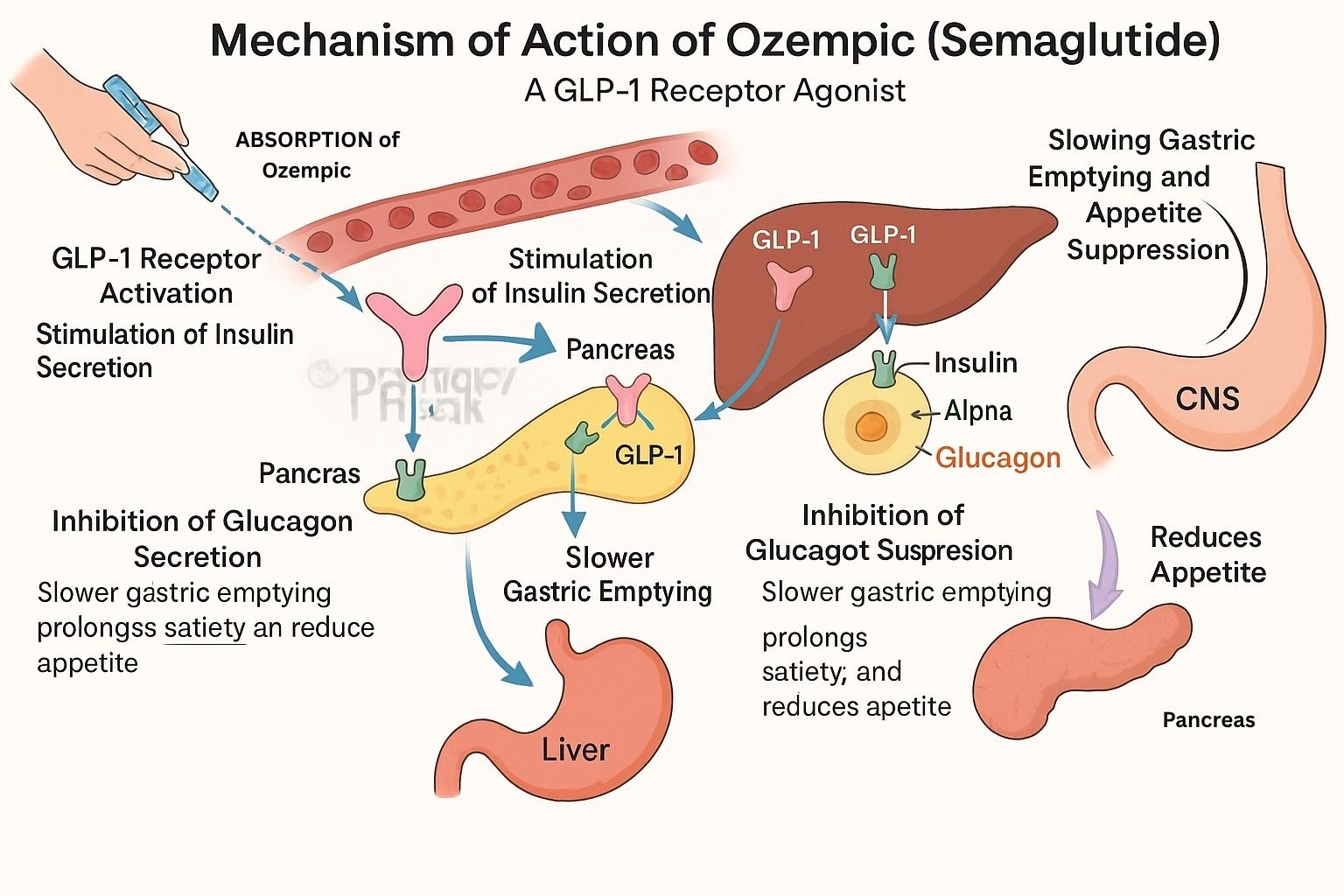
Introduction
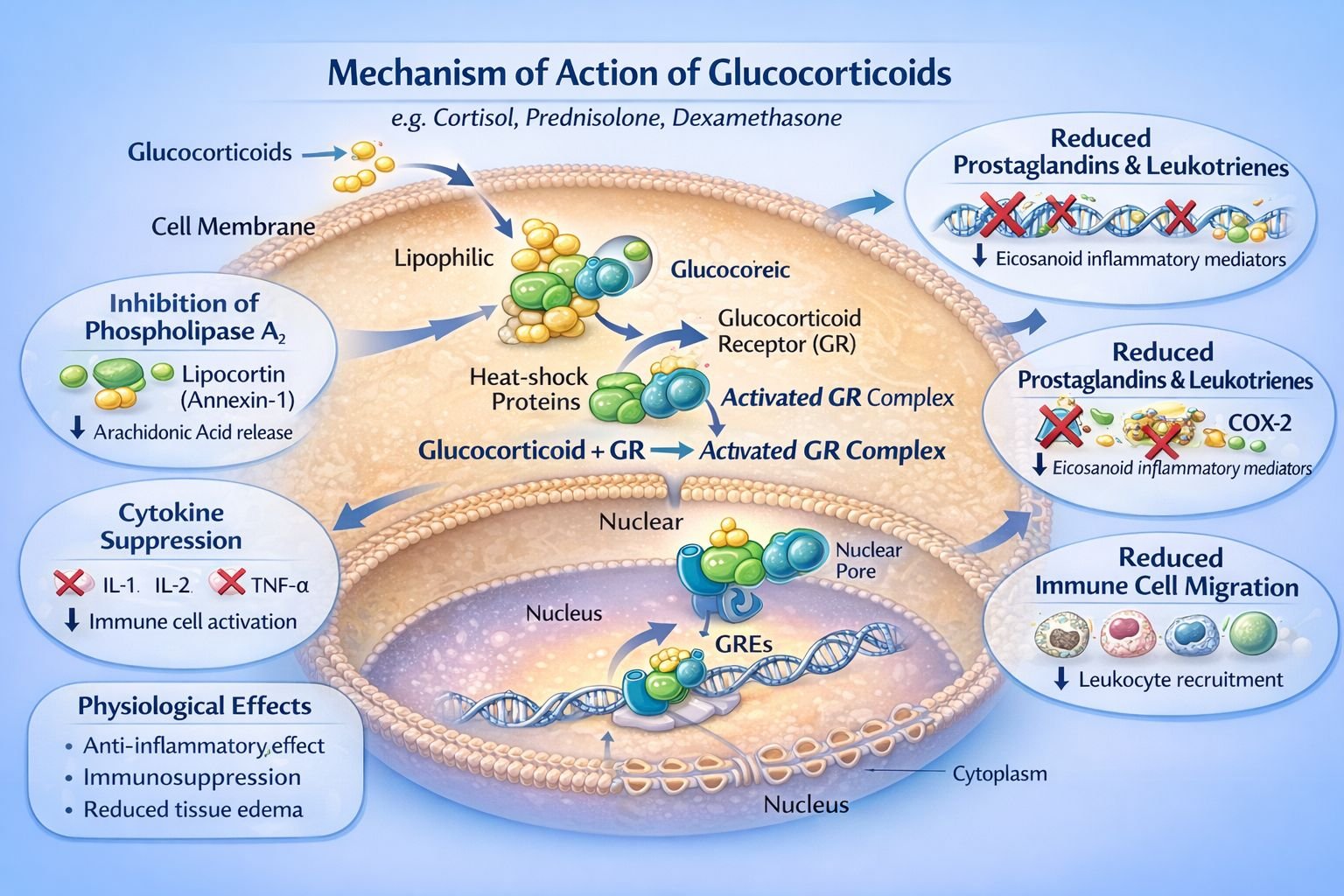
Understanding the mechanism of action (MOA) of drugs is a cornerstone of pharmacology and essential for all medical students. The MOA describes the specific biochemical interaction through which a drug produces its pharmacological effect. This involves how a drug binds to a target, the changes it causes at a molecular or cellular level, and how those changes translate into clinical effects. By grasping these principles, medical students can make sense of why drugs are effective, predict possible side effects, and anticipate drug interactions.
This article will explain the major principles behind the mechanisms of action of drugs, the different types of drug targets, and provide multiple examples to build a solid foundation. The aim is to create a reference page that you can revisit while studying individual drugs.
Why Study Mechanism of Action?
Learning about a drug’s mechanism of action is not just an academic exercise. There are several practical reasons why this knowledge is vital in medical practice:
Rational Drug Selection: Understanding MOA helps in choosing the best drug for a specific disease or symptom.
Anticipating Adverse Effects: Many side effects are predictable once you know how a drug works.
Avoiding Drug Interactions: Some drugs work on the same targets or pathways, which can lead to interactions.
Personalizing Therapy: MOA can guide personalized treatment, especially in cases like cancer therapy or infectious diseases.
Developing New Drugs: Most new drug development is based on modifying existing mechanisms or discovering new targets.
Basic Principles of Drug Action
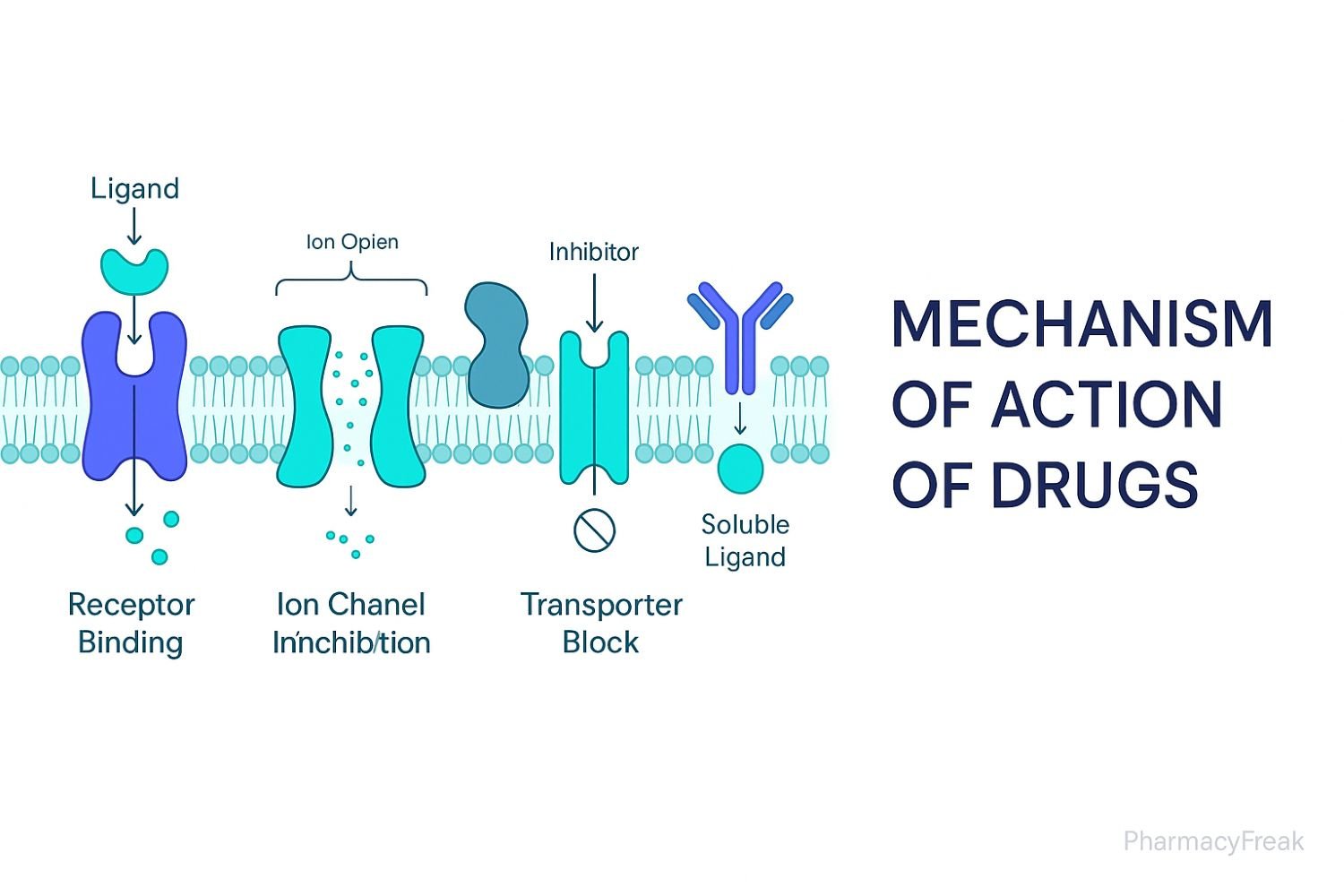
Drugs act by altering normal physiological or biochemical processes in the body. Most drugs do not create new functions but modify existing ones. The main ways drugs produce their effects include:
Interacting with Receptors
Inhibiting or Activating Enzymes
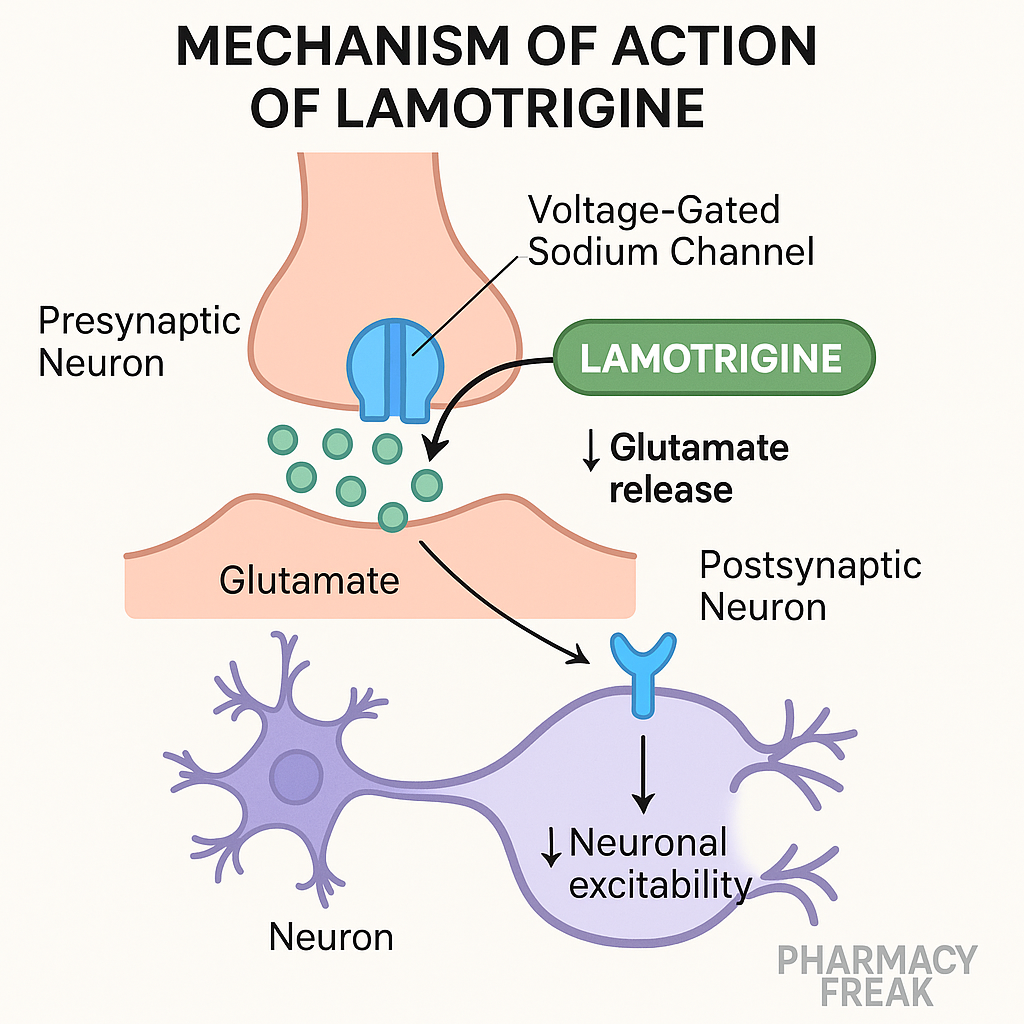
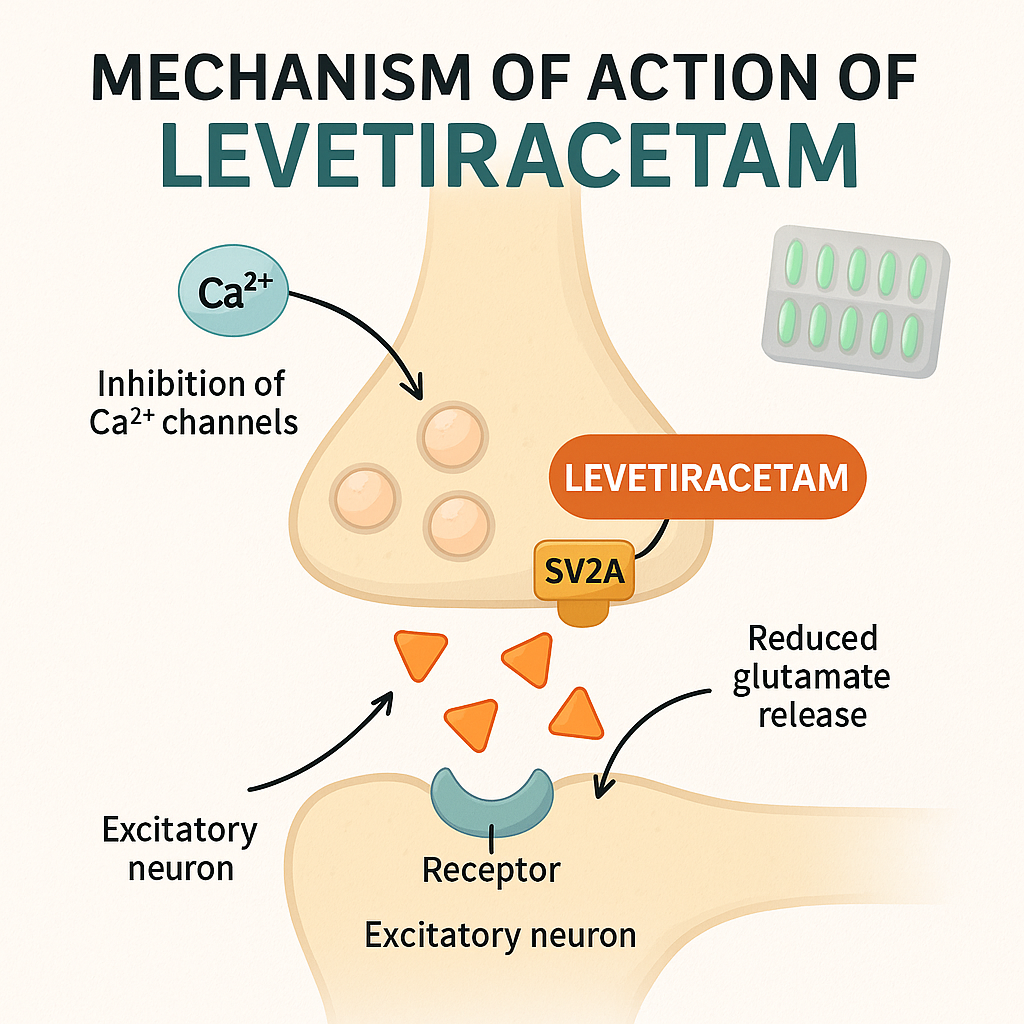
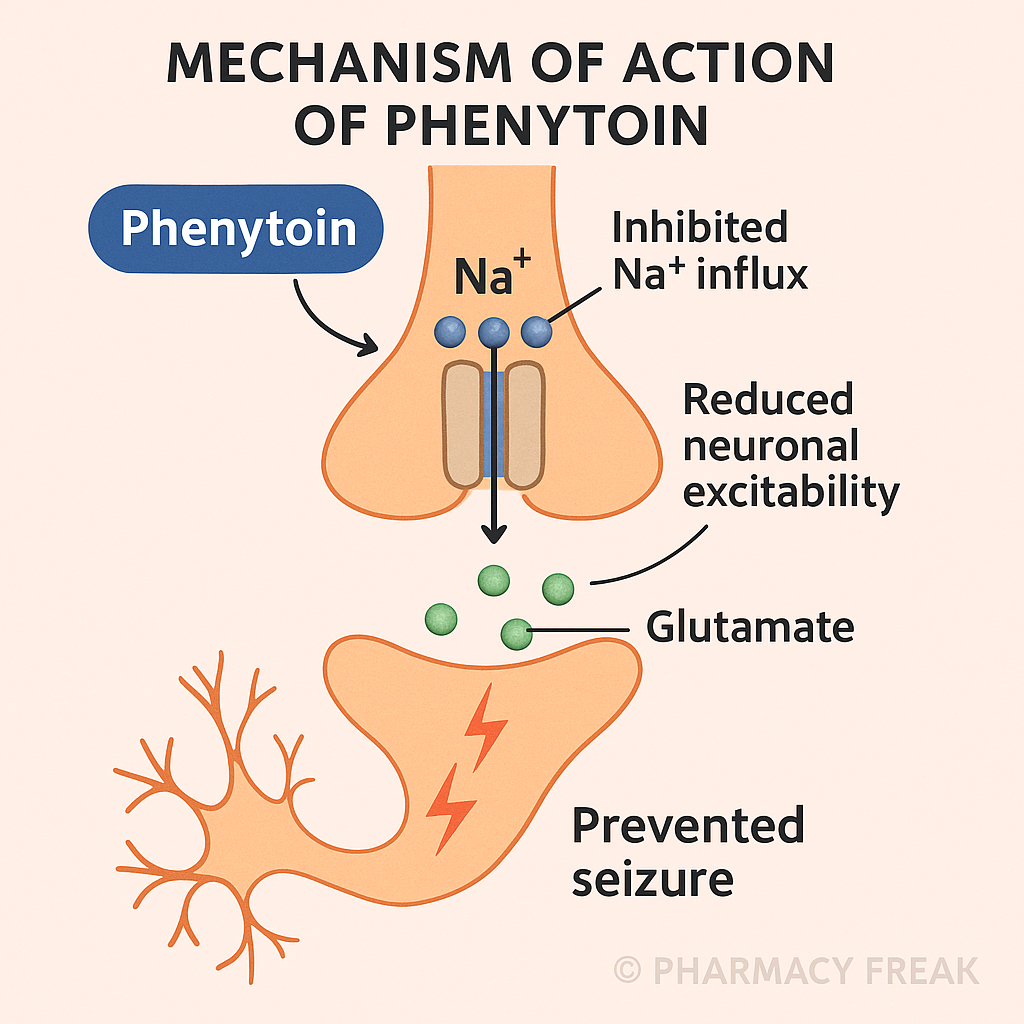
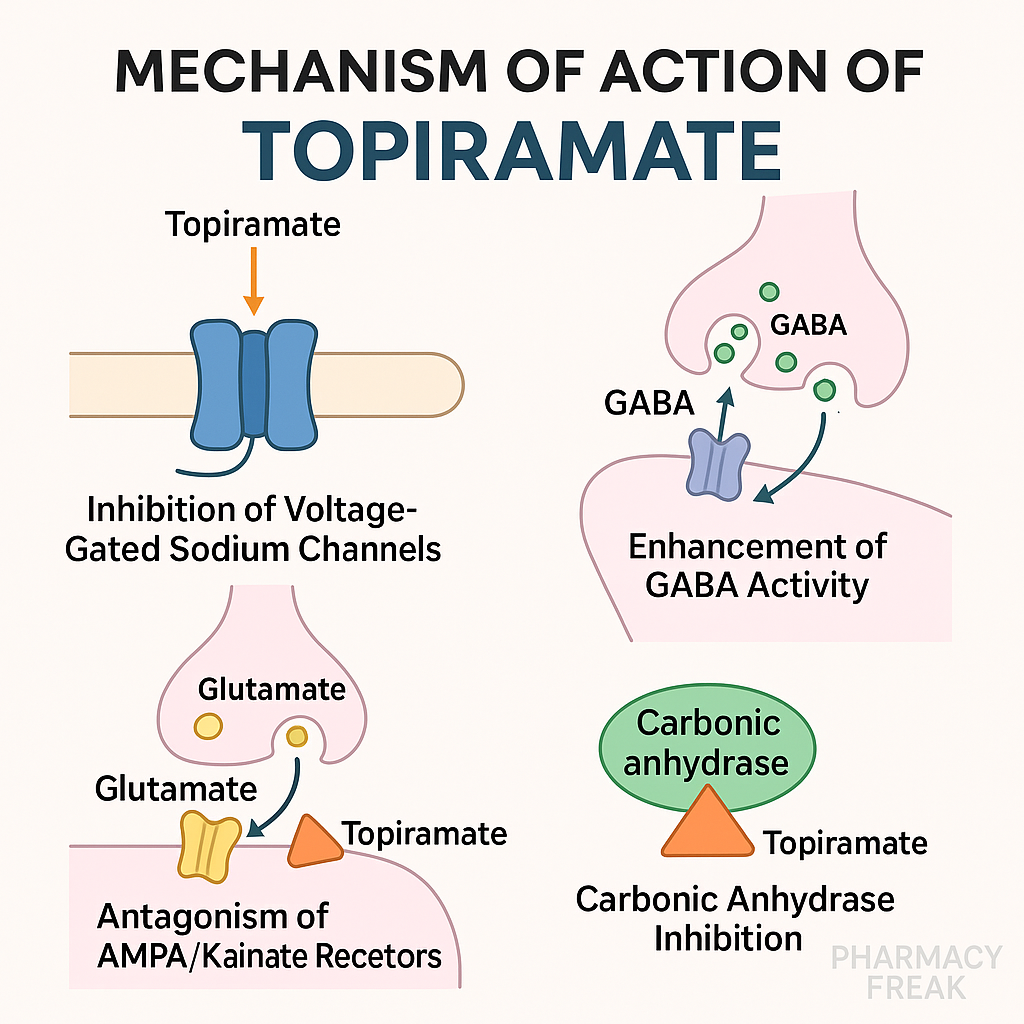
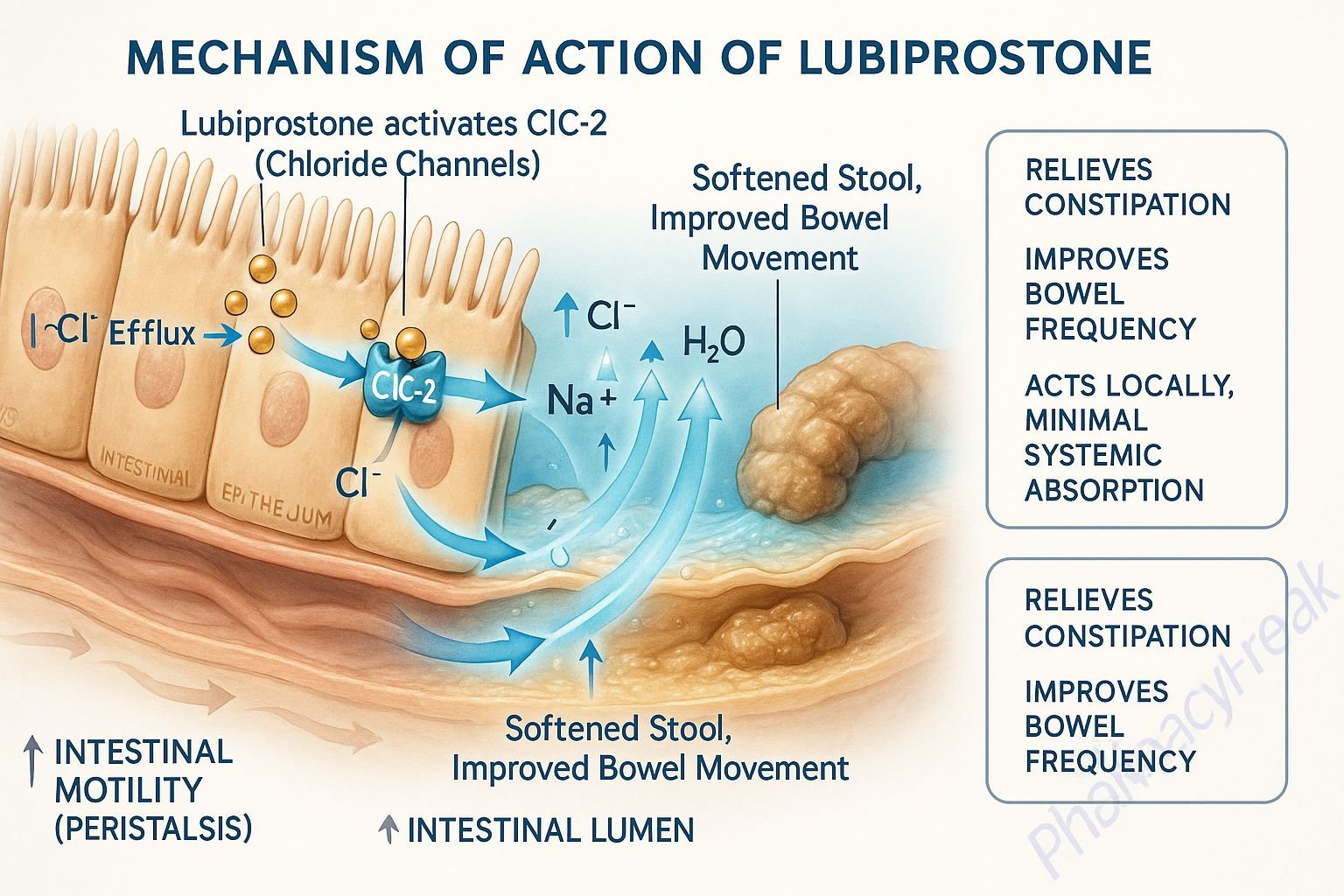
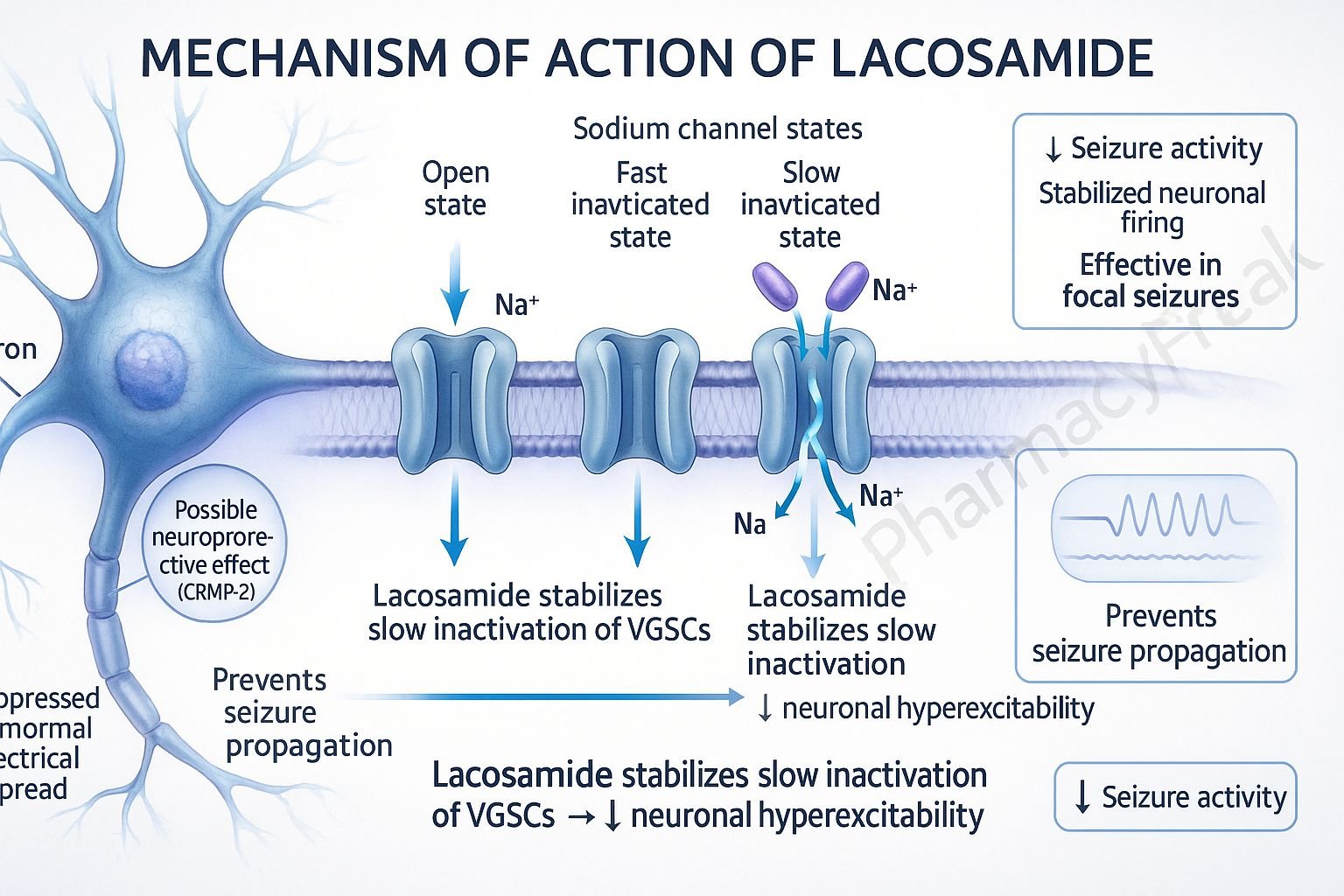
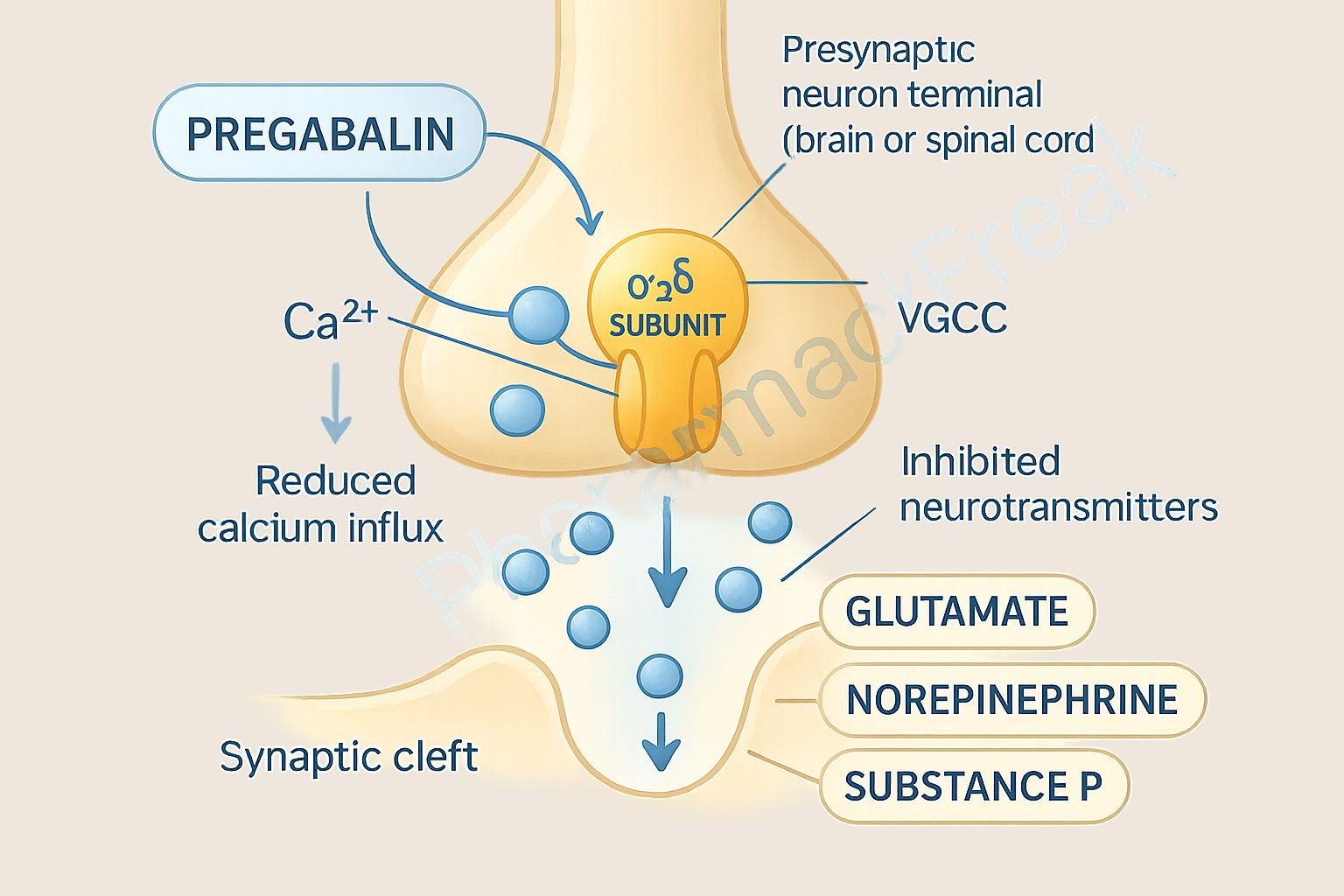
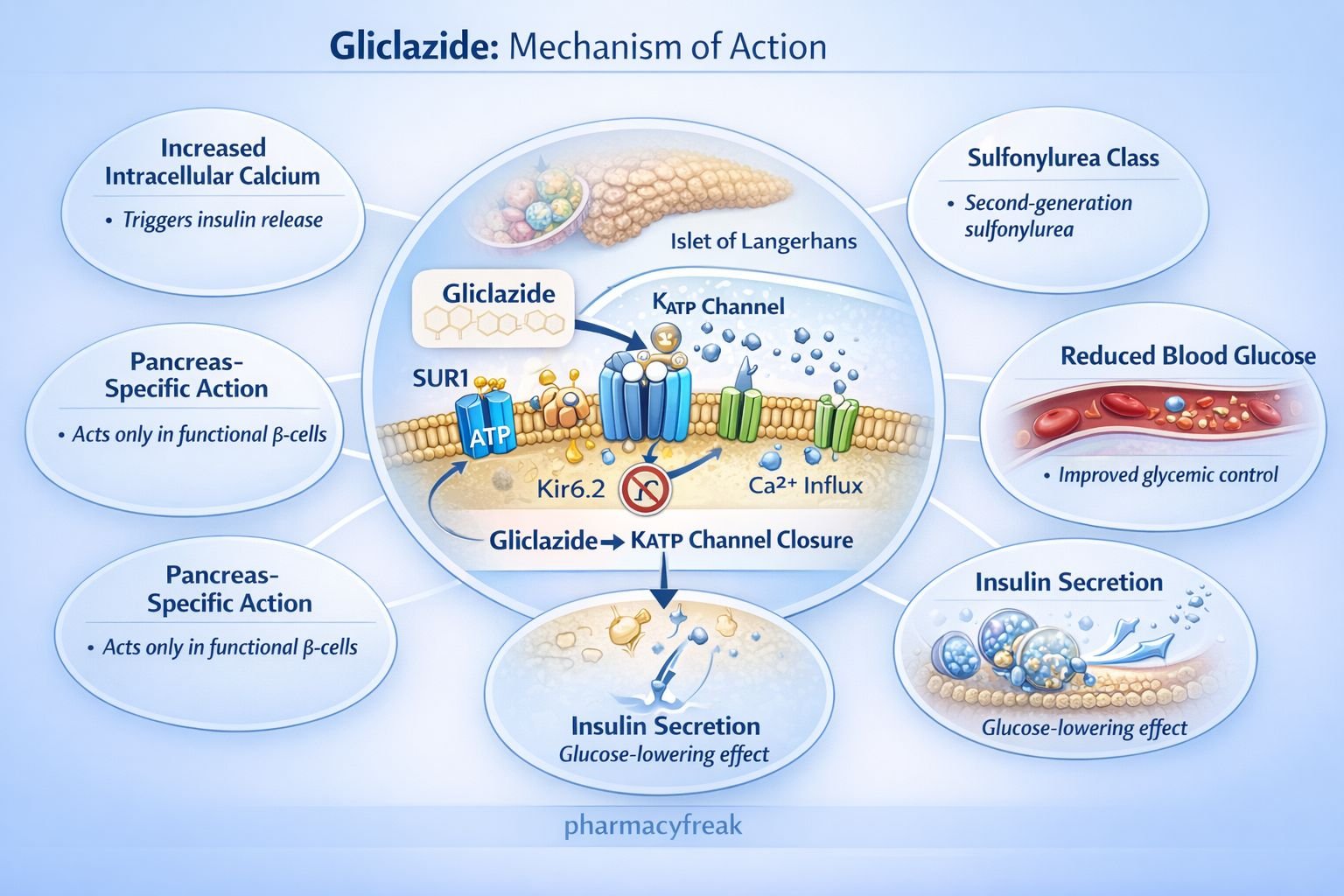
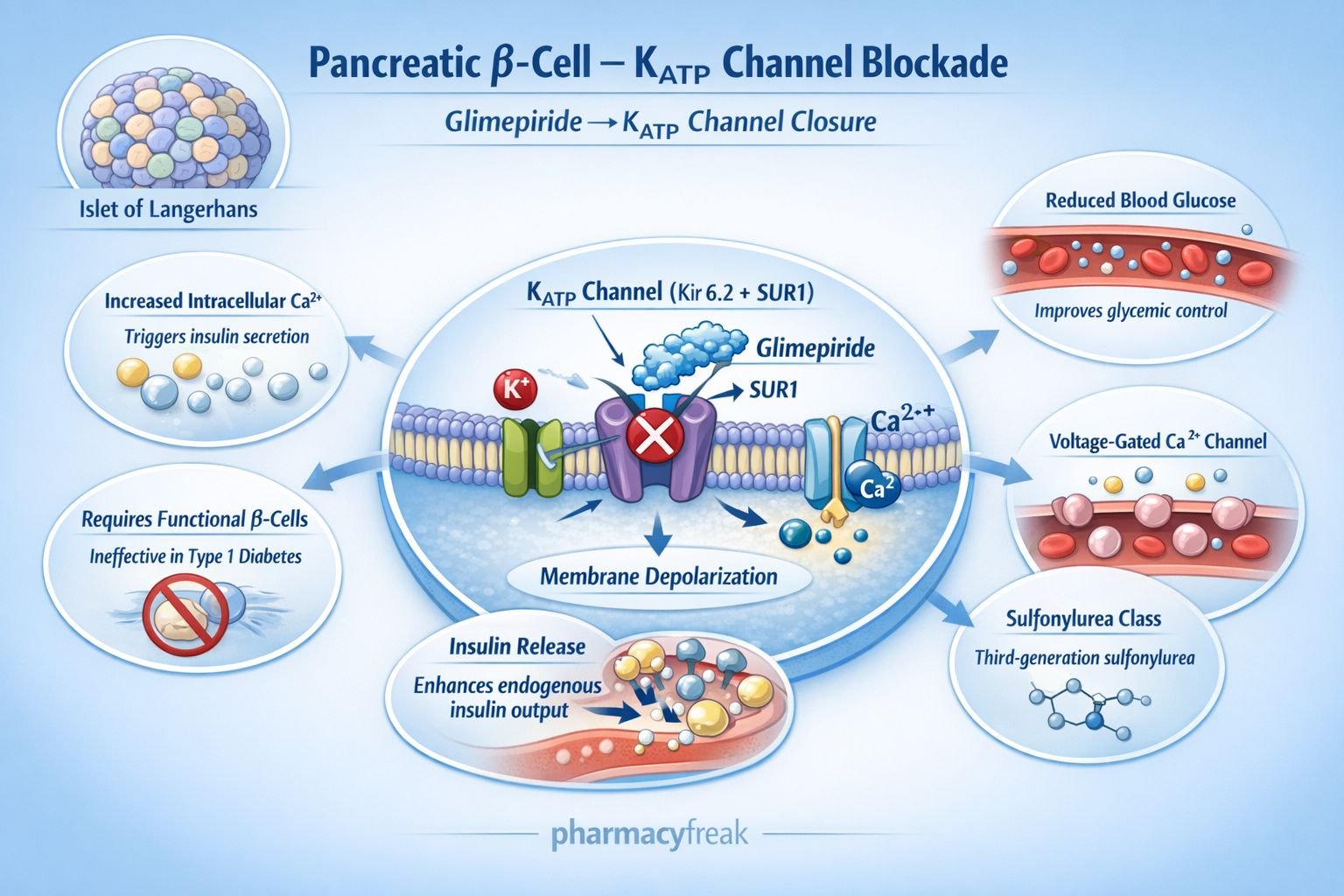
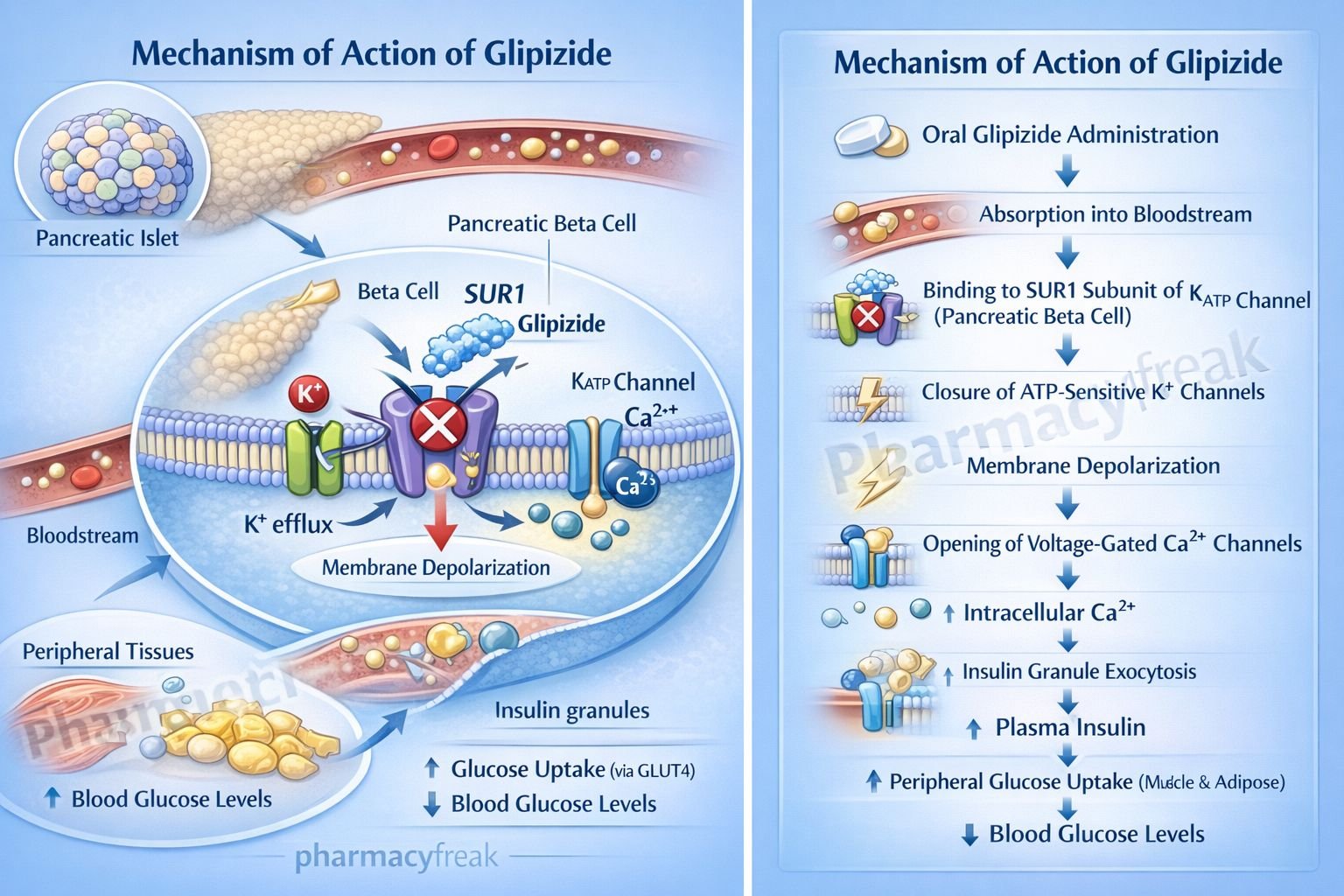
Blocking or Opening Ion Channels
Affecting Transporters and Carrier Proteins
Direct Physical or Chemical Action
Let’s examine each in detail.
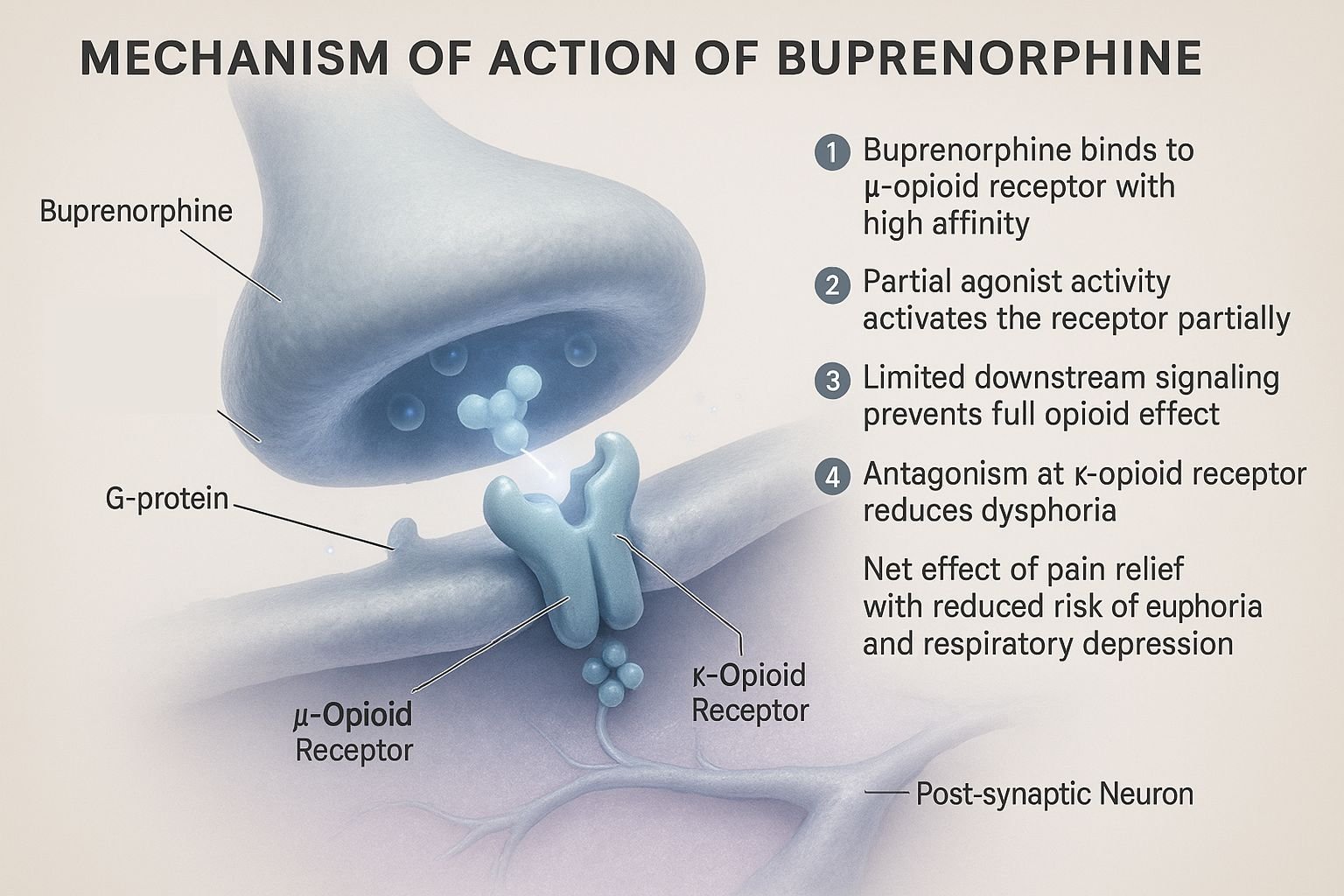
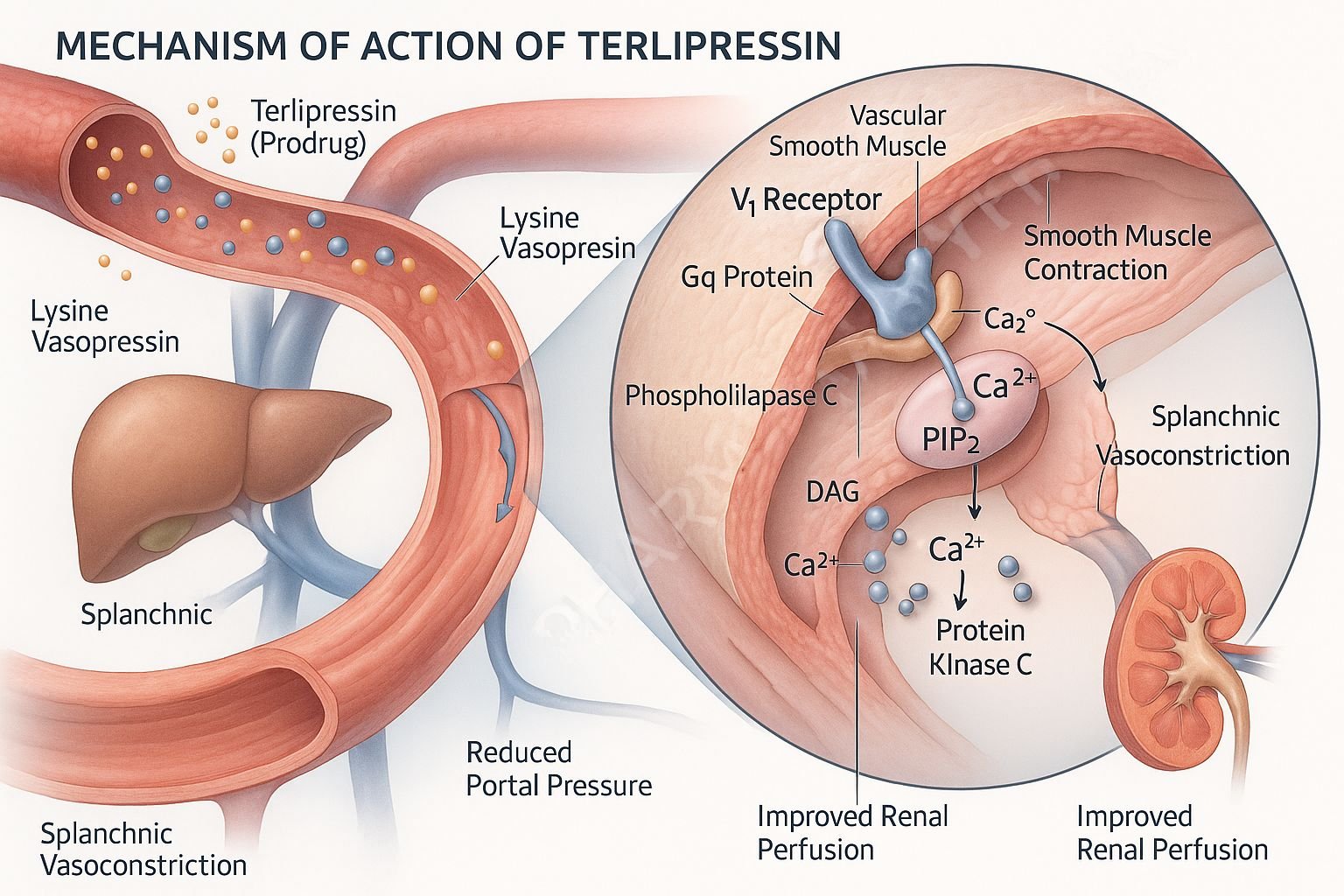
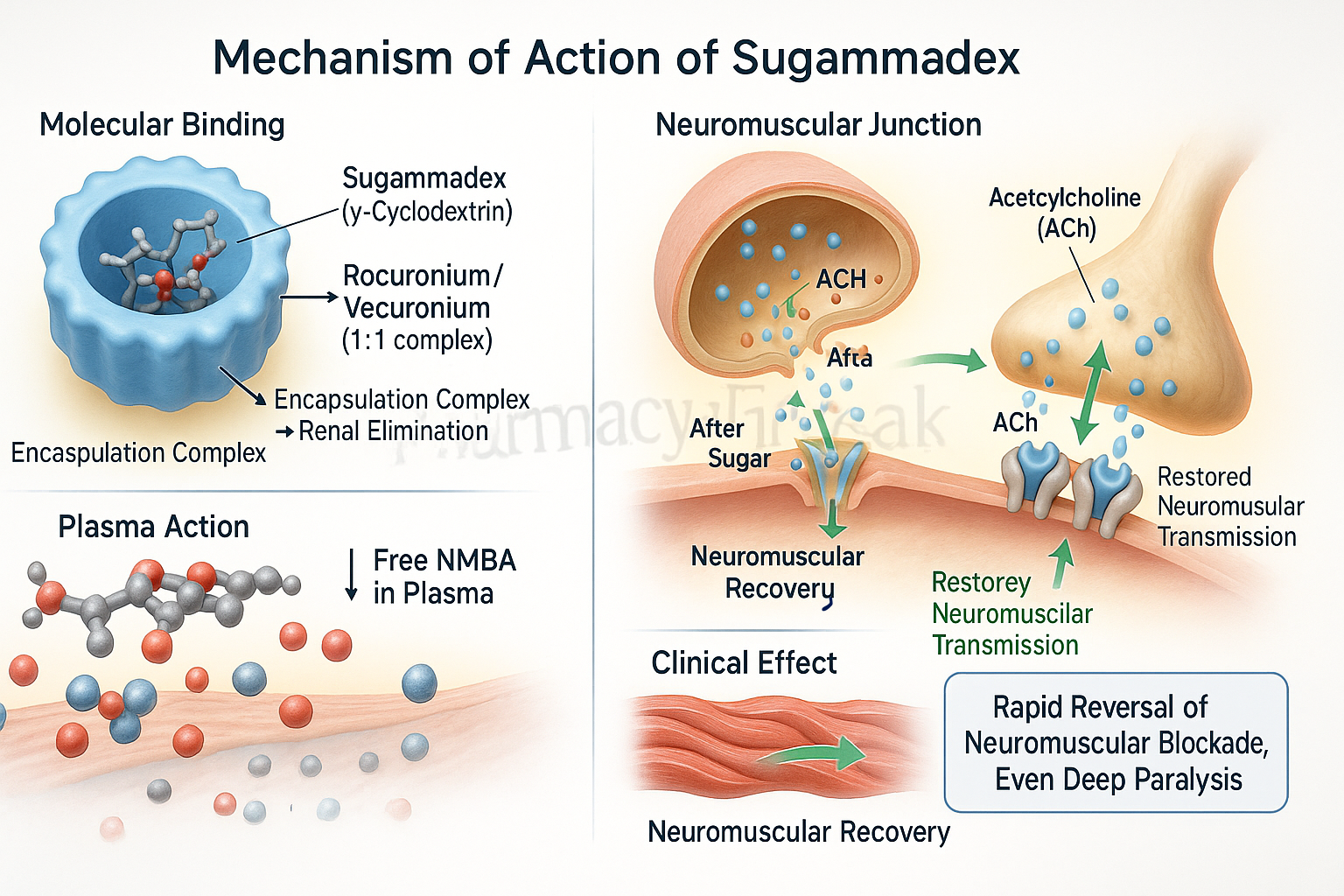
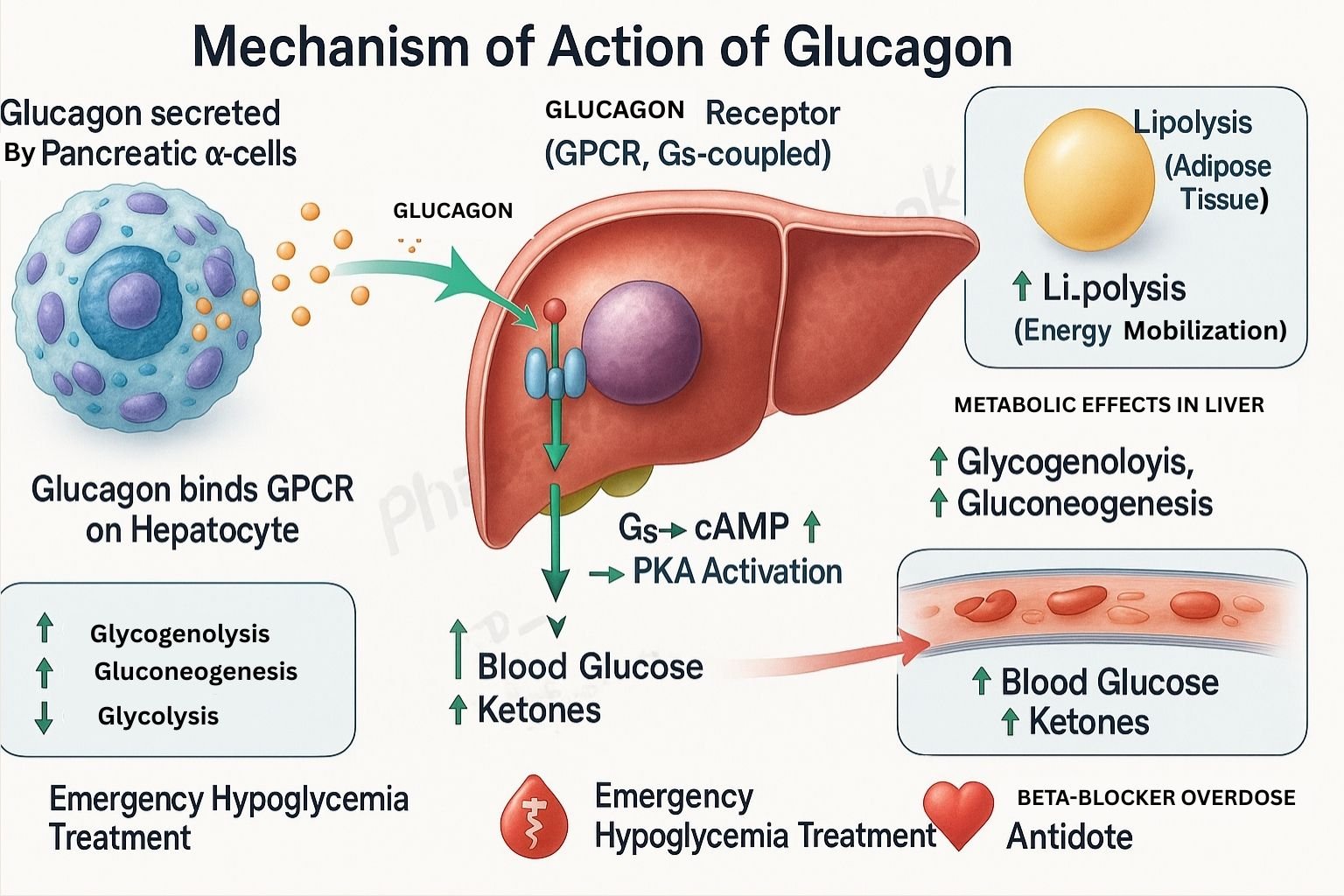
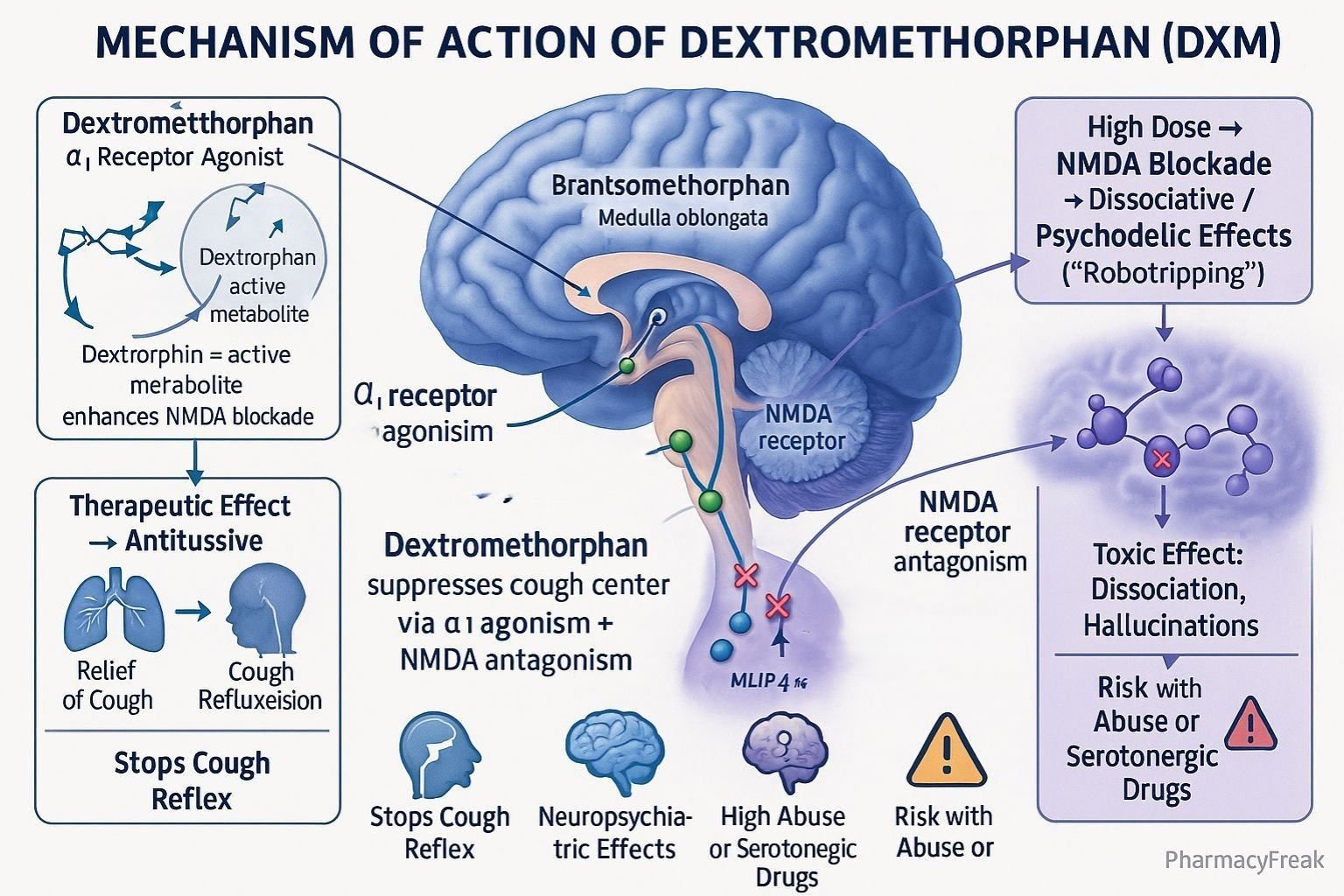
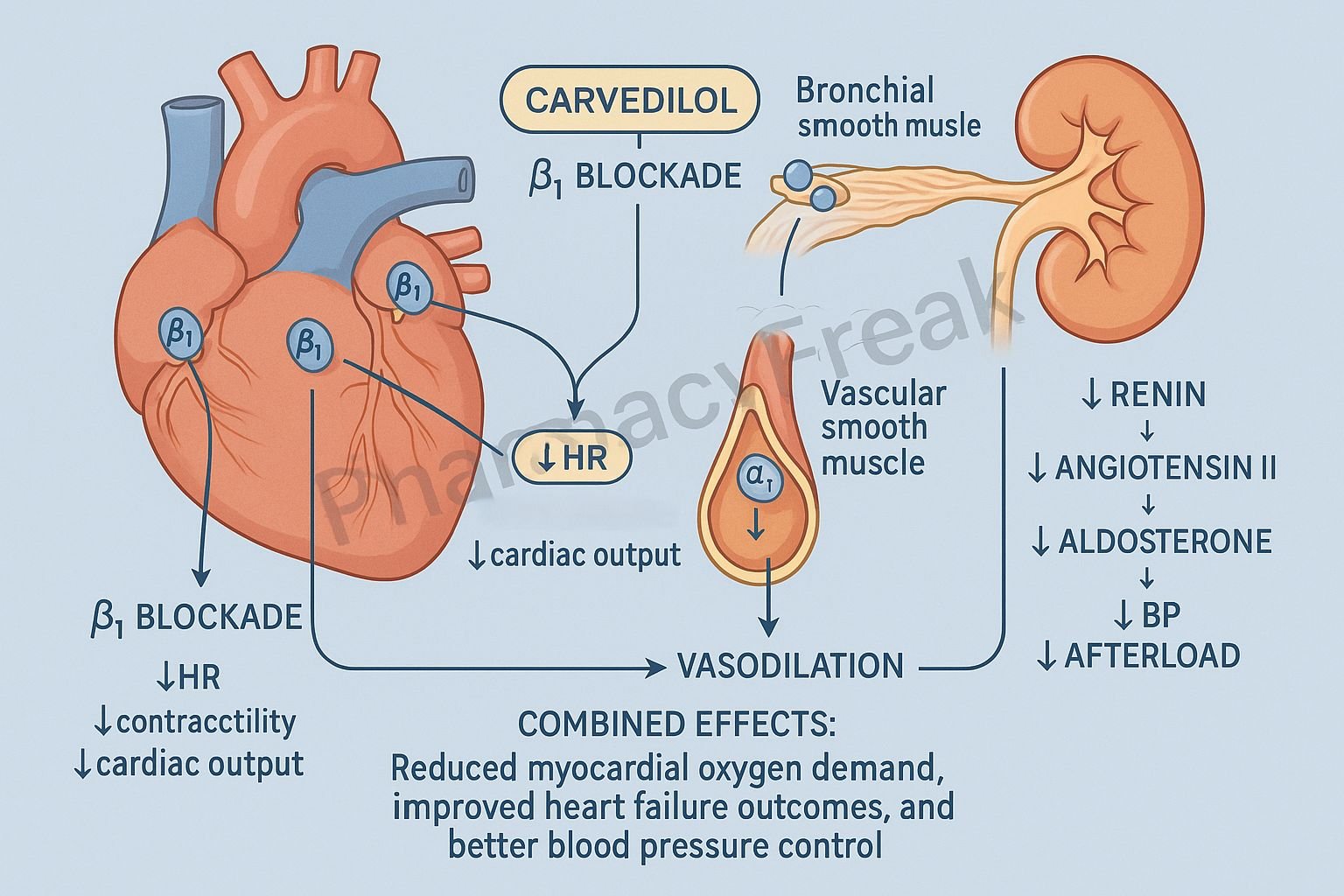
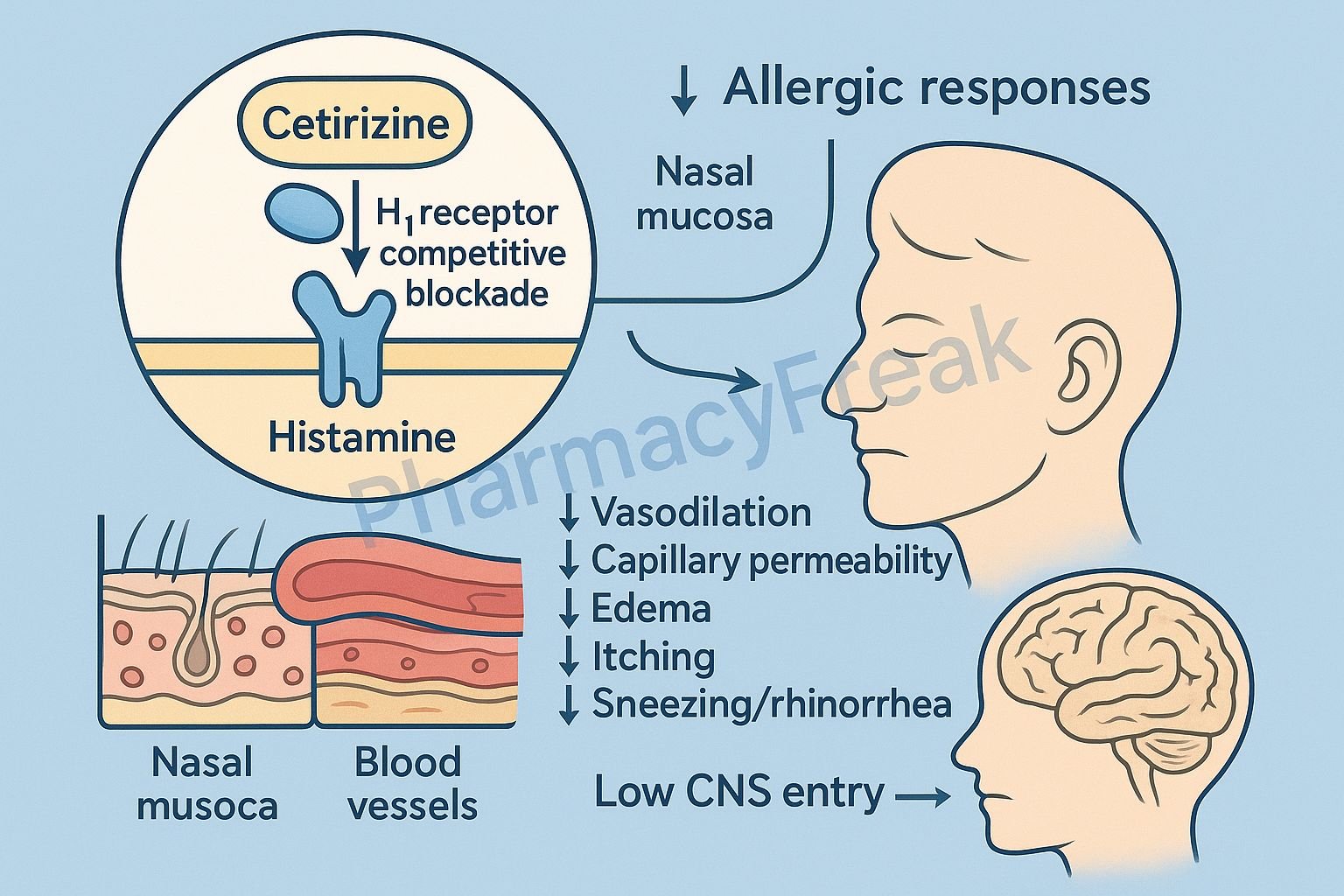
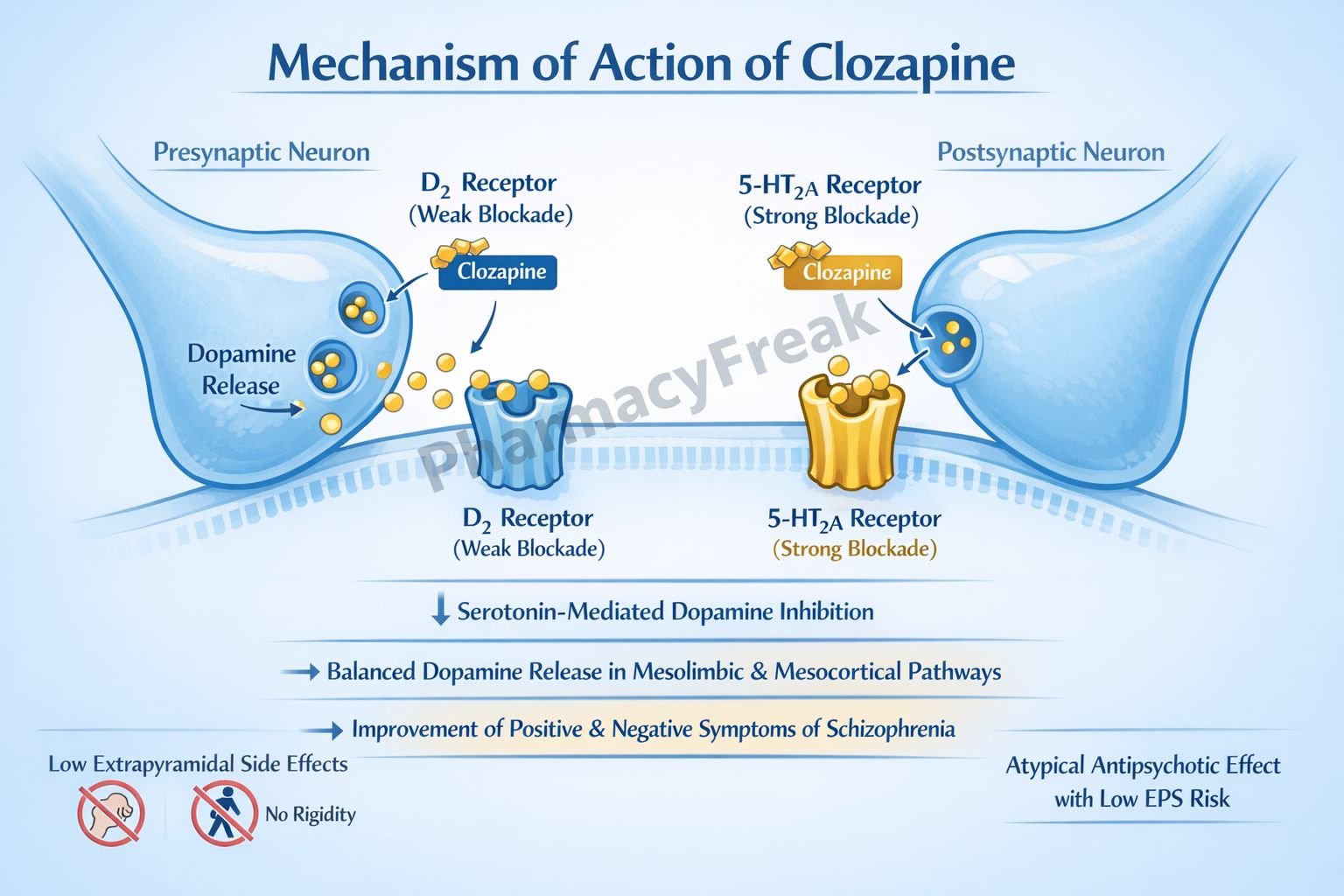
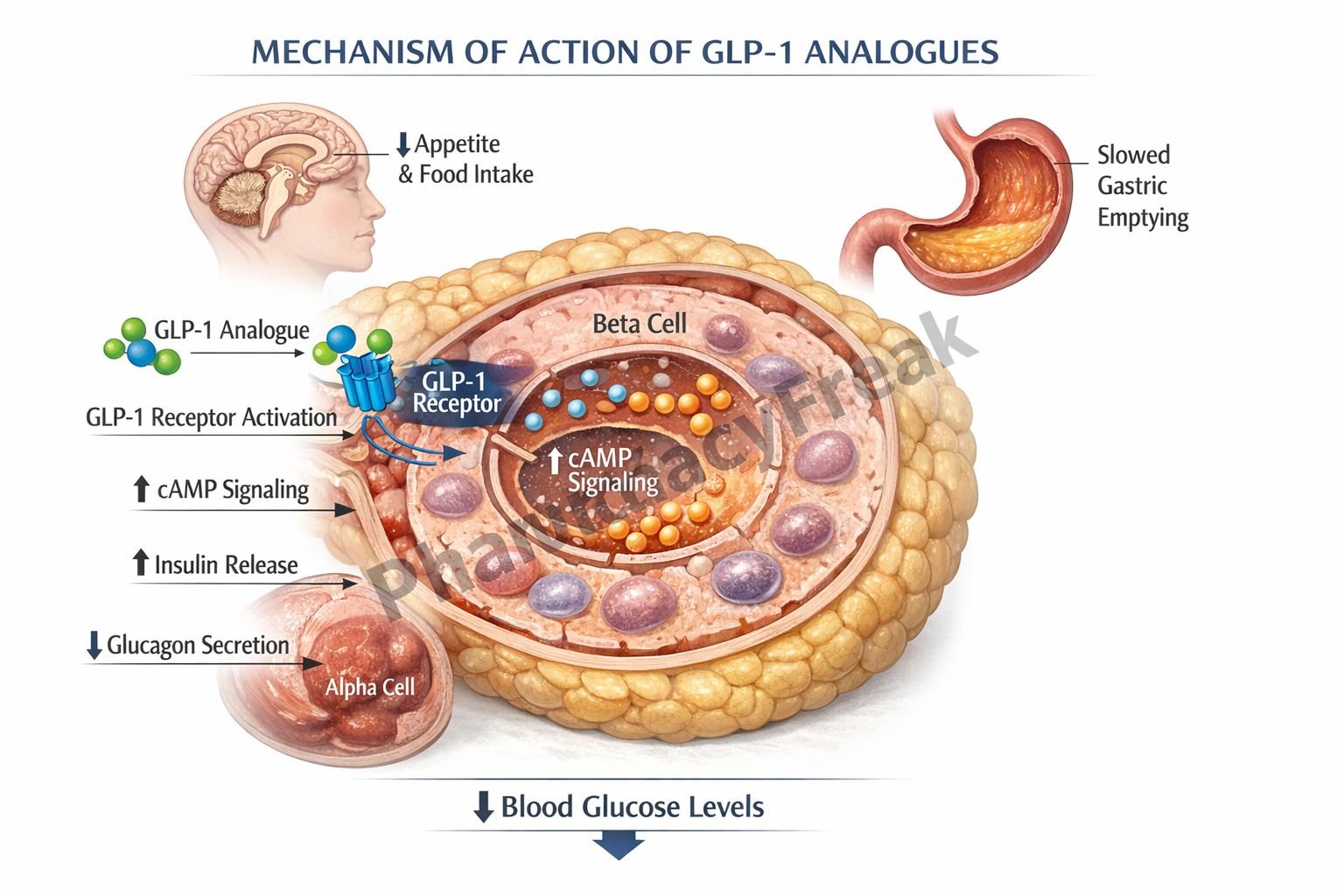
1. Receptors: The Most Common Drug Targets
What Are Receptors?
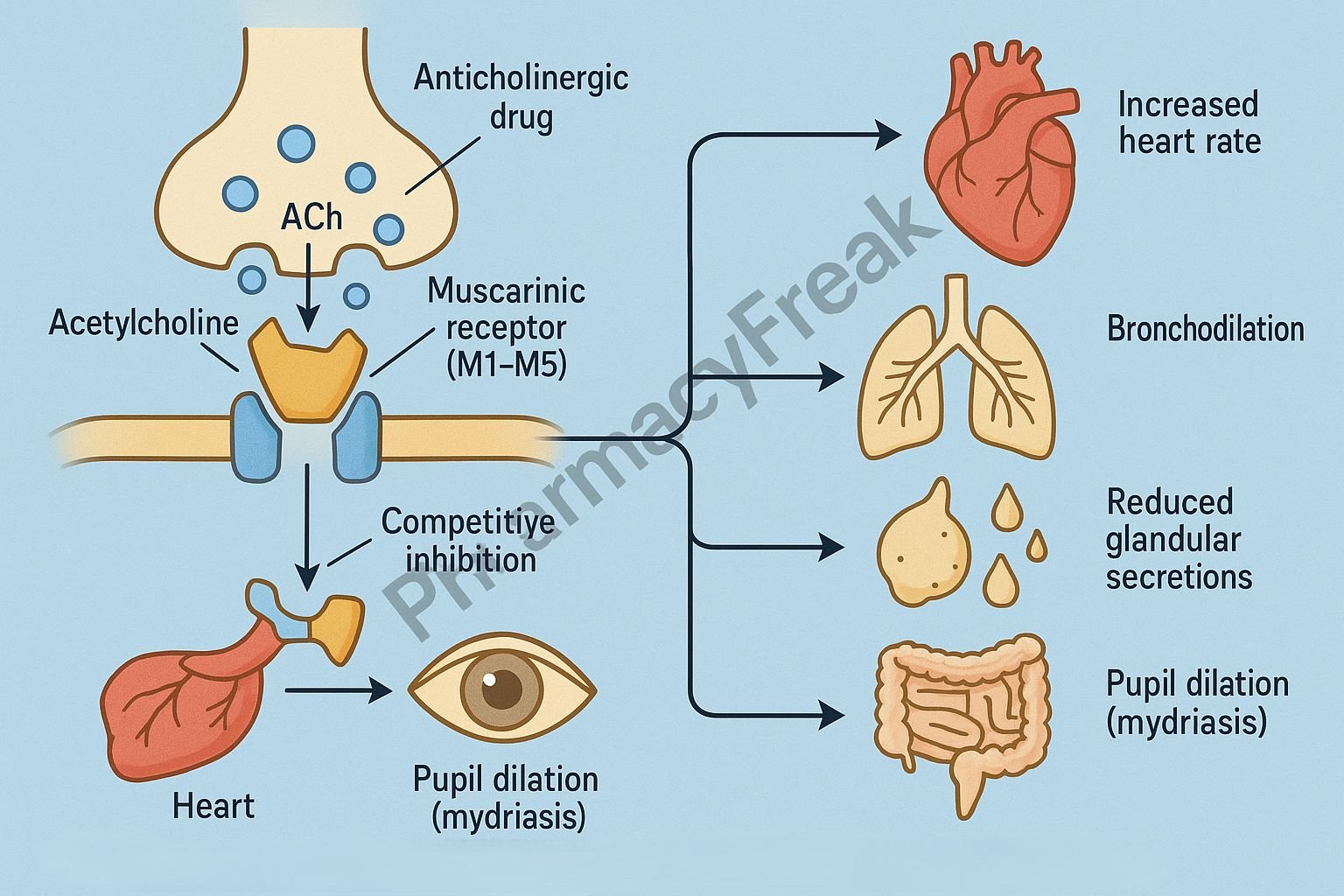
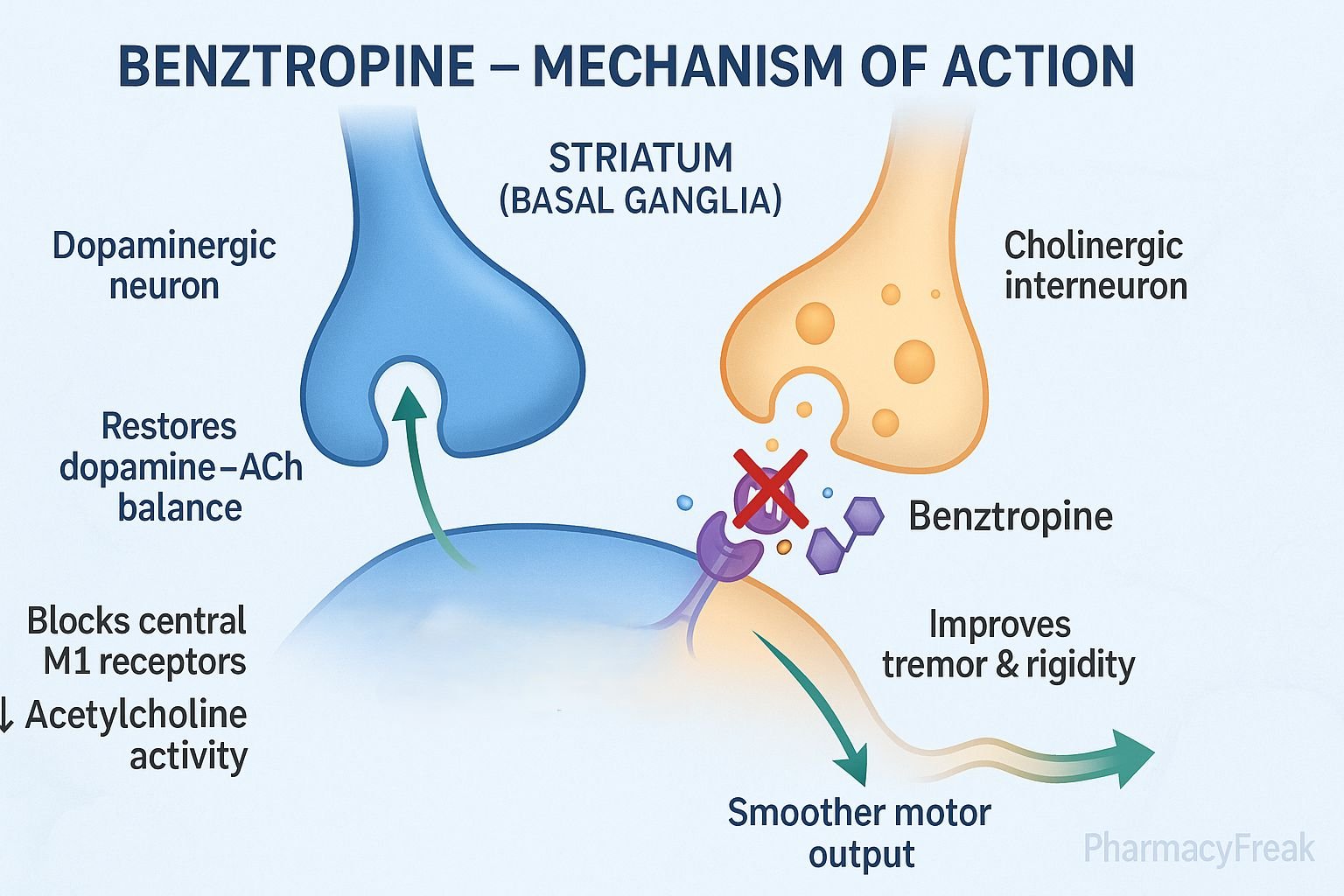
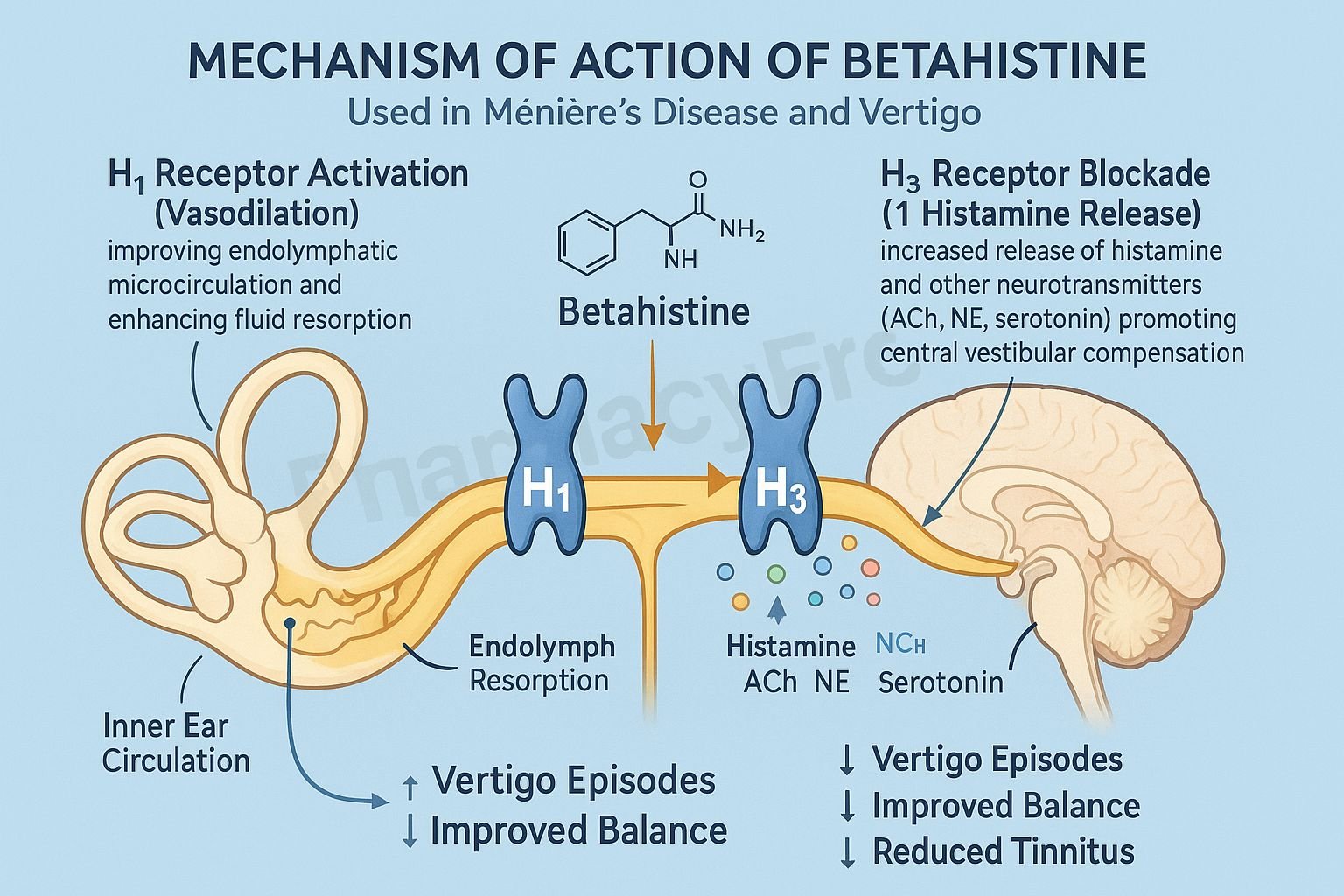
Receptors are protein molecules found on the surface of cells or within cells. They receive signals from endogenous substances like hormones, neurotransmitters, and other signaling molecules.
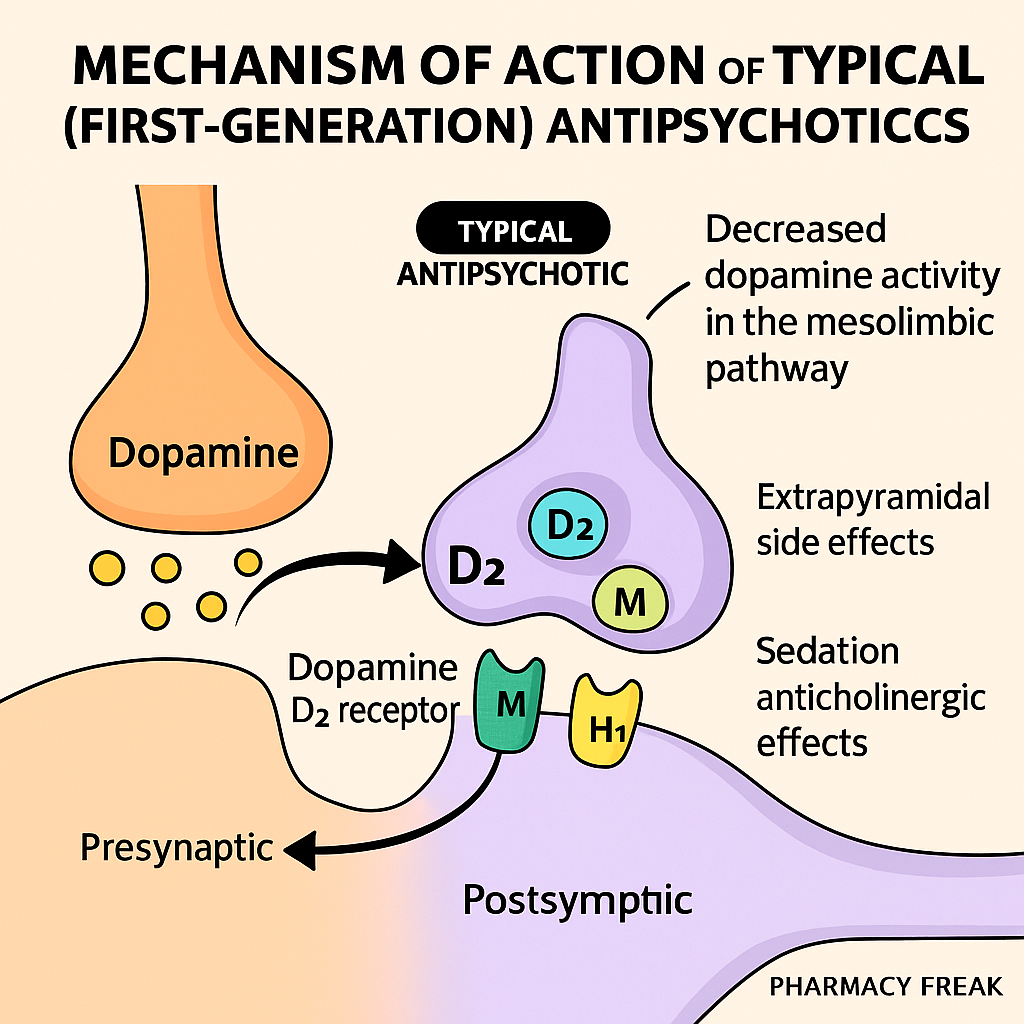
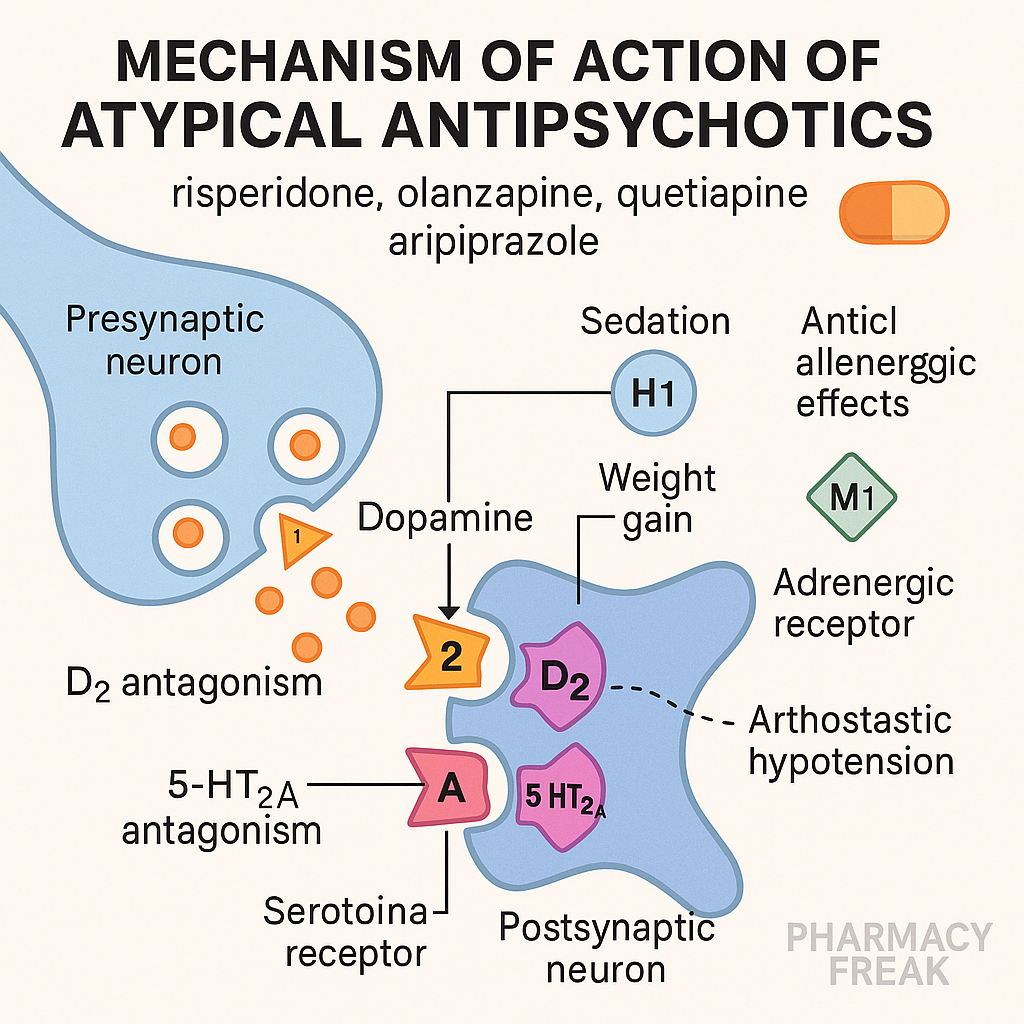
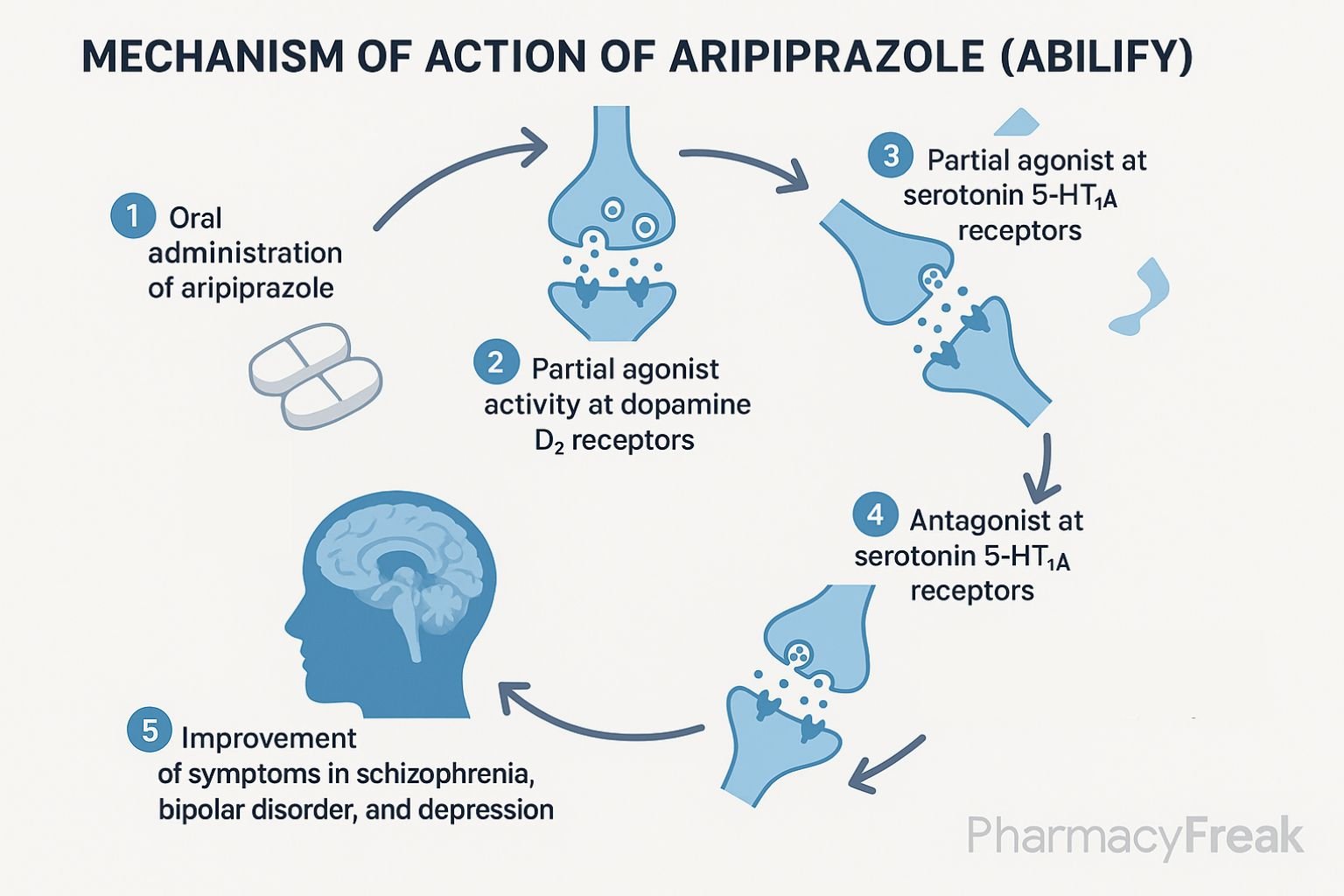
How Drugs Work on Receptors
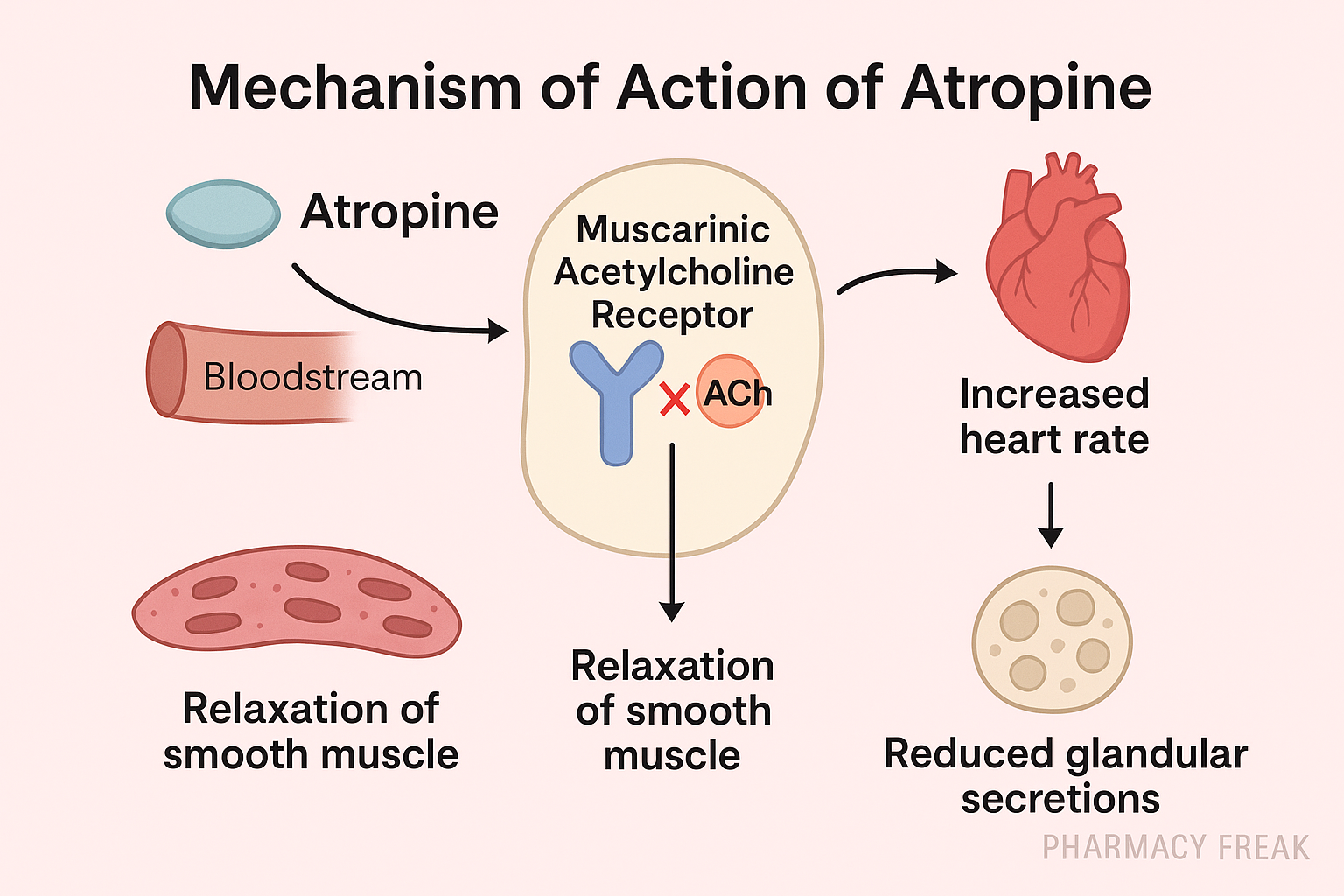
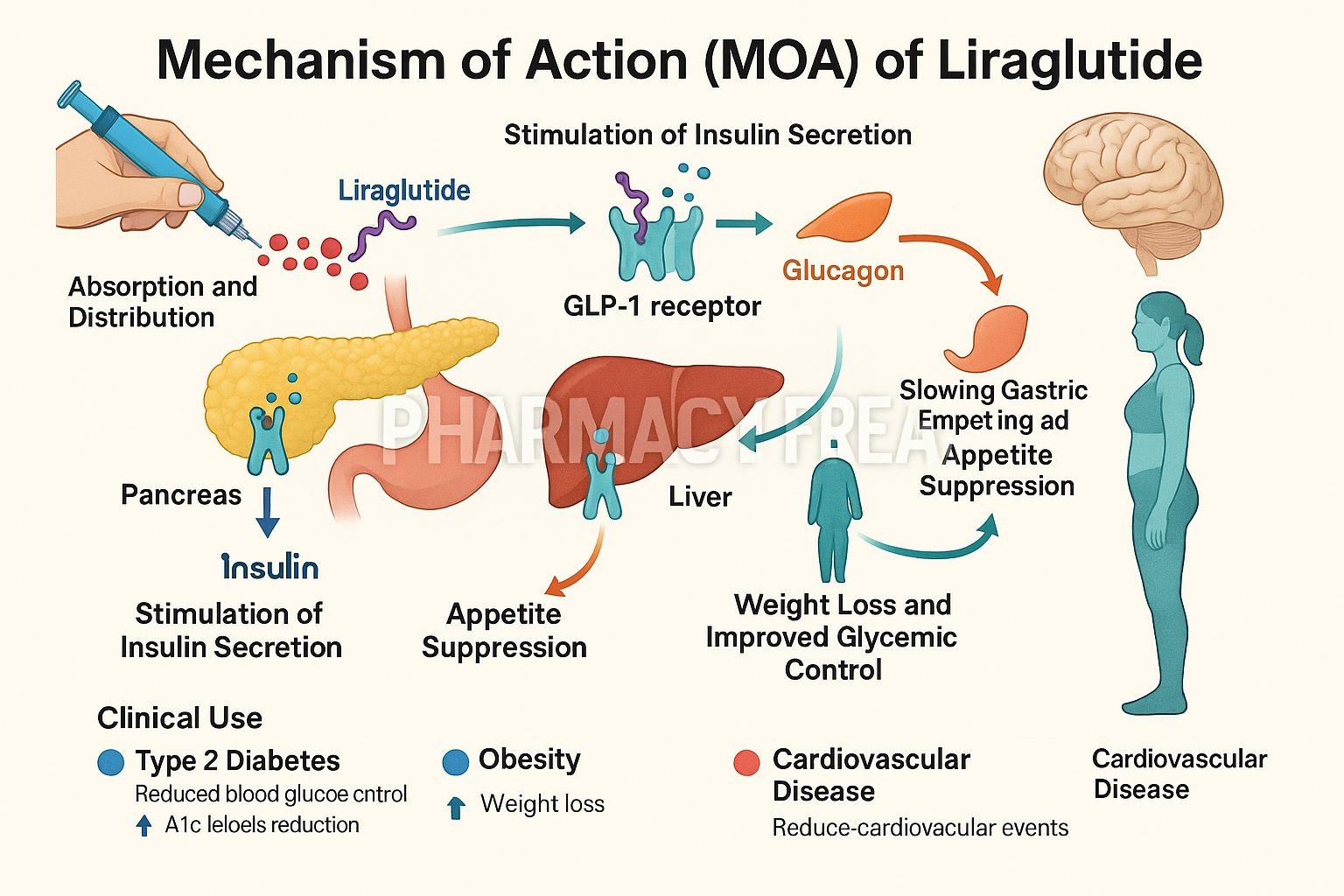
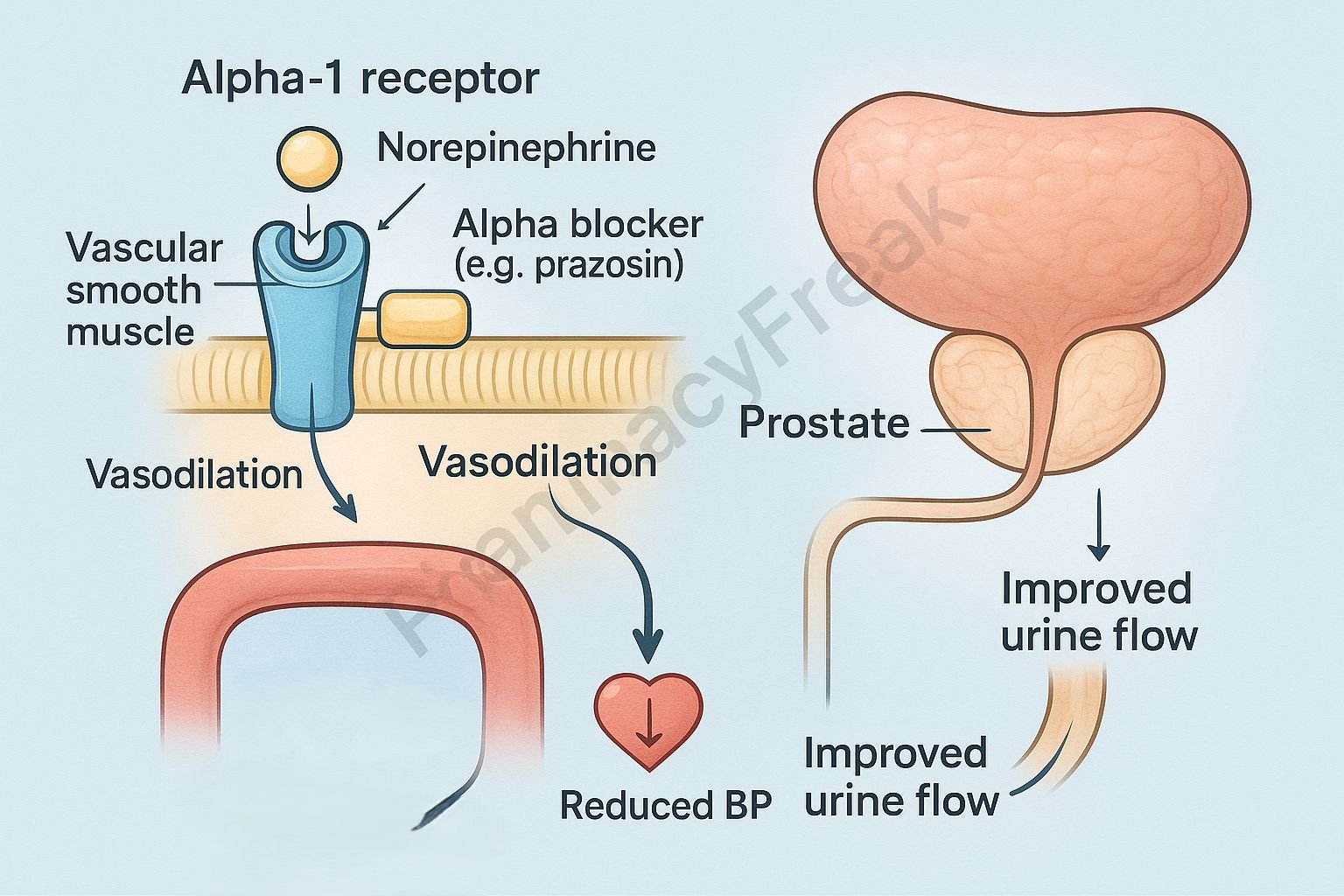
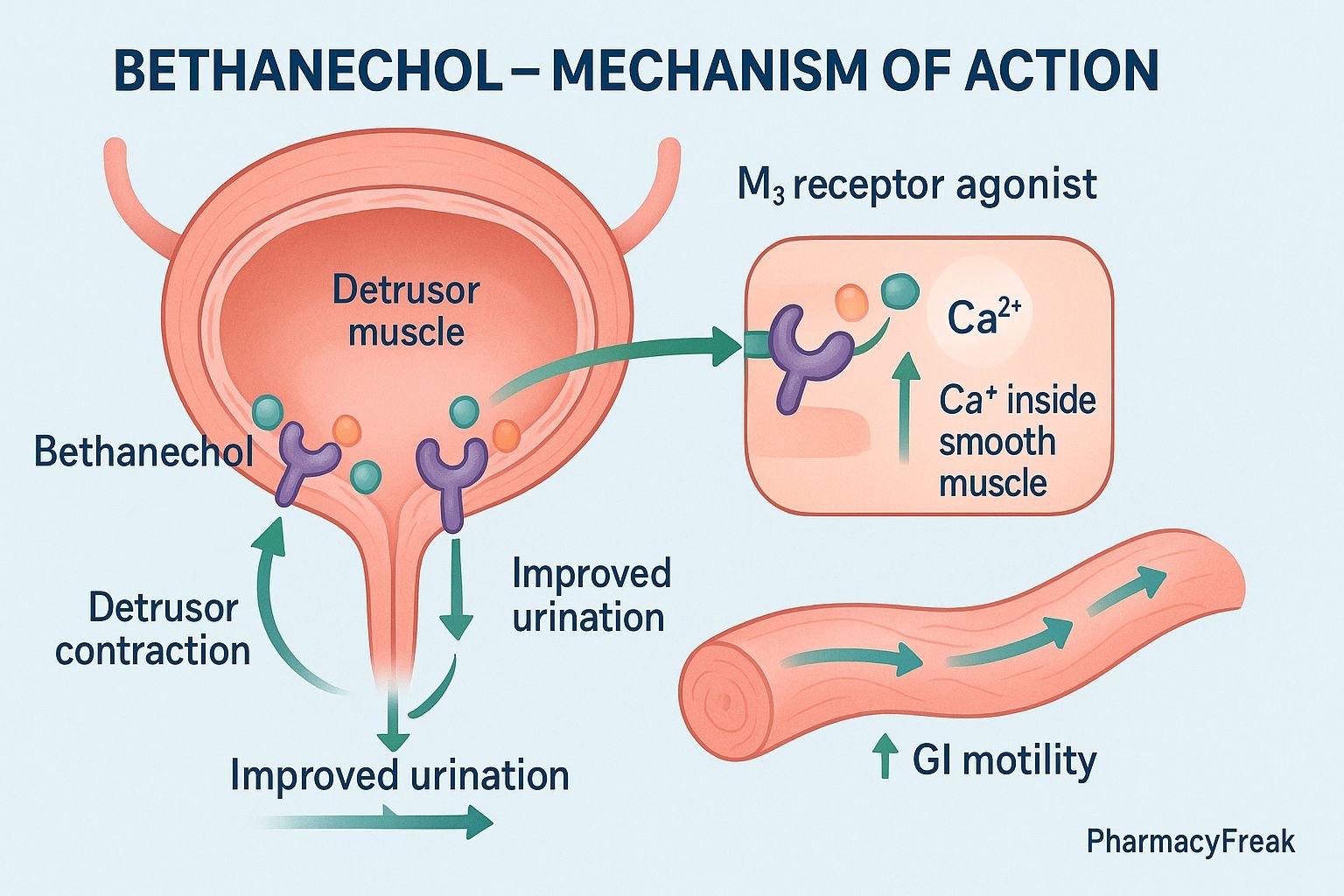
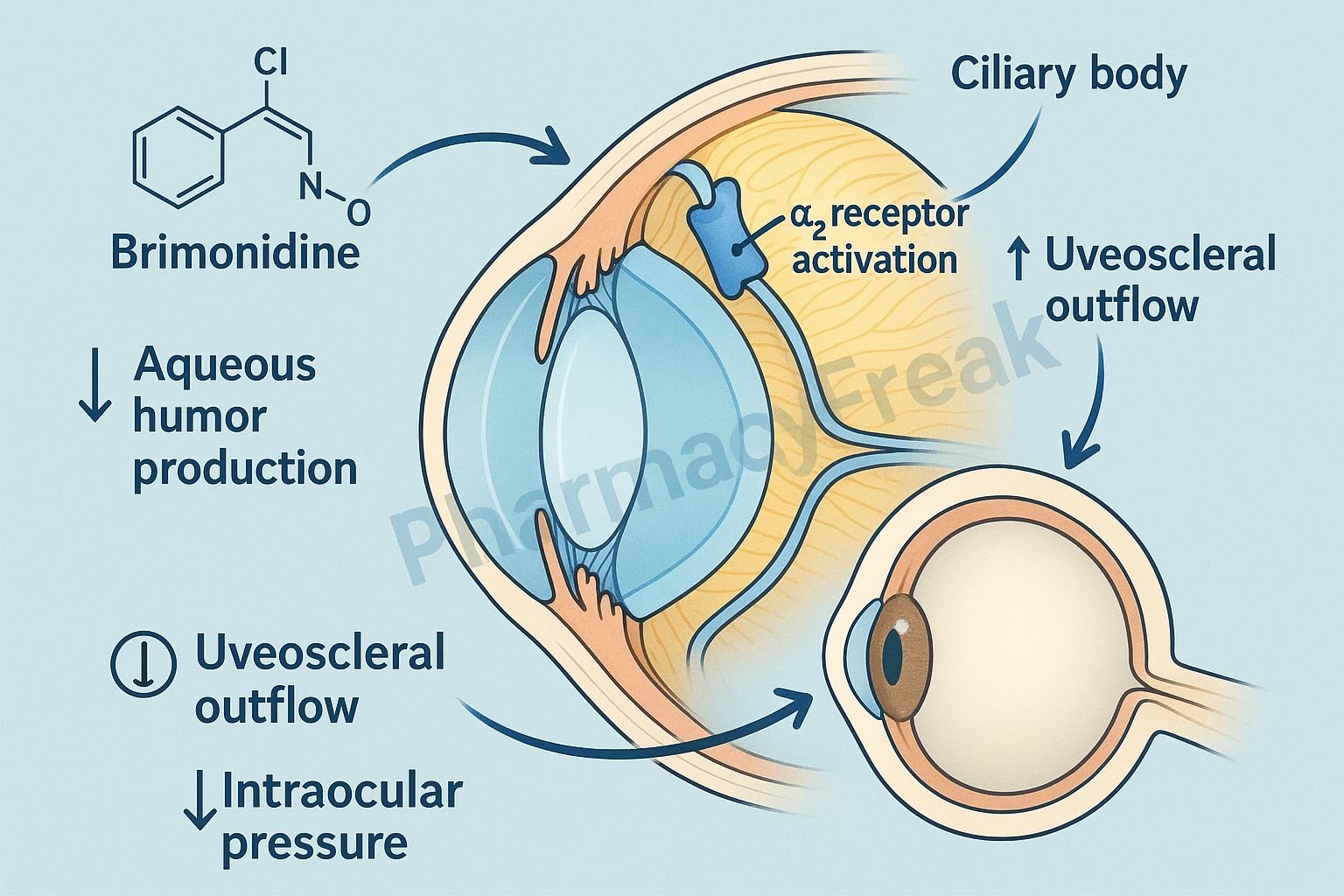
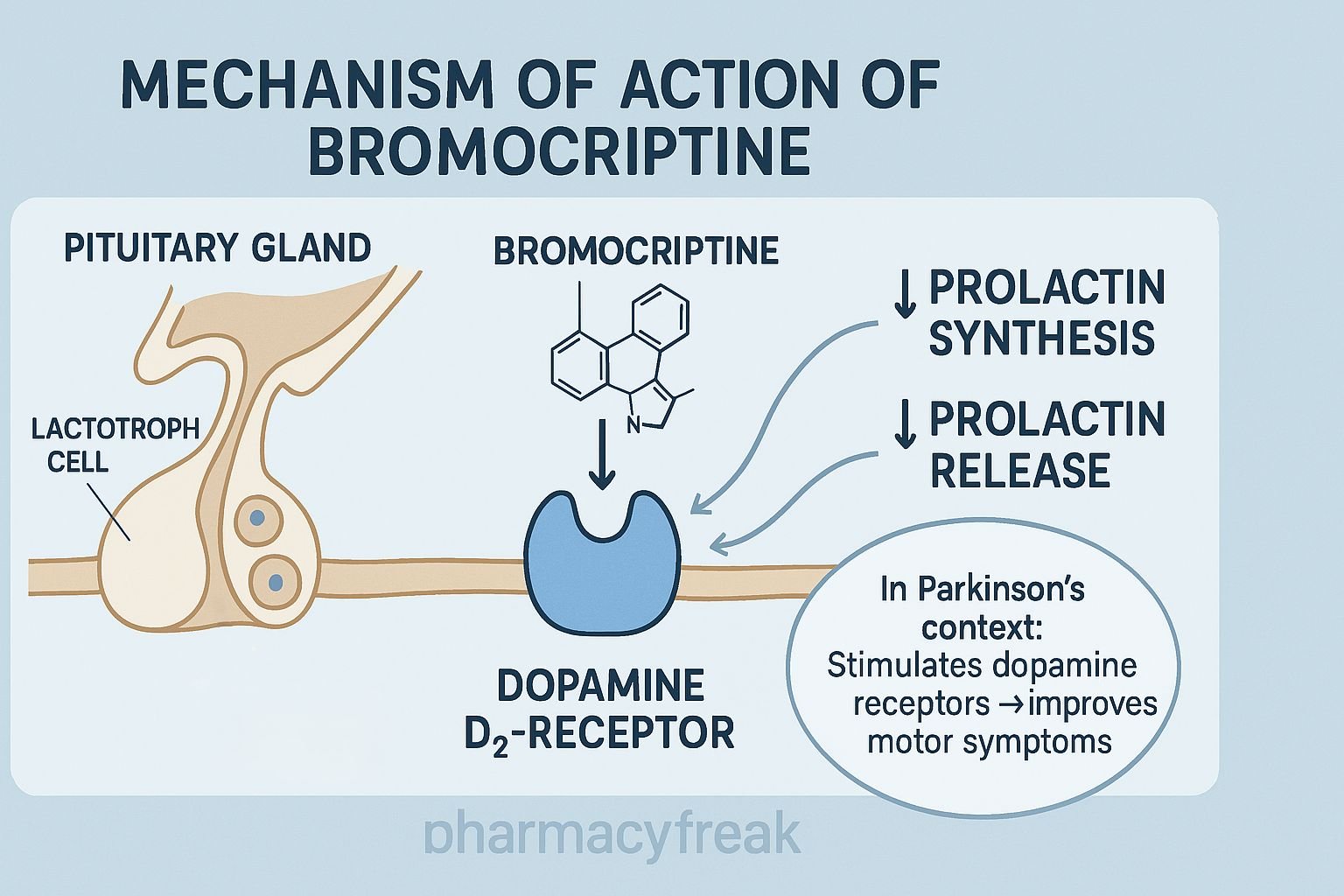
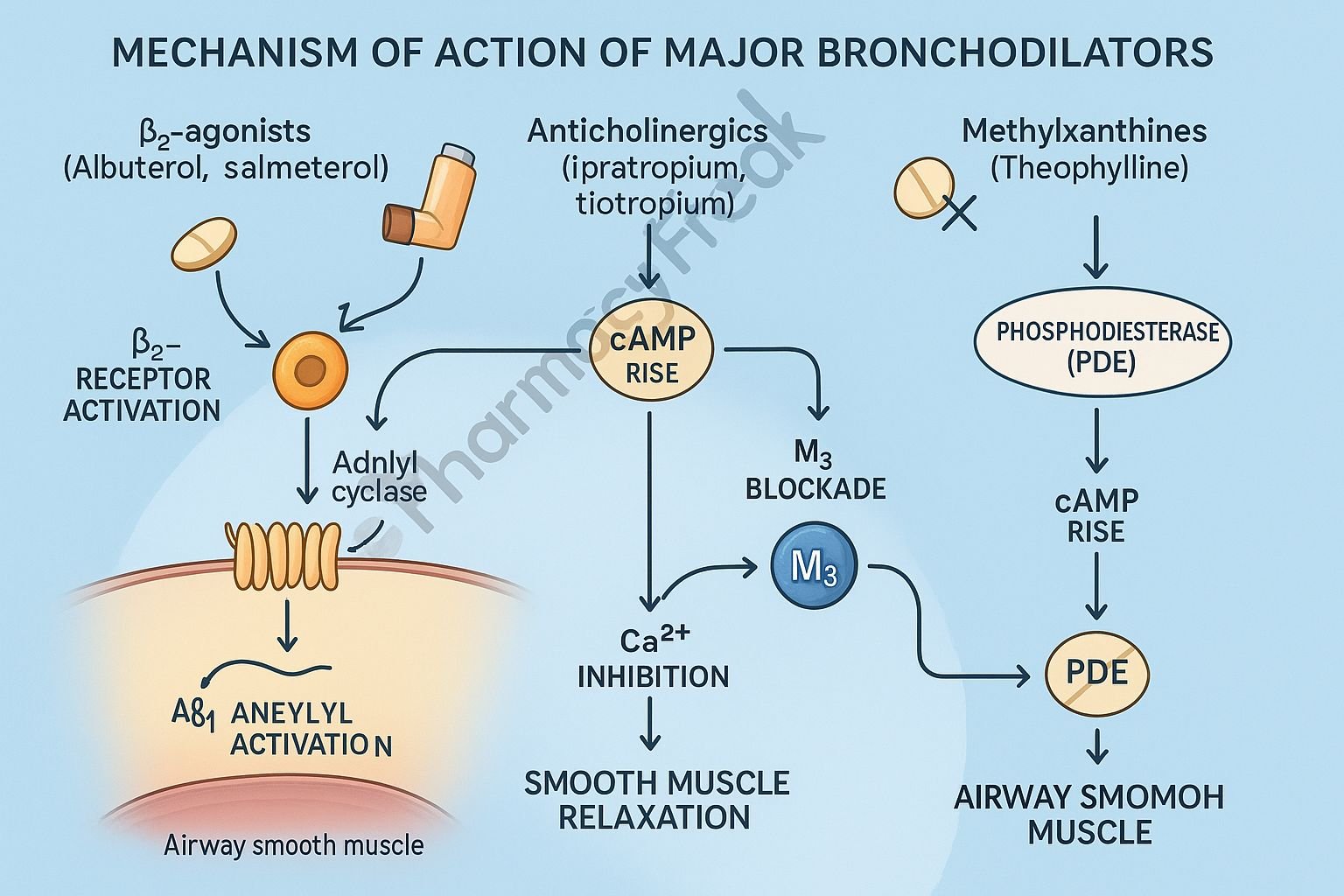
Agonists: Drugs that bind to receptors and mimic the action of the natural ligand, activating the receptor.
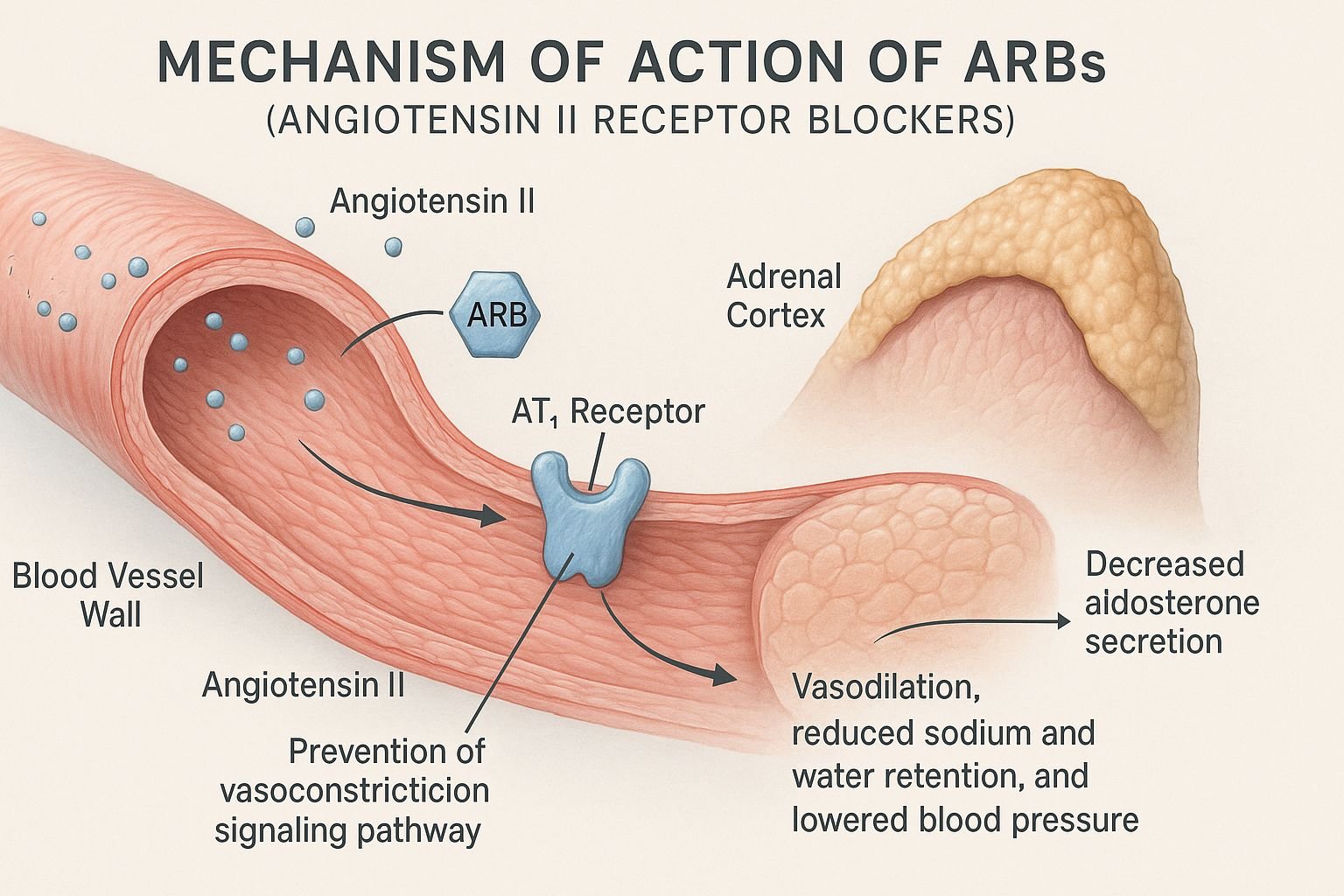
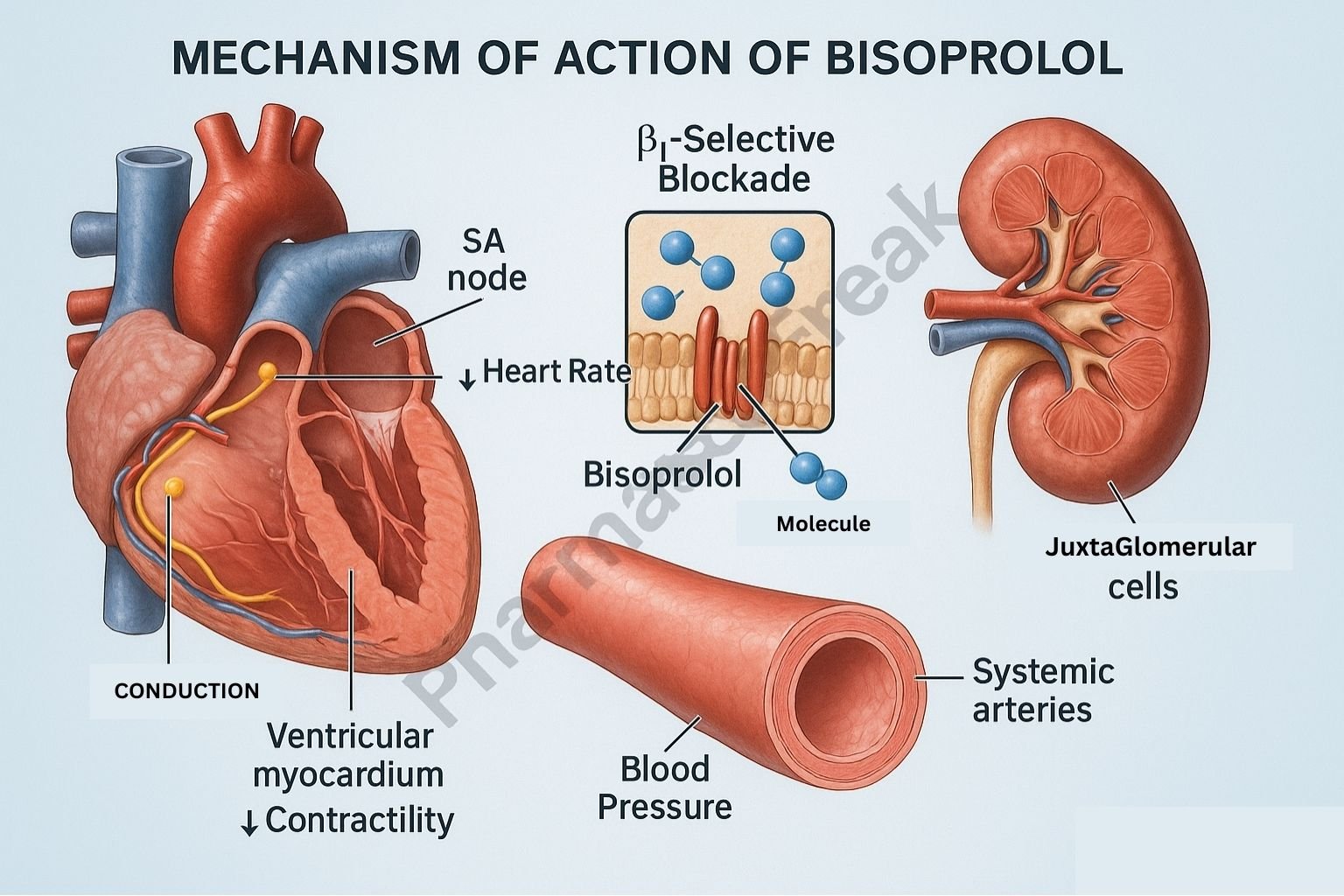
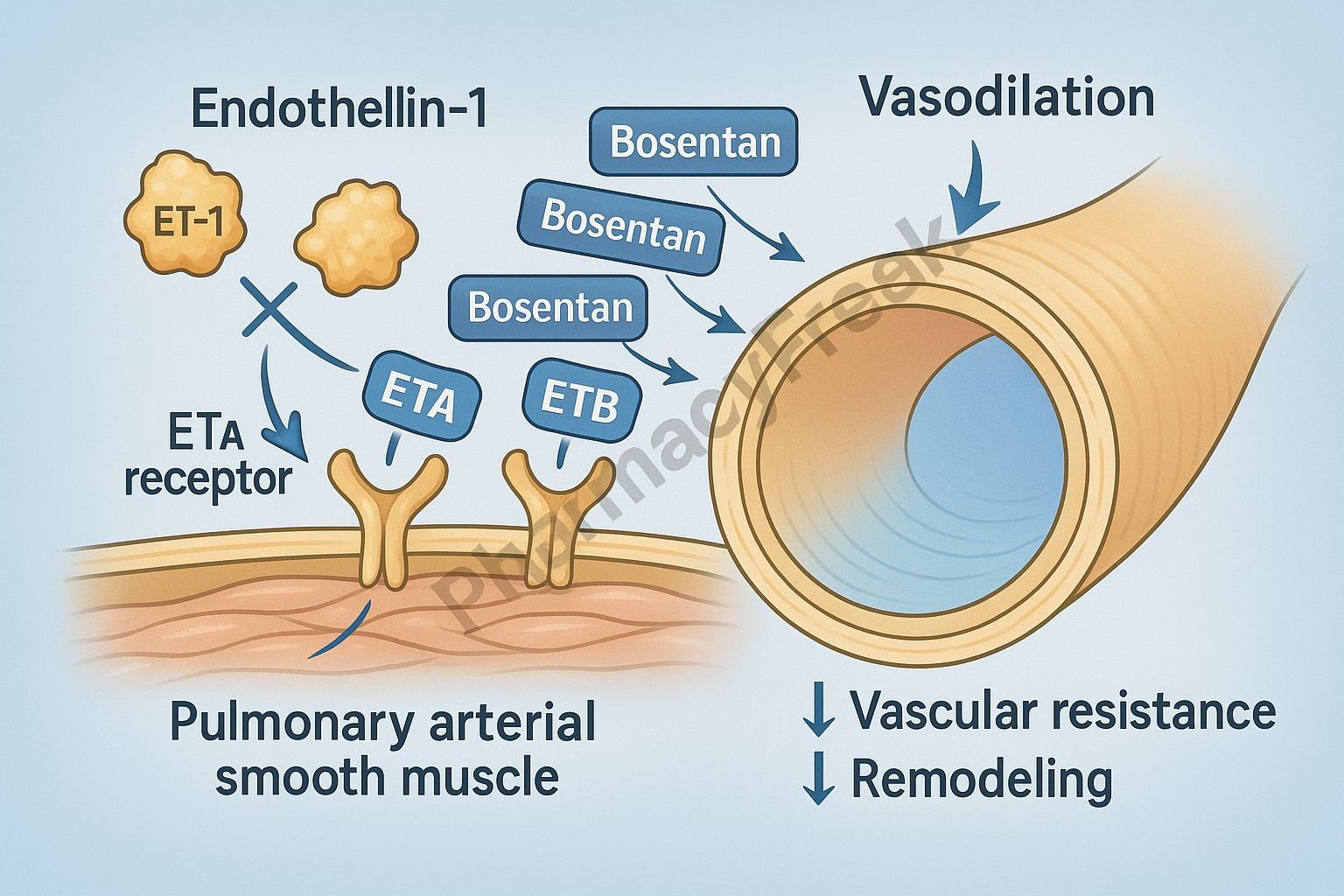
Antagonists: Drugs that bind to receptors but do not activate them. Instead, they block the natural ligand from binding.
Partial Agonists: These activate receptors but produce a weaker response than full agonists.
Inverse Agonists: These produce the opposite effect of agonists by stabilizing receptors in their inactive state.
Examples
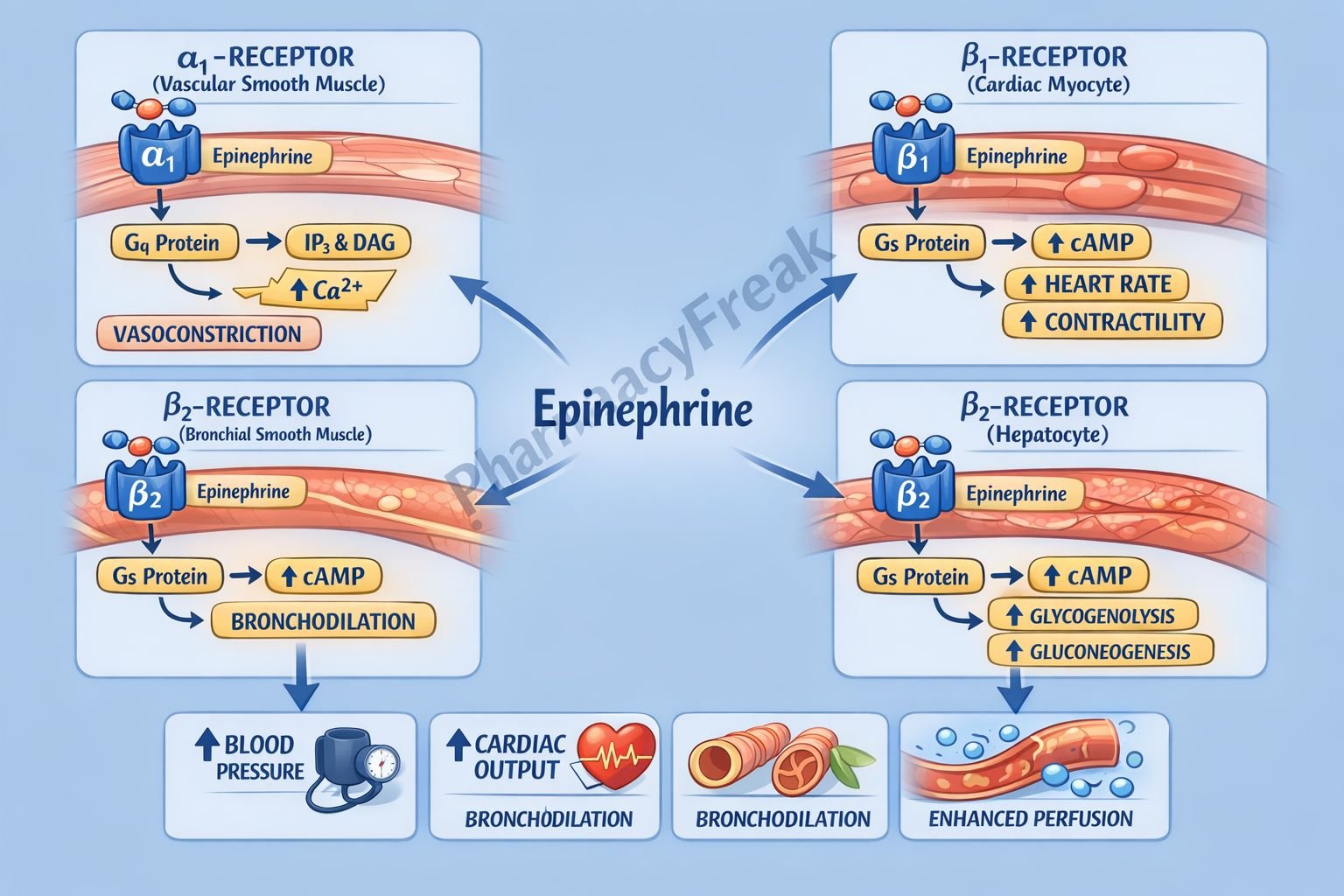
Beta-adrenergic agonists (e.g., salbutamol): Used in asthma to relax airway muscles by stimulating beta-2 receptors.
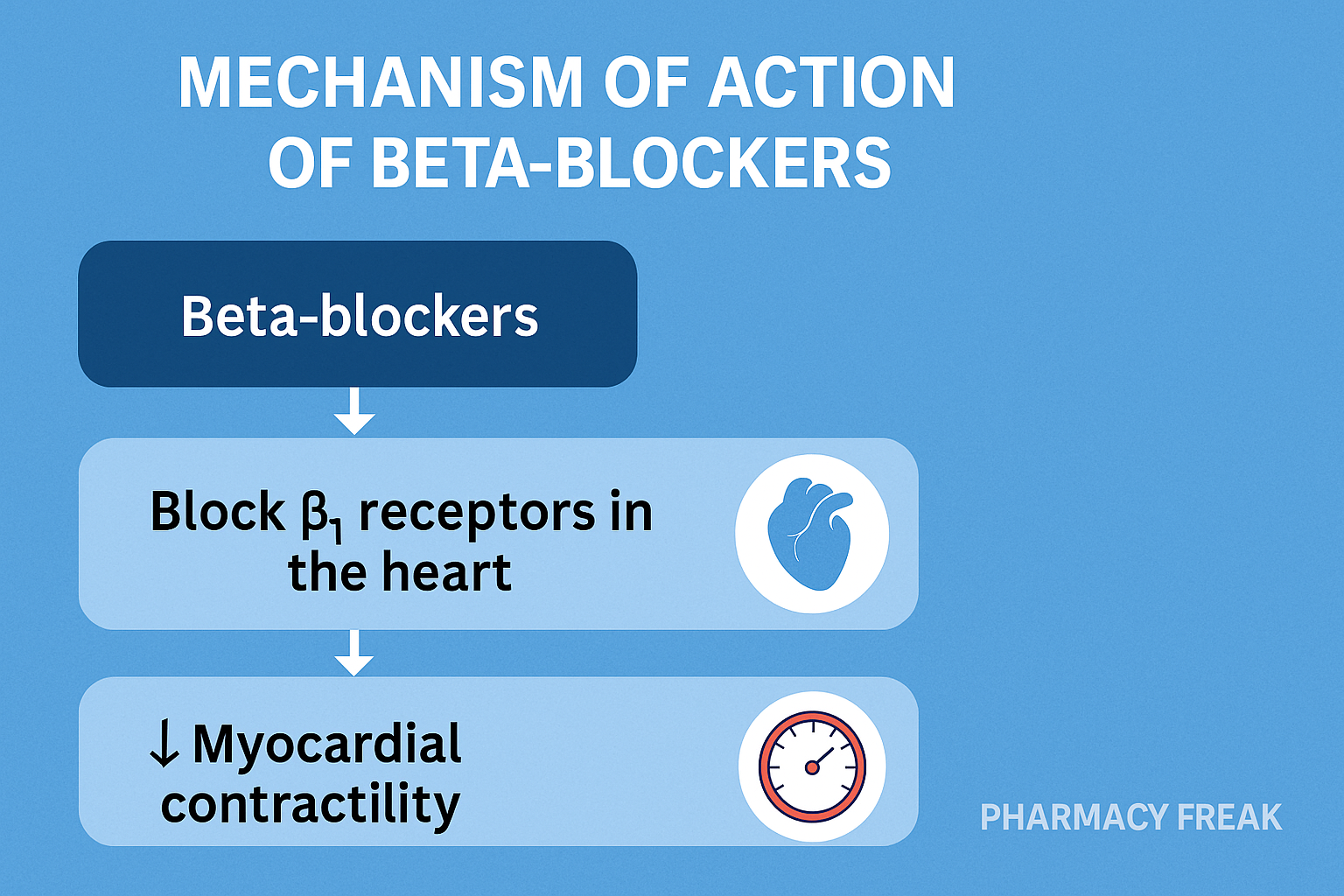
Beta-blockers (e.g., propranolol): Used in hypertension to block beta receptors, slowing the heart rate and reducing blood pressure.
Opioid agonists (e.g., morphine): Bind to opioid receptors in the central nervous system to relieve pain.
Clinical Relevance
Receptor-based drug action explains the selectivity and potency of many medications. Knowing receptor types and locations can help predict therapeutic and adverse effects.
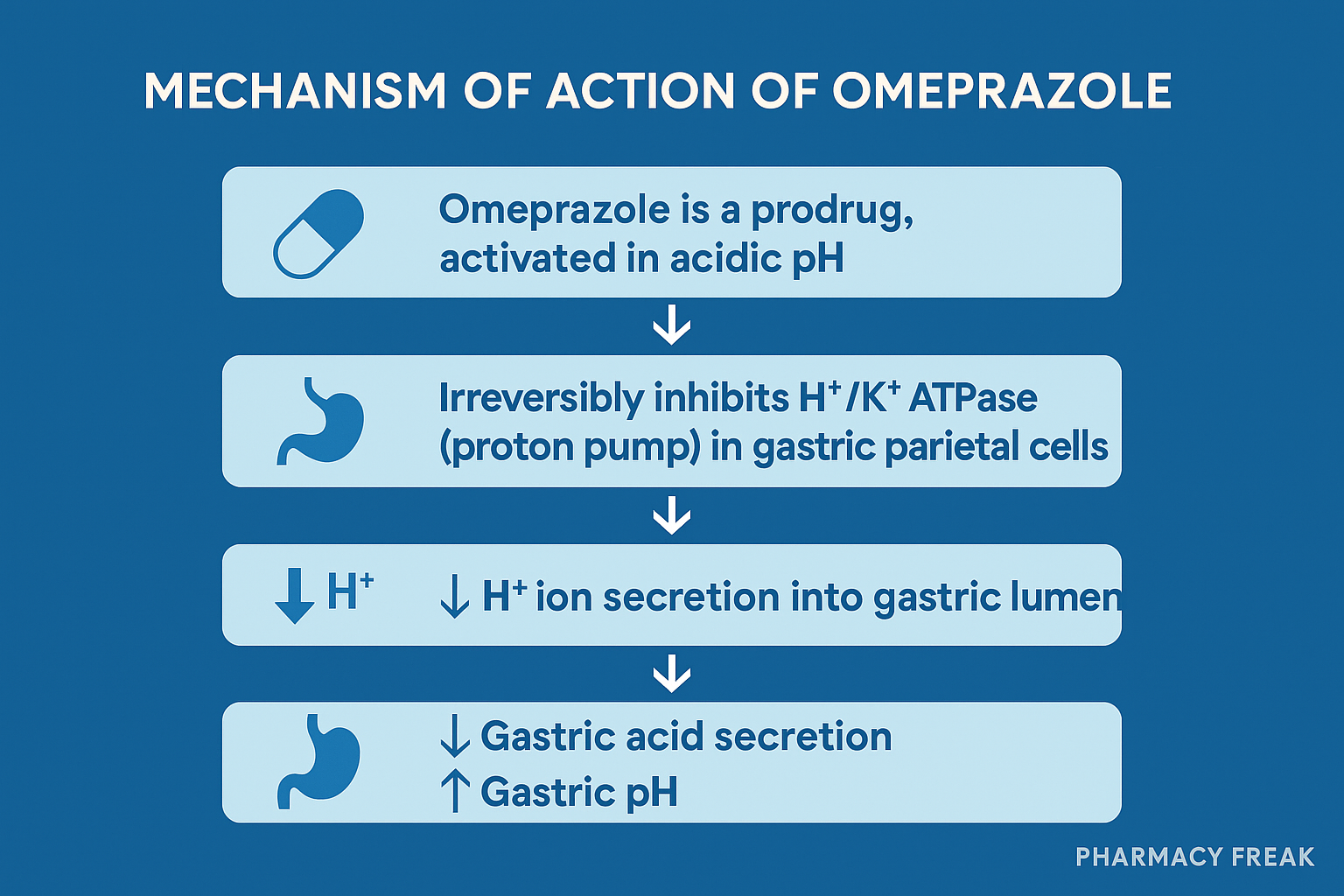
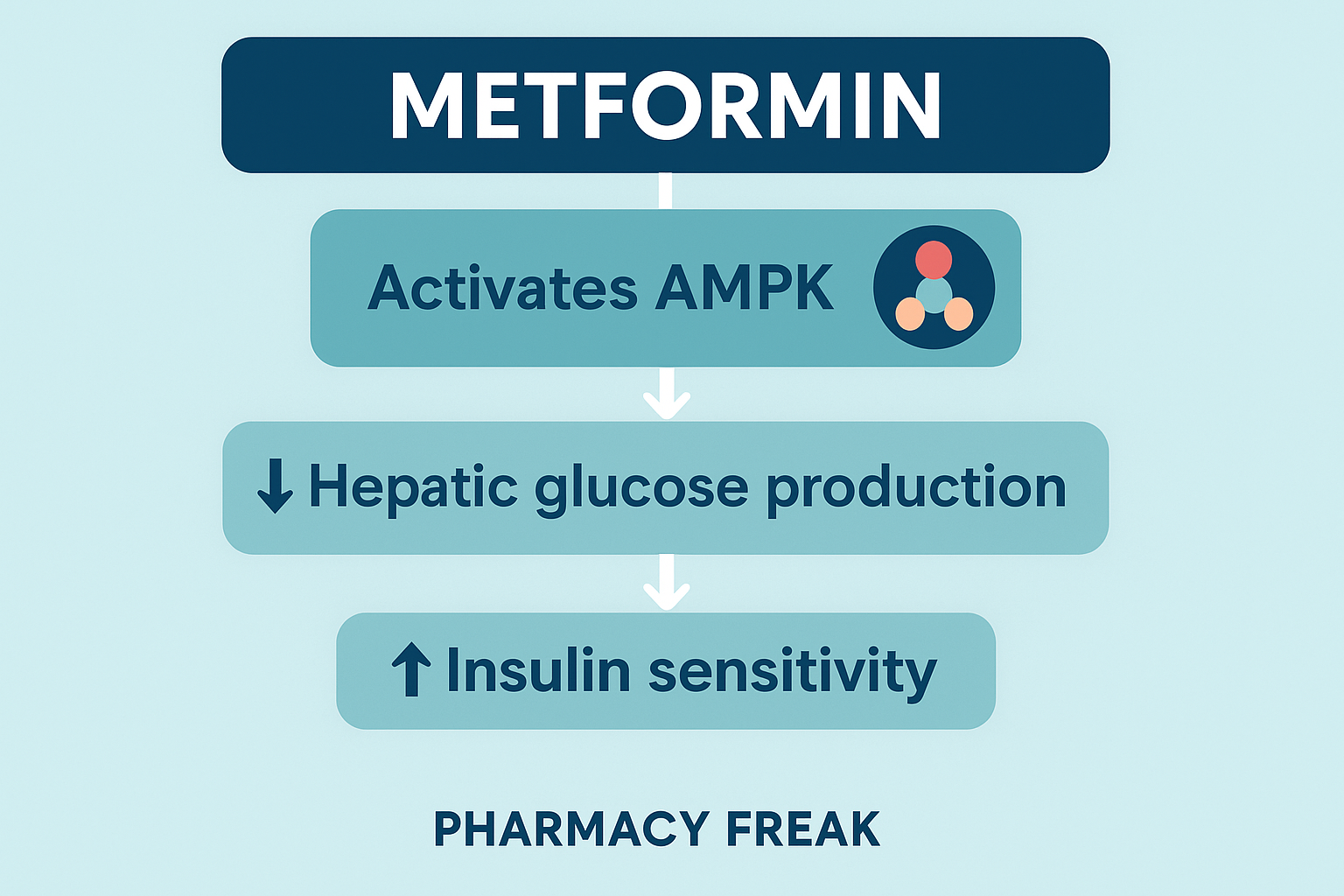
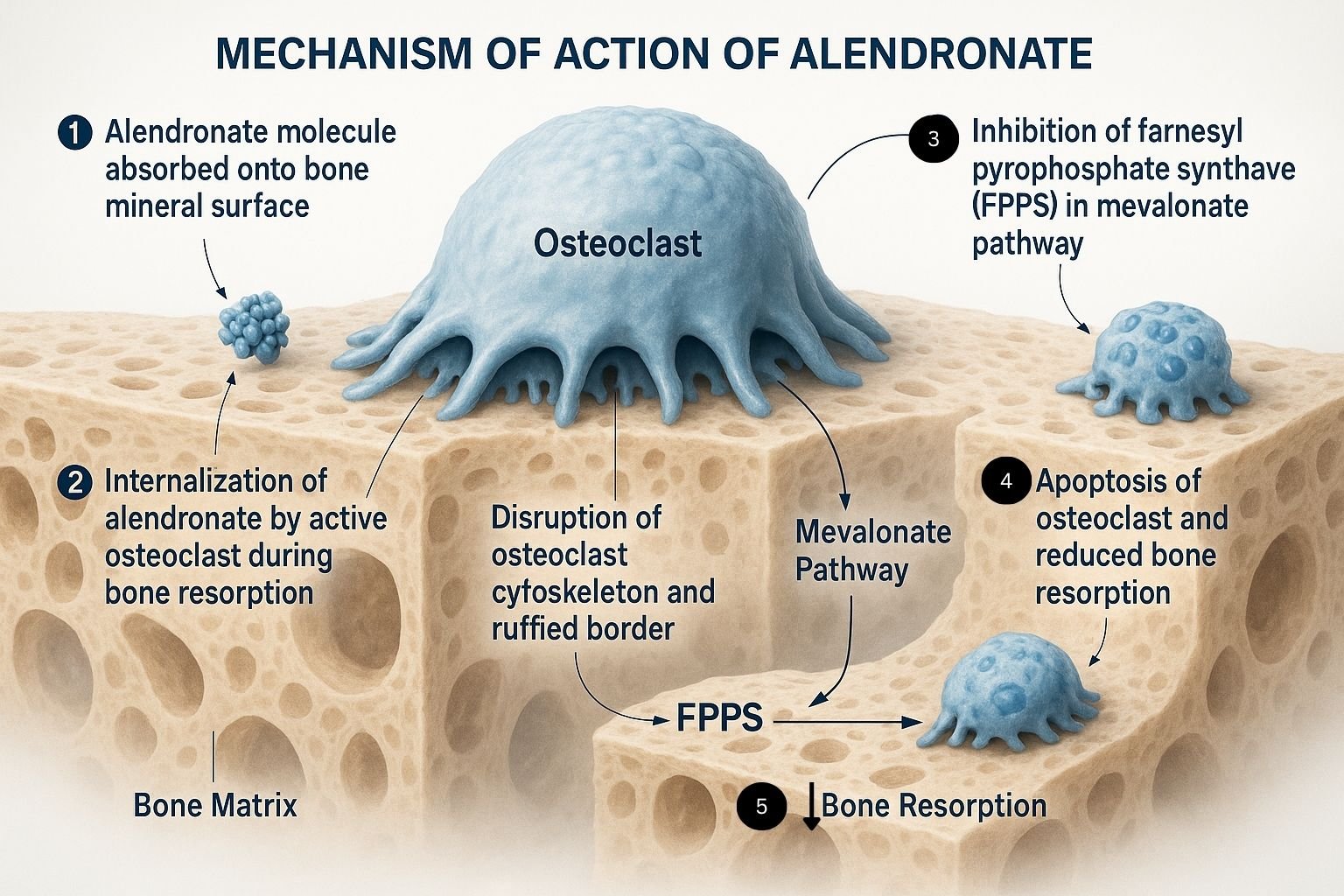
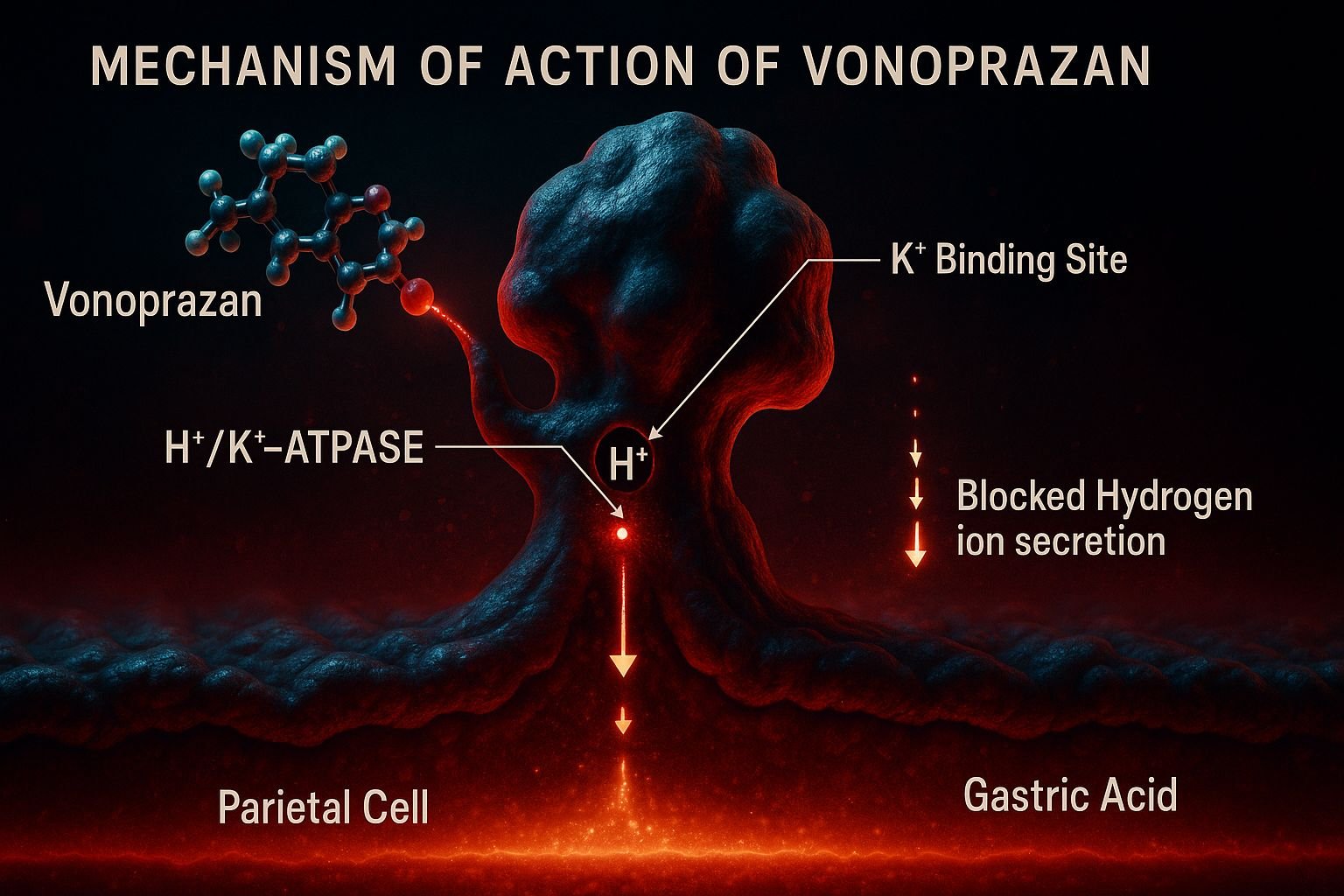
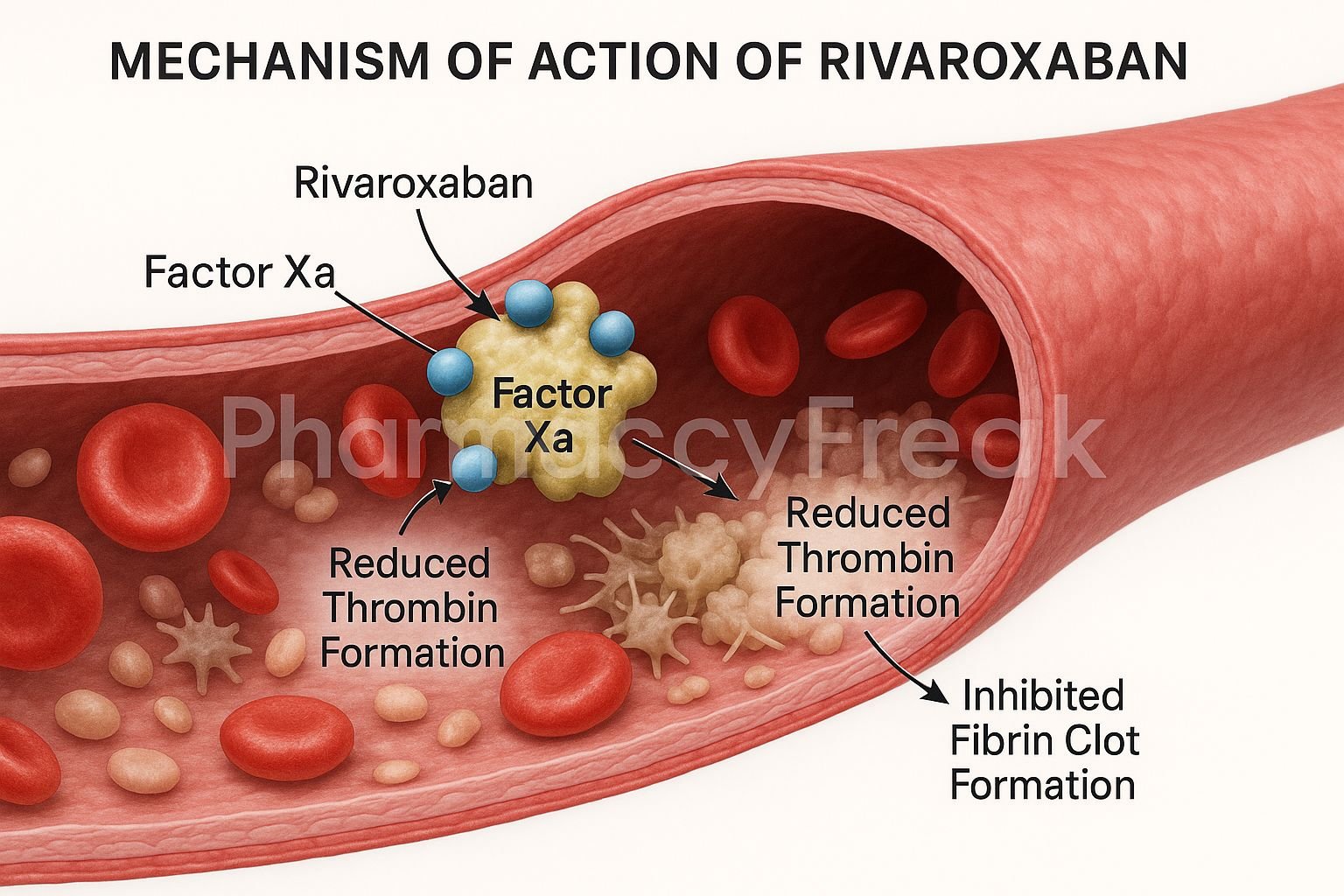
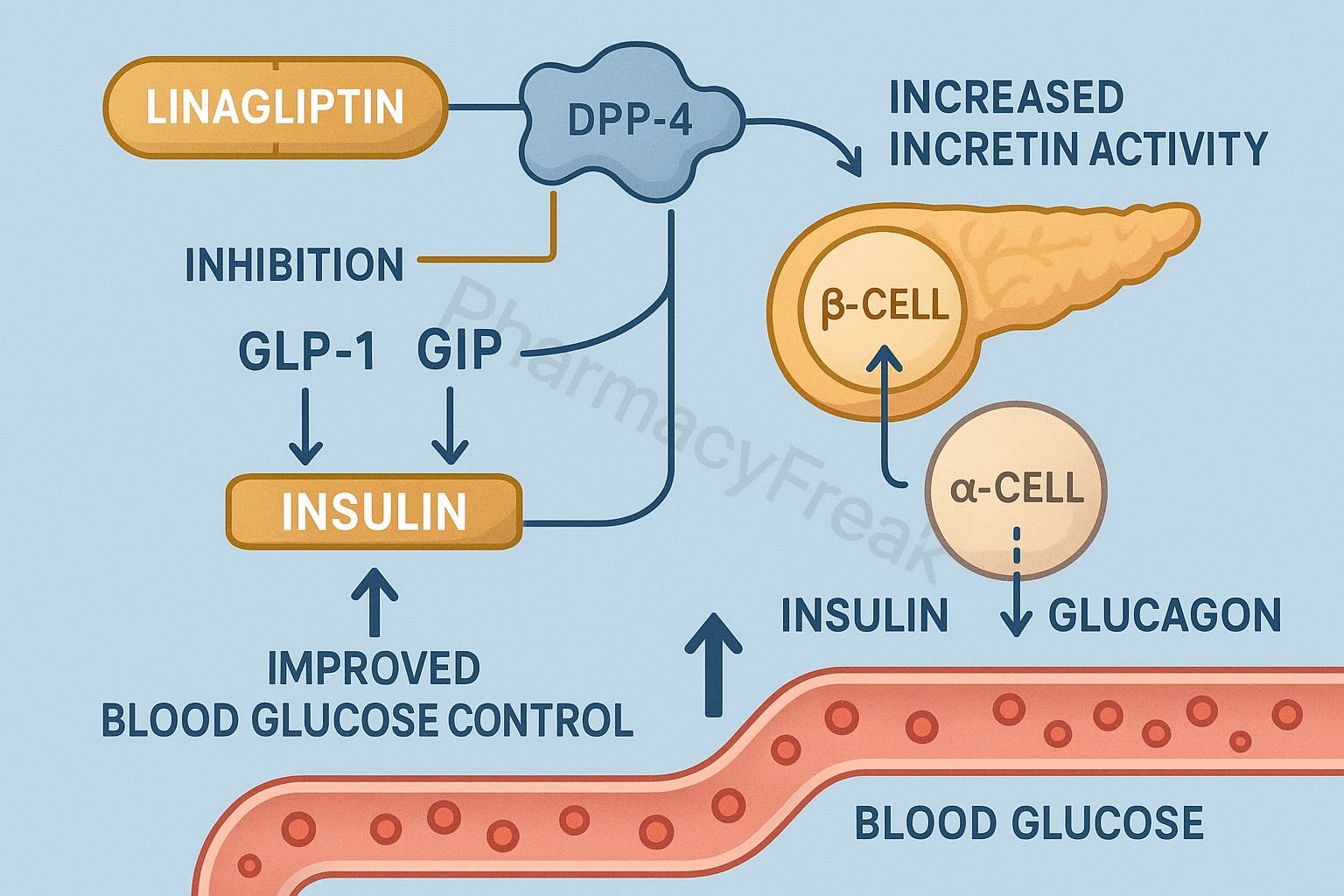
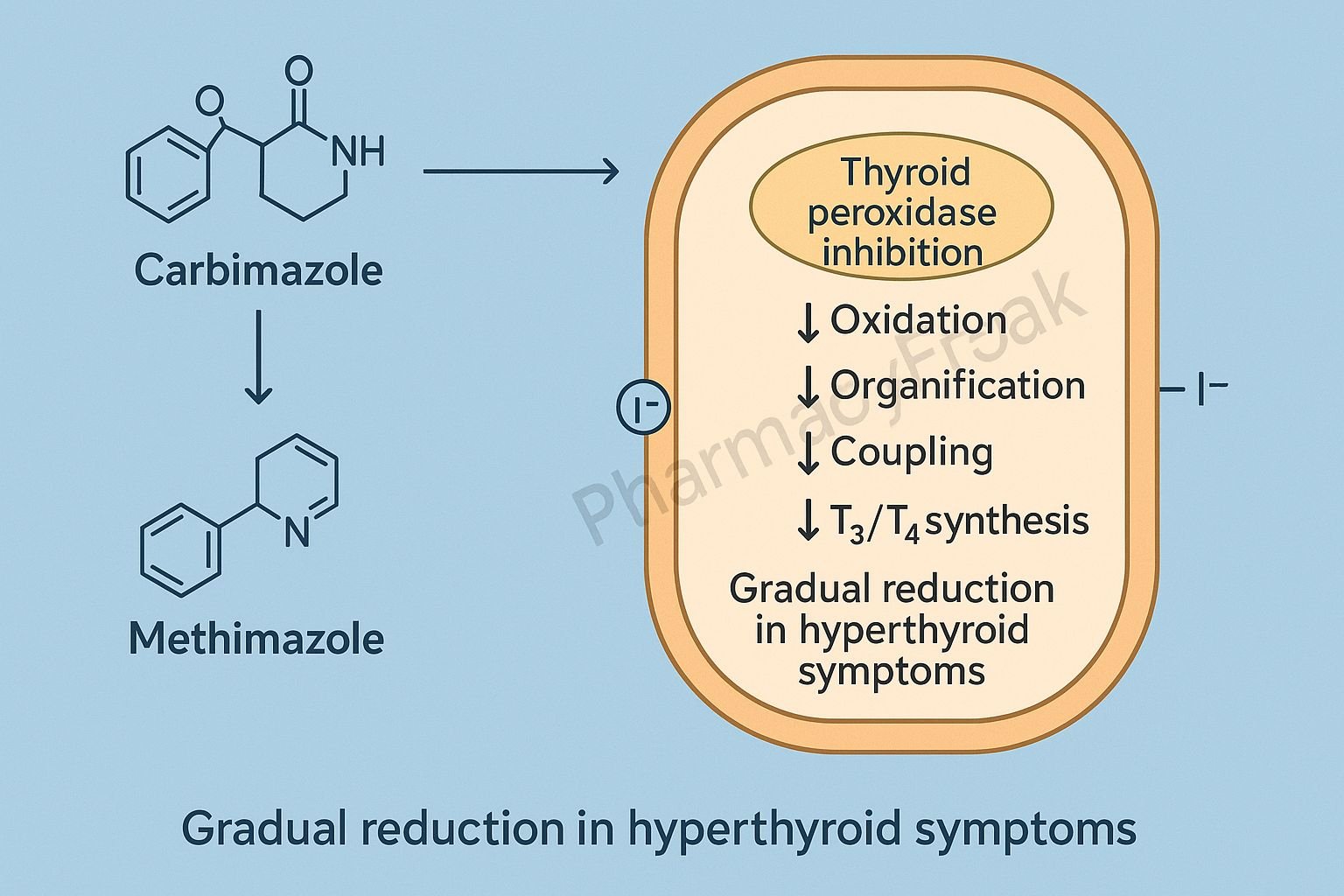
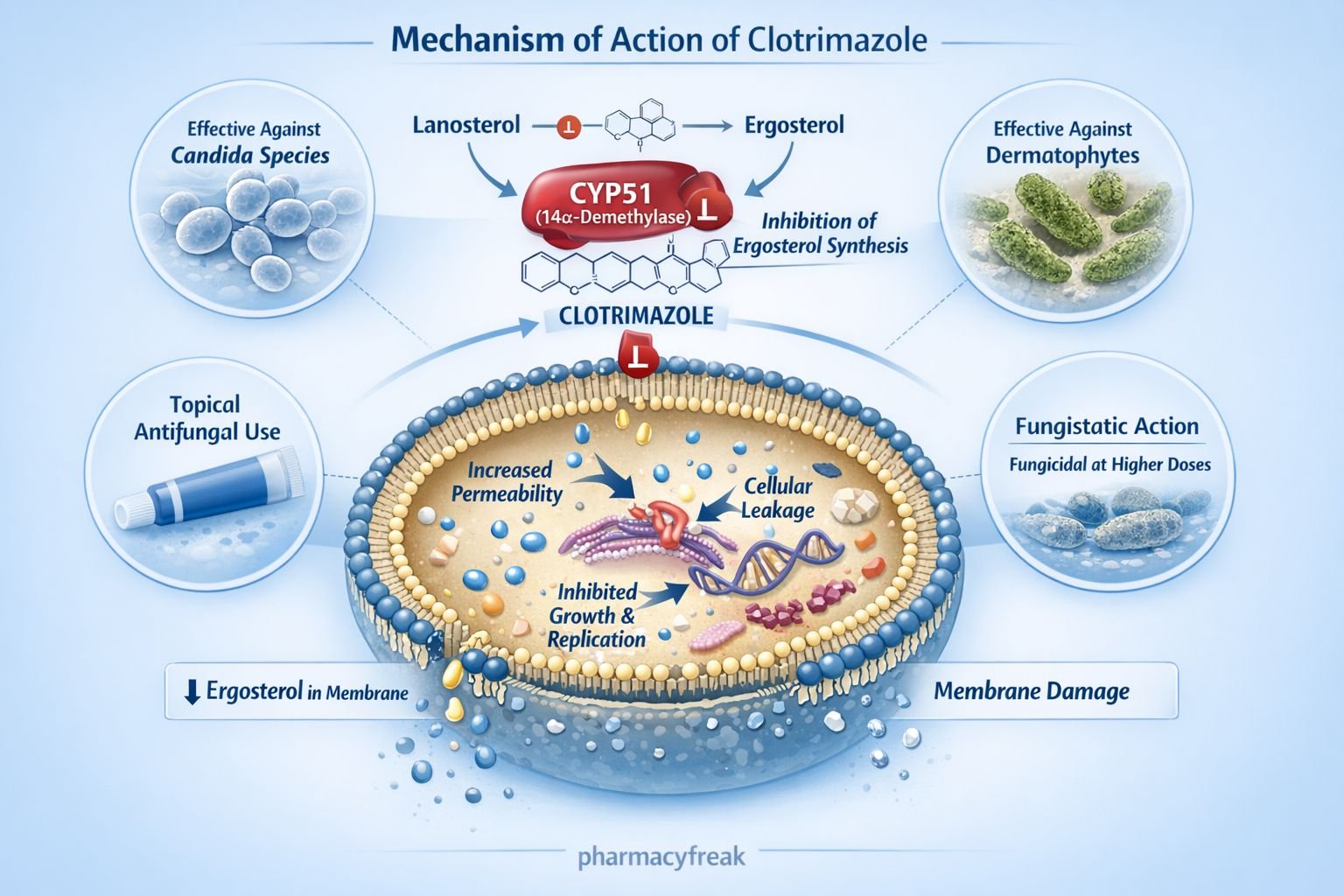
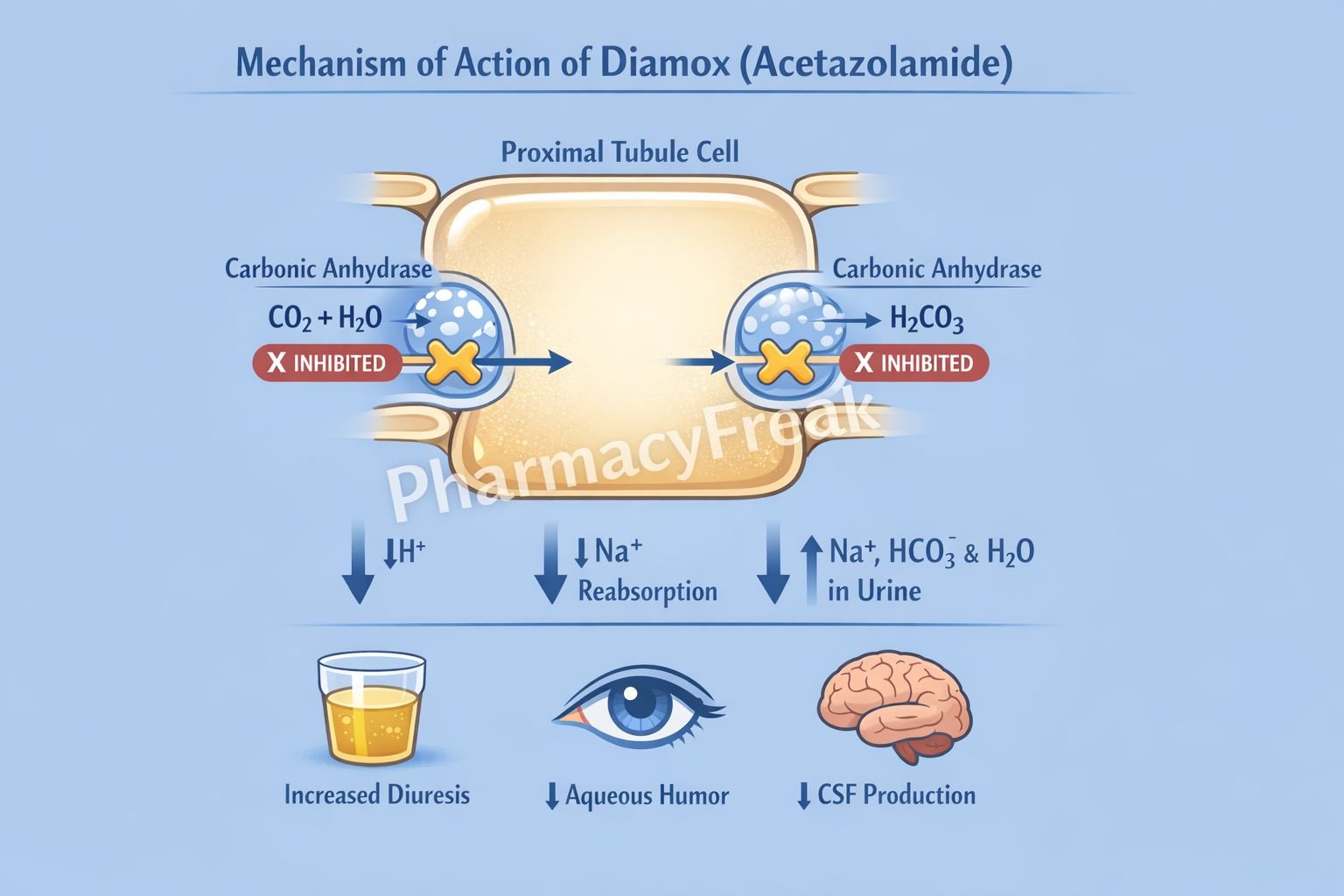
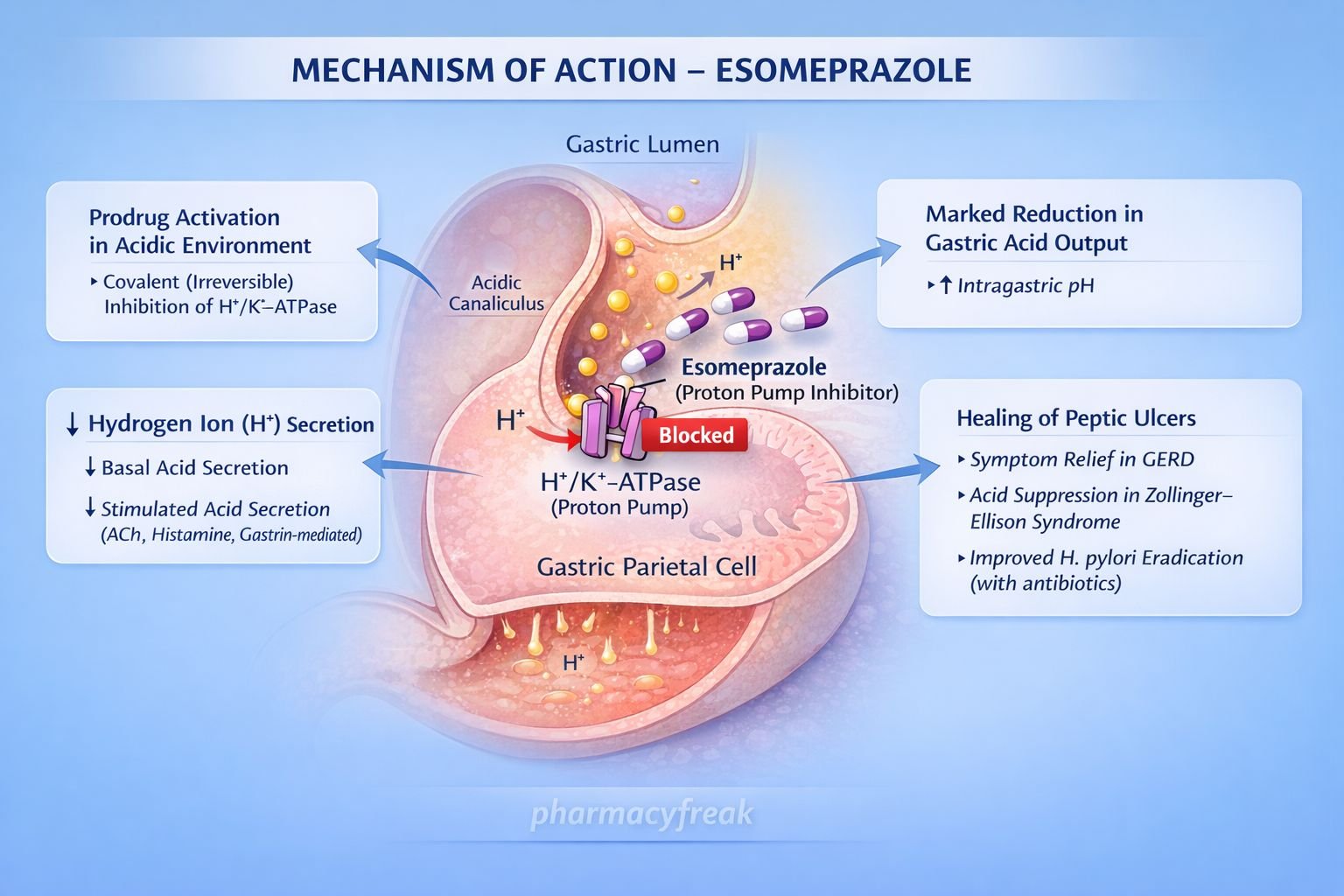
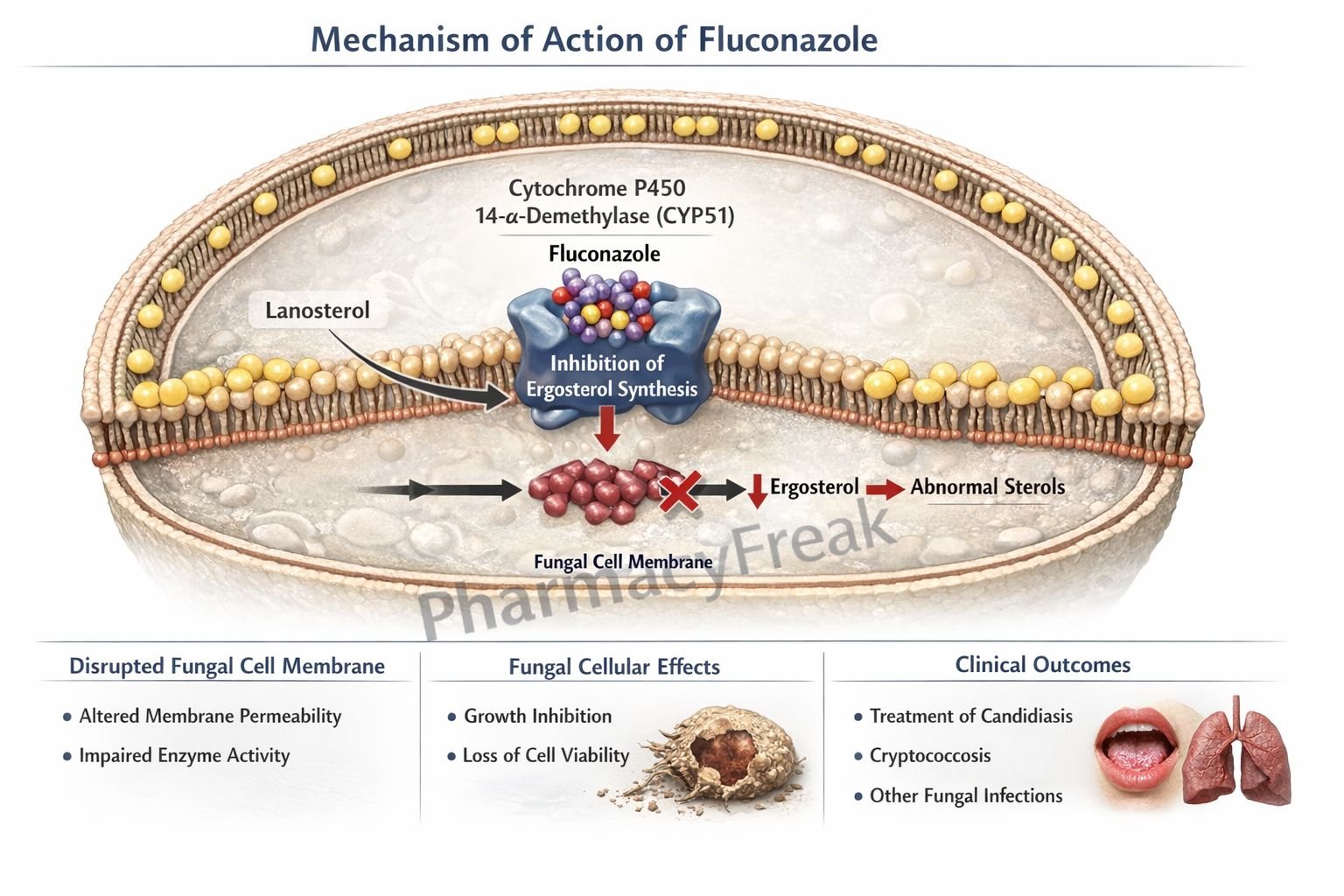
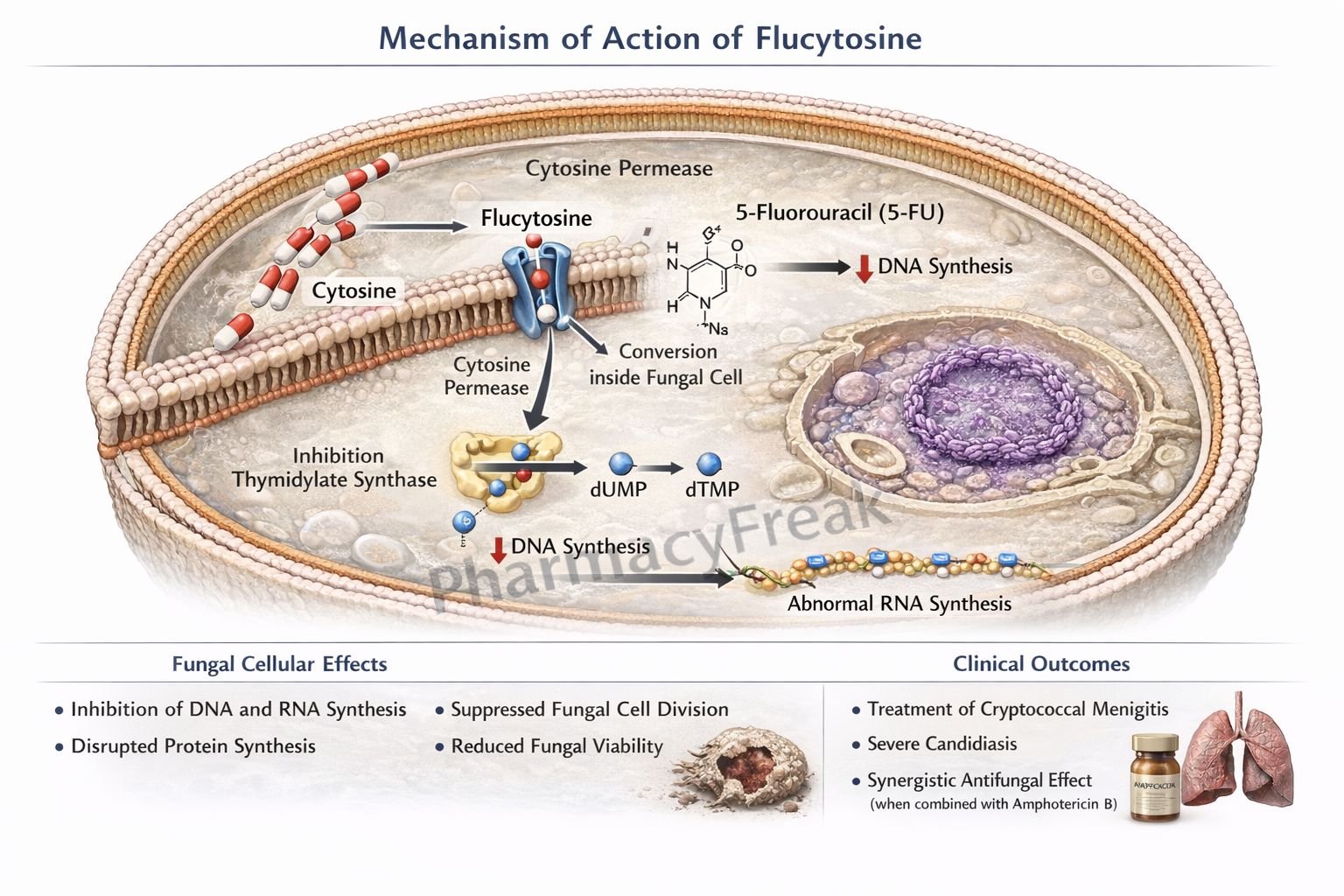
2. Enzymes: Catalysts as Drug Targets
What Are Enzymes?
Enzymes are proteins that speed up (catalyze) biochemical reactions in the body. Many drugs exert their effects by inhibiting or, less commonly, activating enzymes.
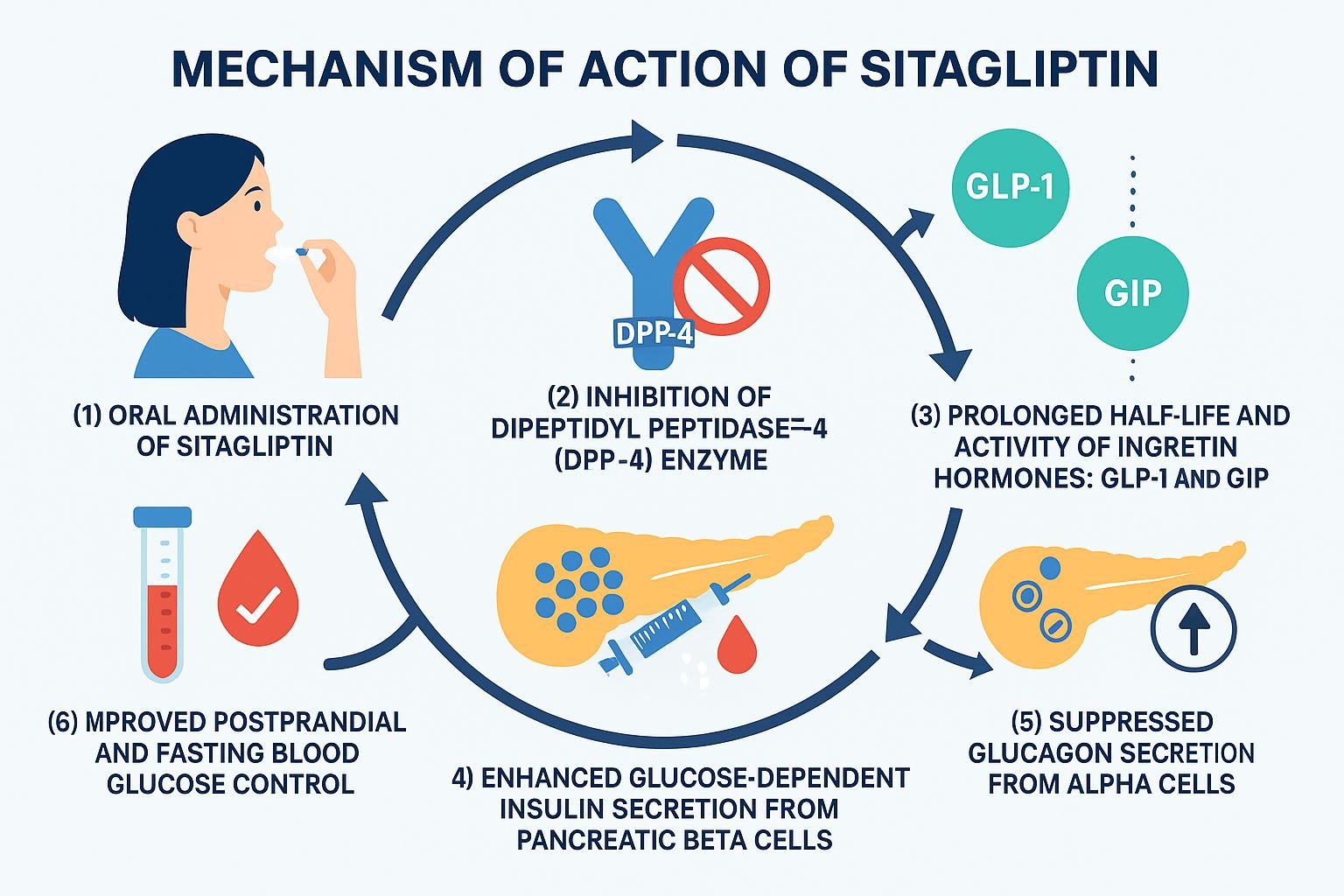
How Drugs Interact with Enzymes
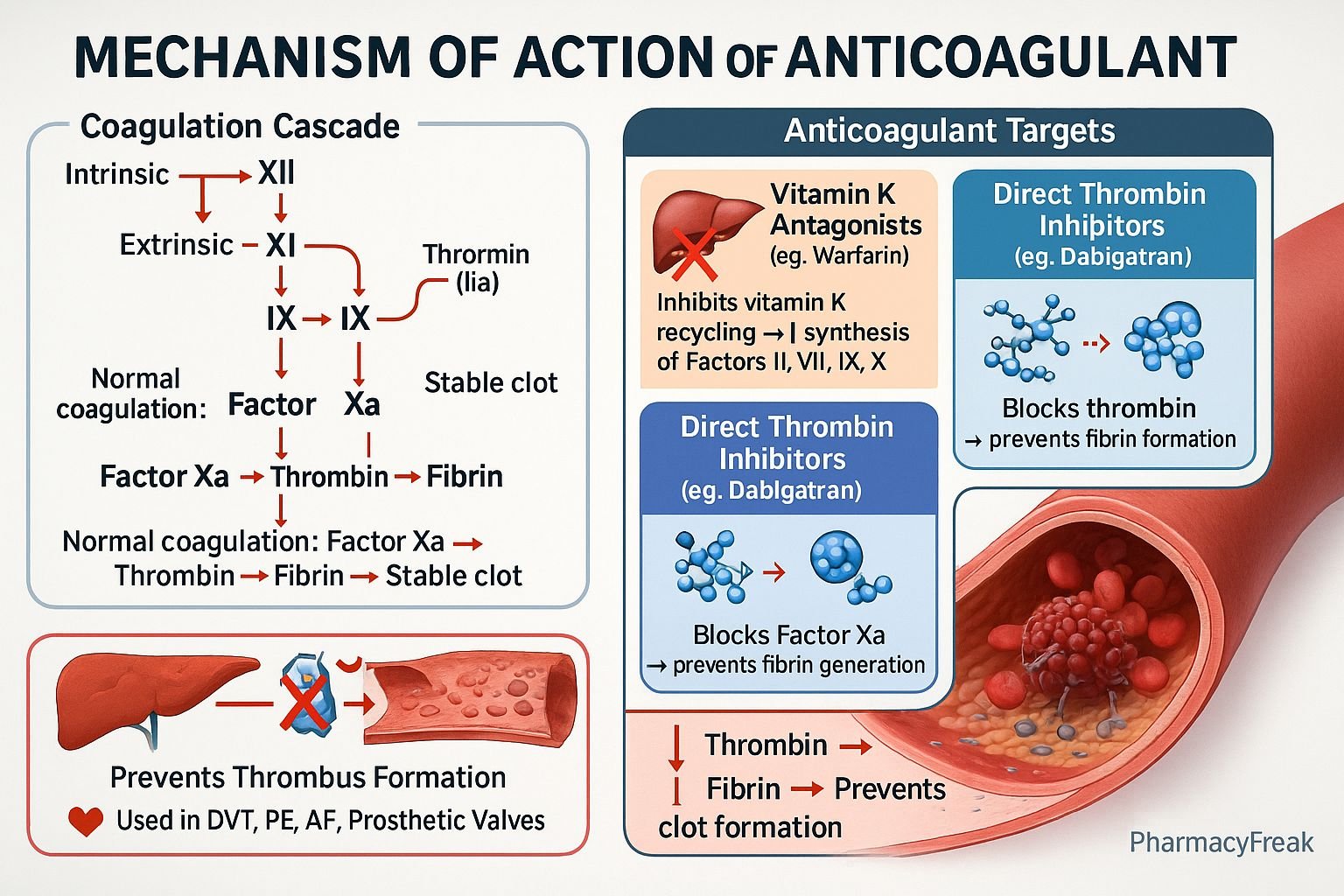
Enzyme Inhibitors: These drugs block the activity of specific enzymes, preventing the formation of certain products or the breakdown of substances.
Enzyme Activators: These drugs increase enzyme activity, but such drugs are less common in clinical practice.
Examples
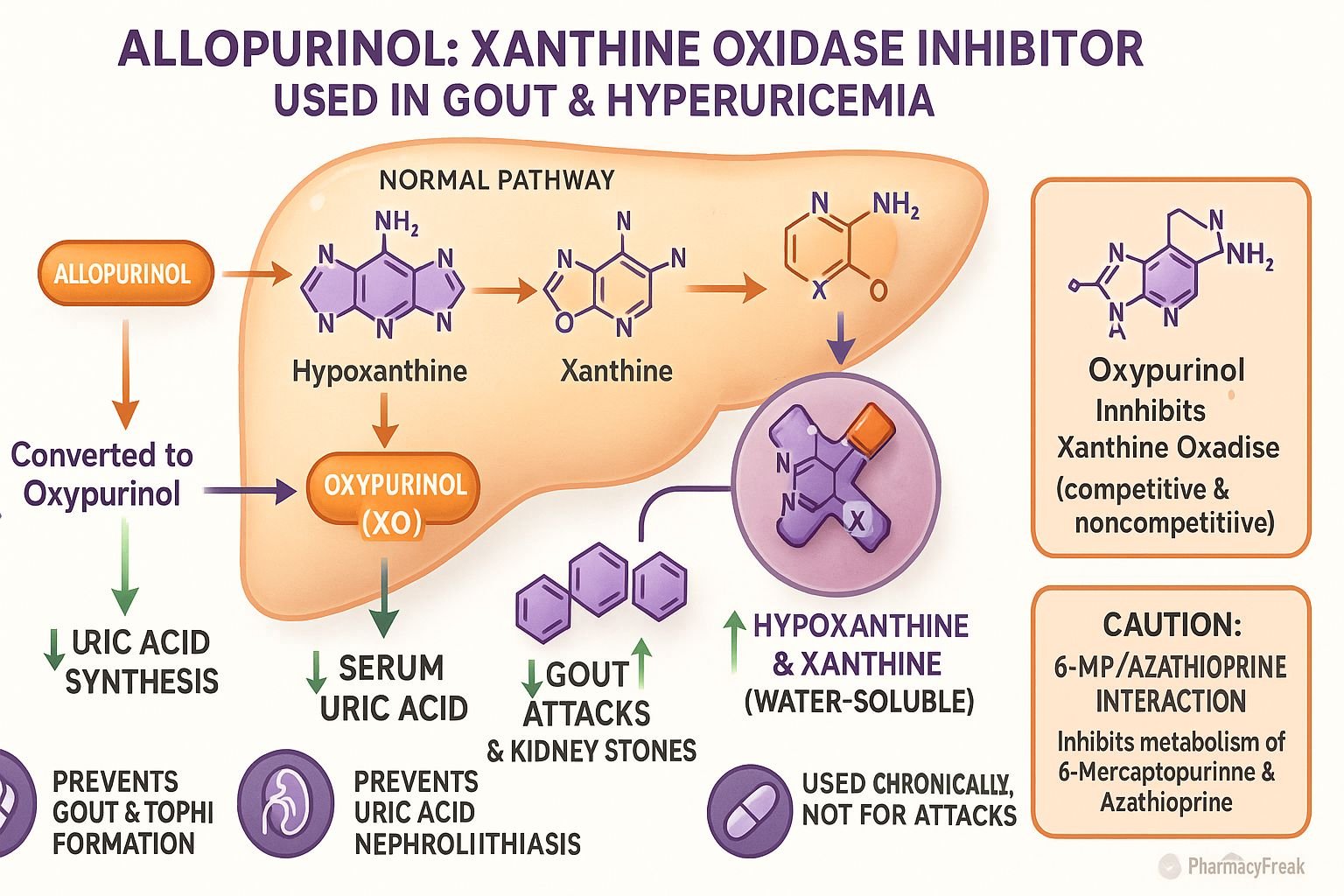
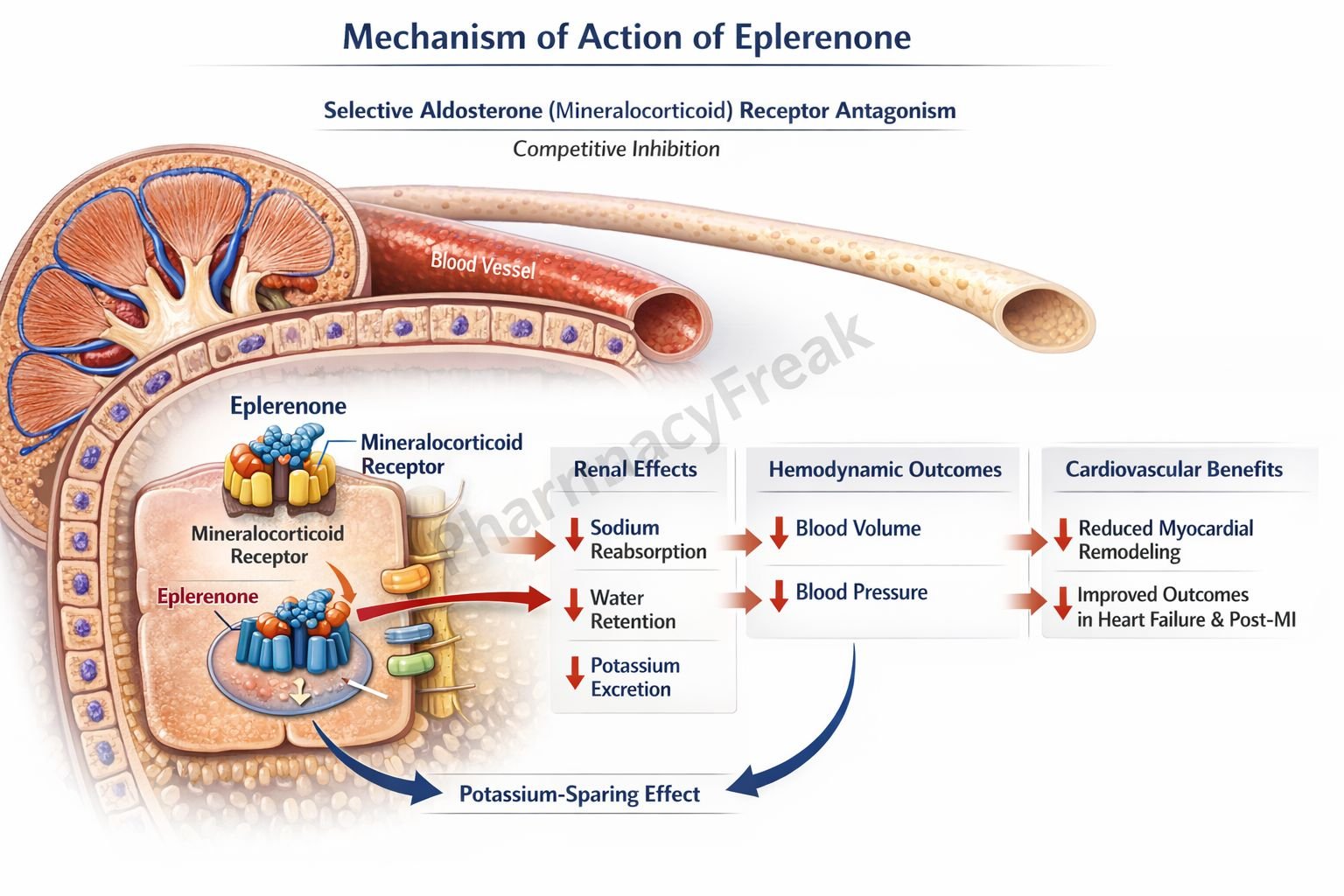
ACE Inhibitors (e.g., enalapril): Inhibit the angiotensin-converting enzyme, decreasing the production of angiotensin II, leading to lower blood pressure.
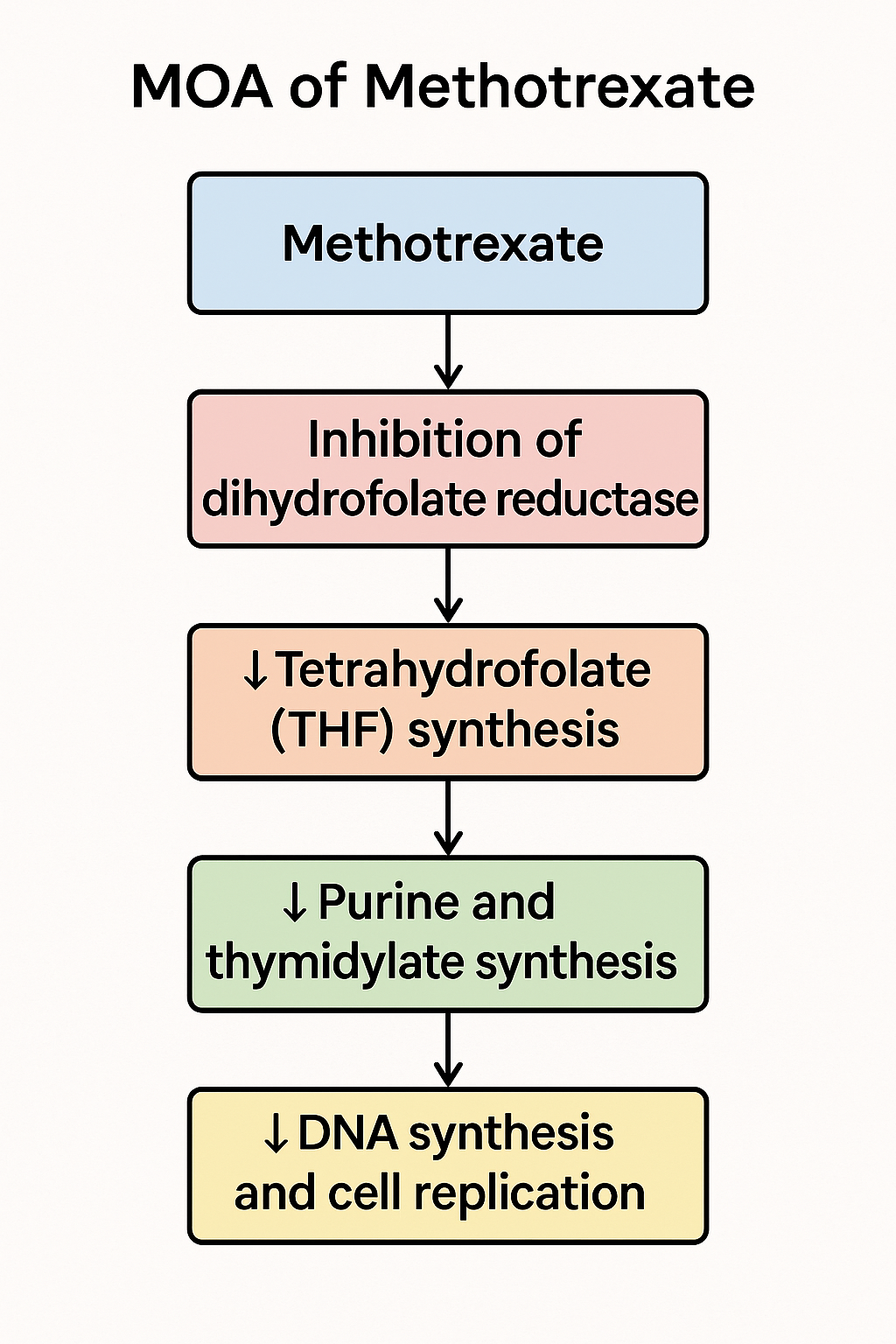
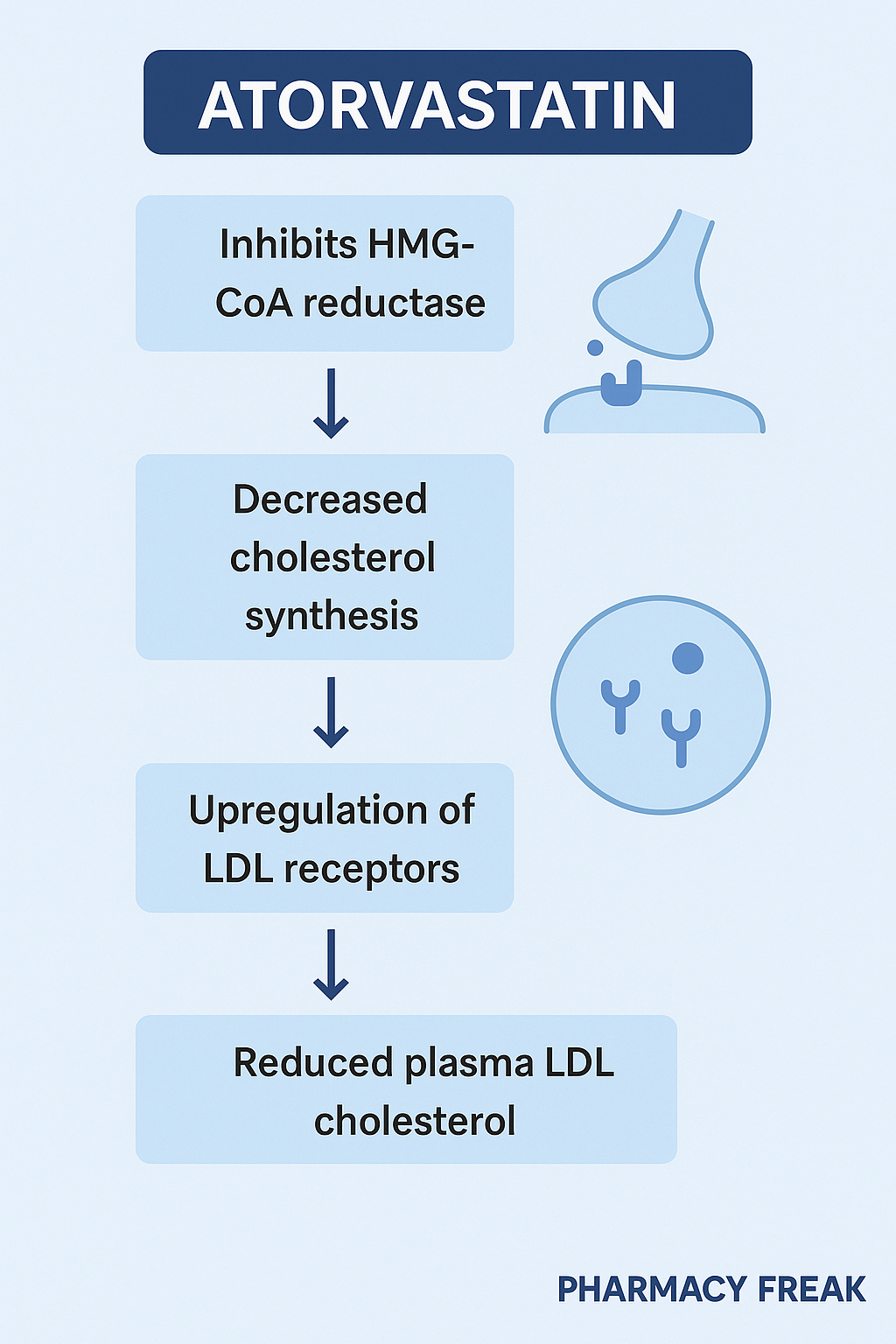
Statins (e.g., atorvastatin): Inhibit HMG-CoA reductase, reducing cholesterol synthesis in the liver.
Acetylcholinesterase inhibitors (e.g., donepezil): Prevent the breakdown of acetylcholine, used in Alzheimer’s disease to enhance cholinergic transmission.
Clinical Relevance
Enzyme inhibition can be highly specific and lead to pronounced clinical effects. However, enzyme inhibitors can sometimes cause toxicity if they also block enzymes involved in detoxification or other vital processes.
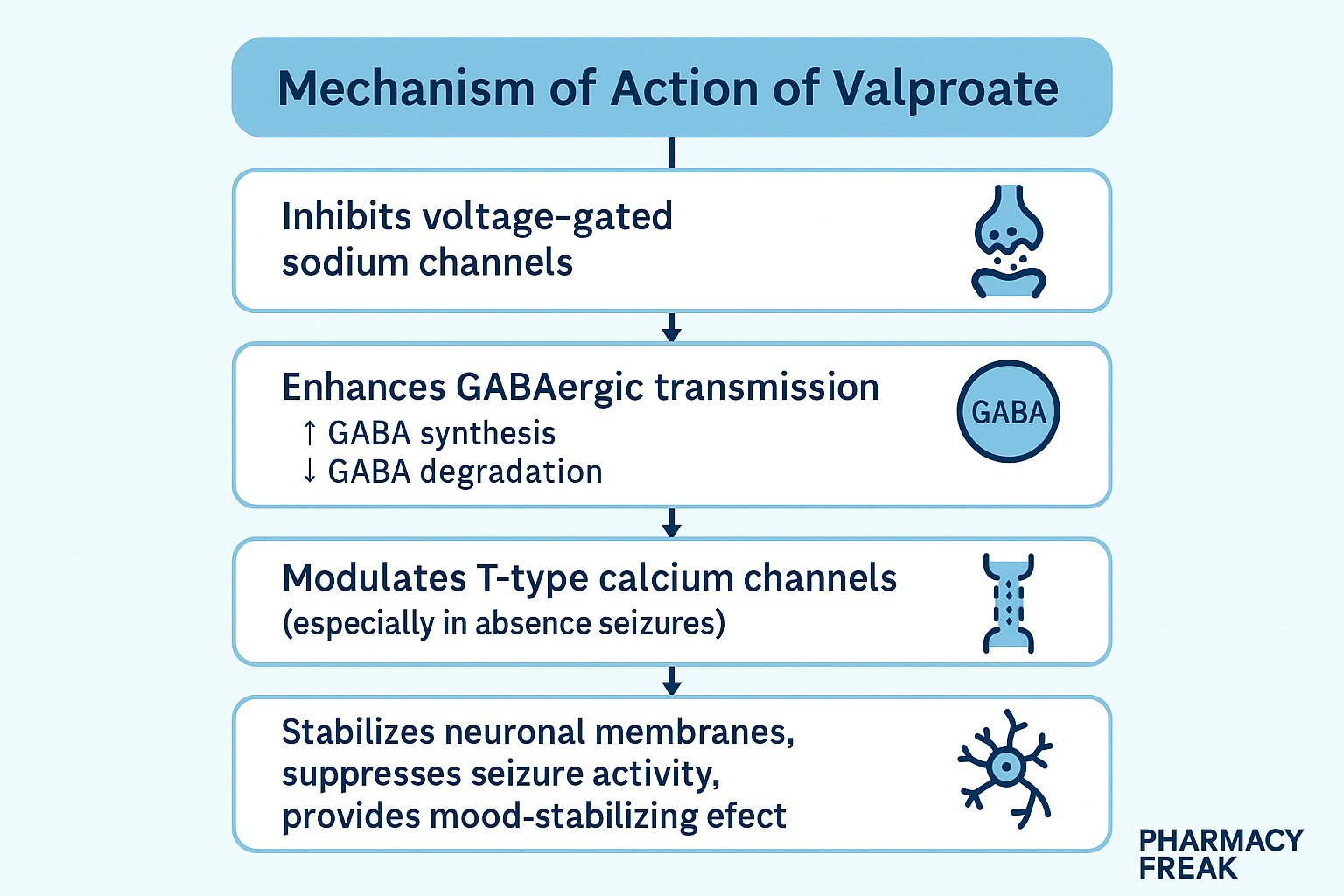
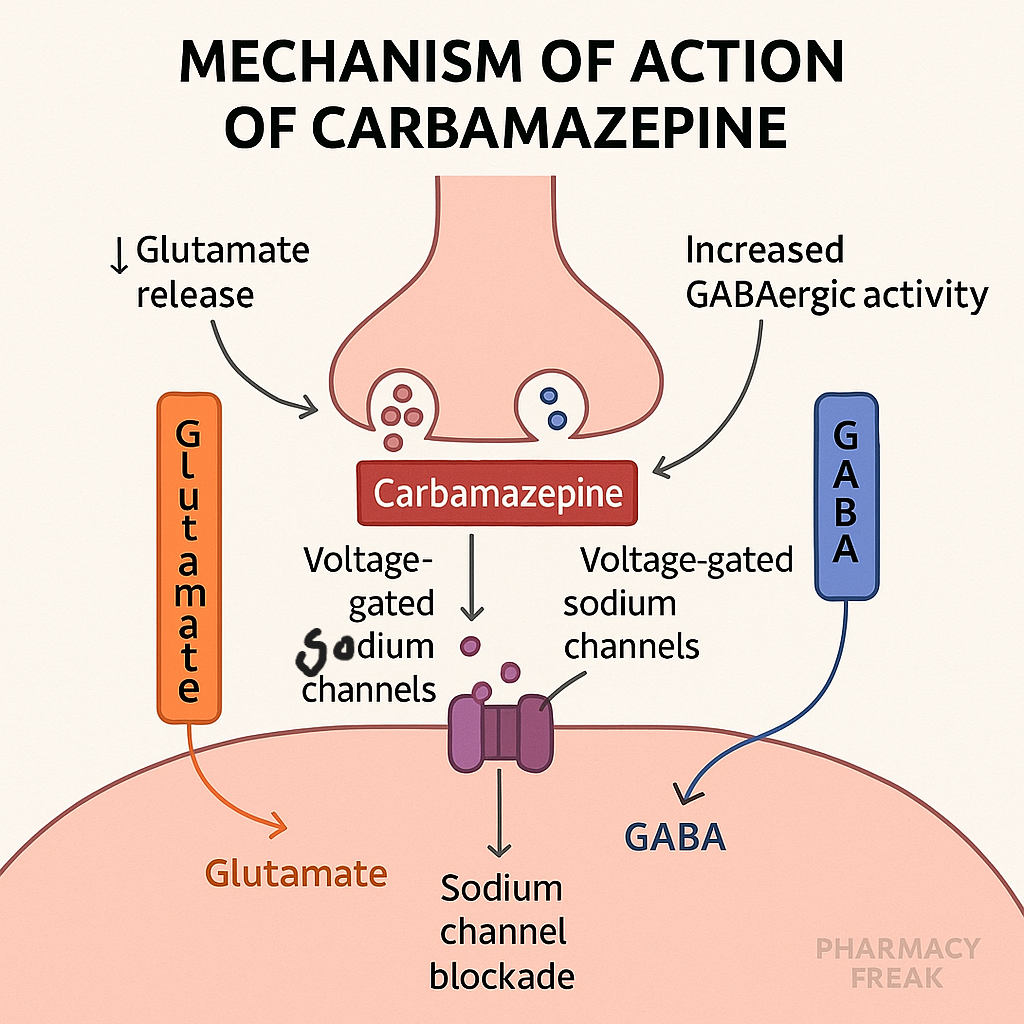
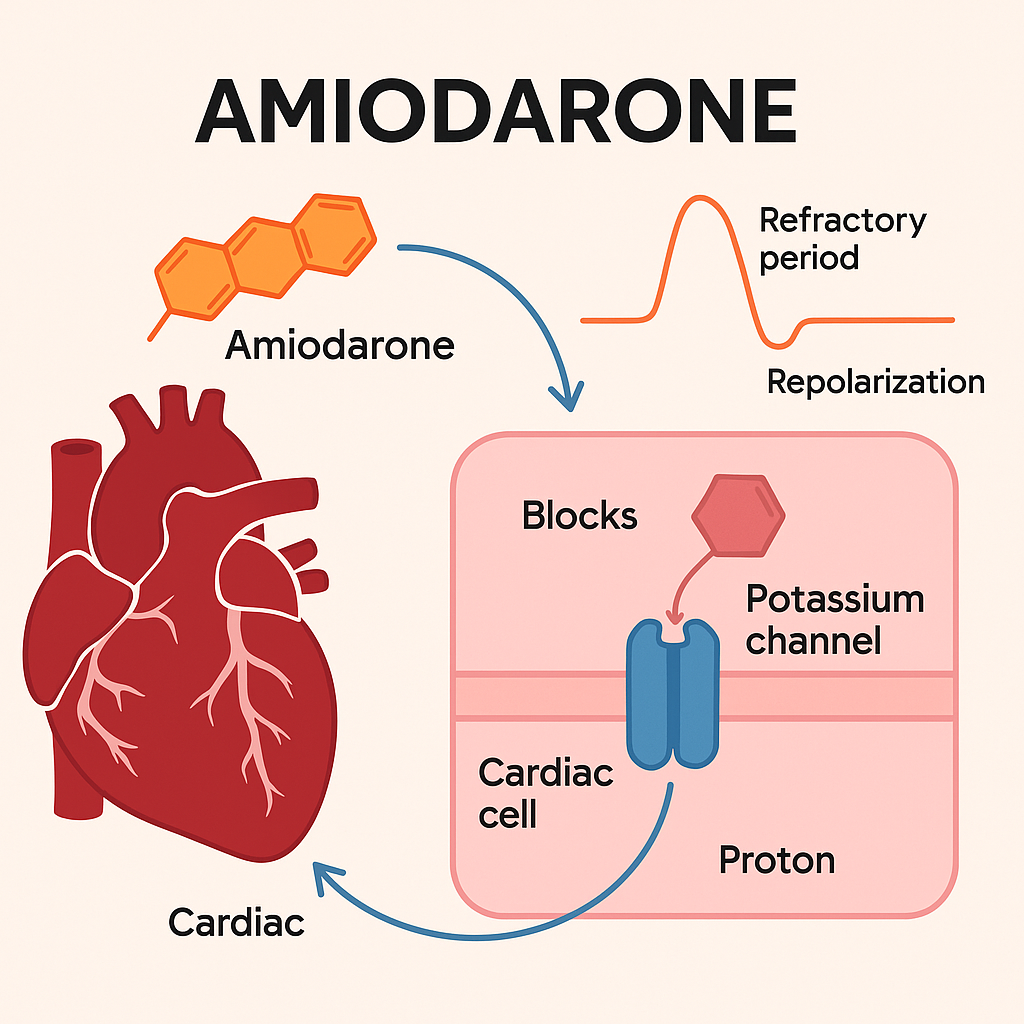
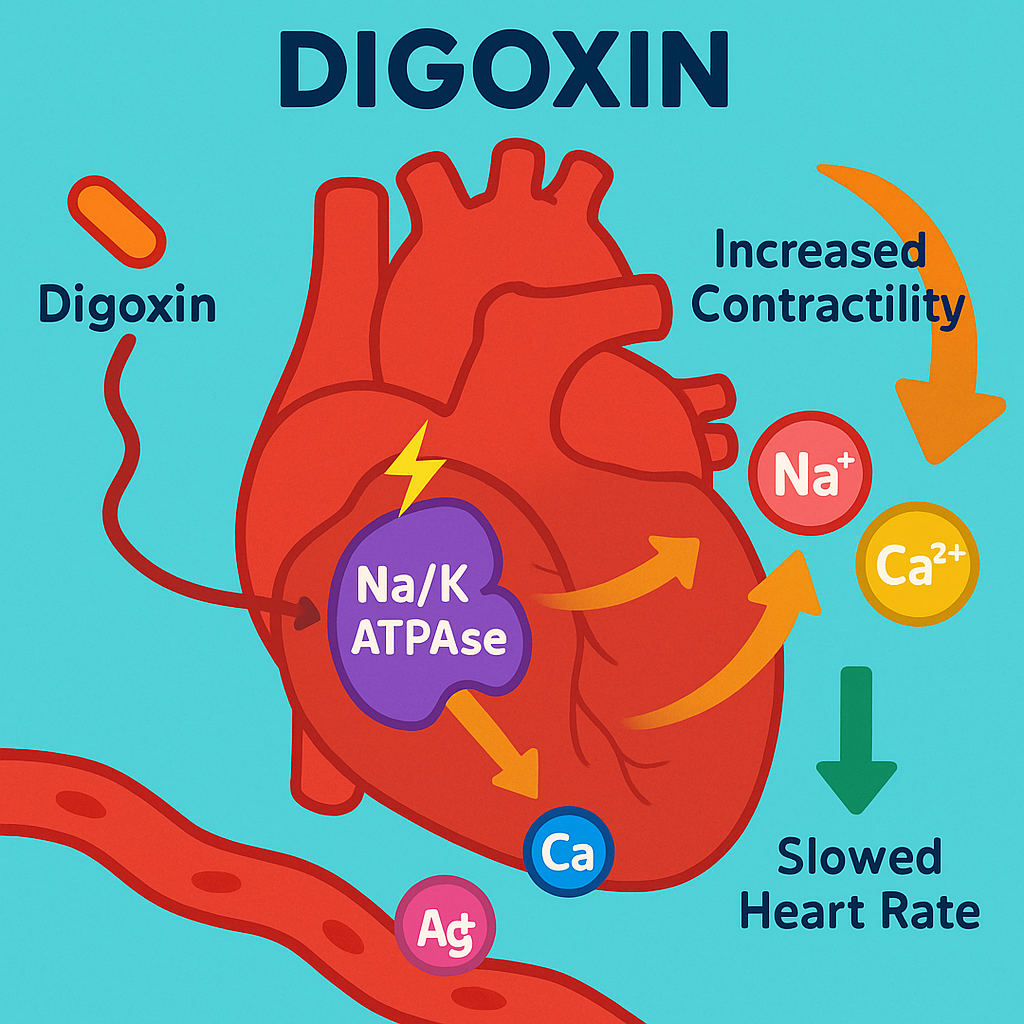
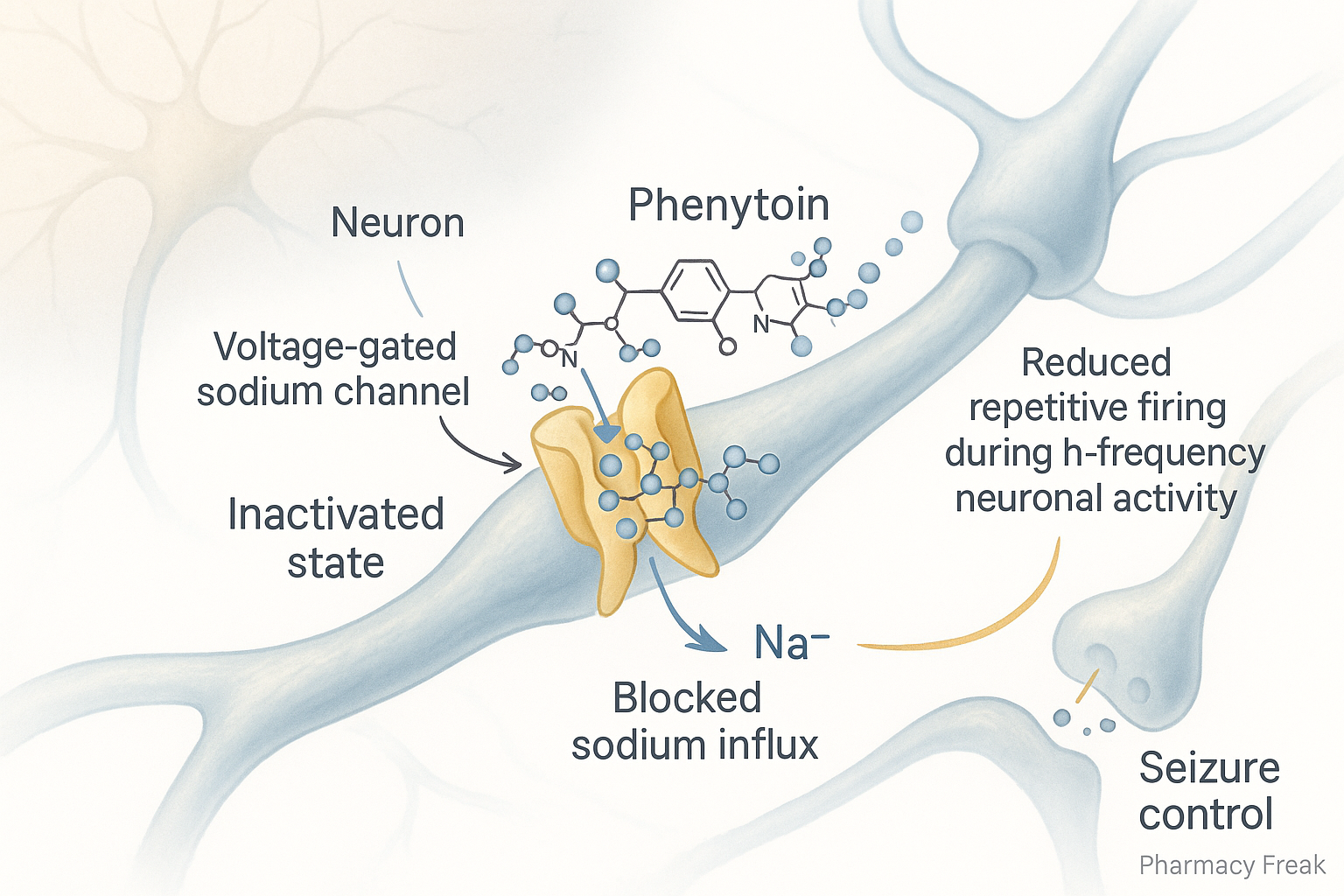
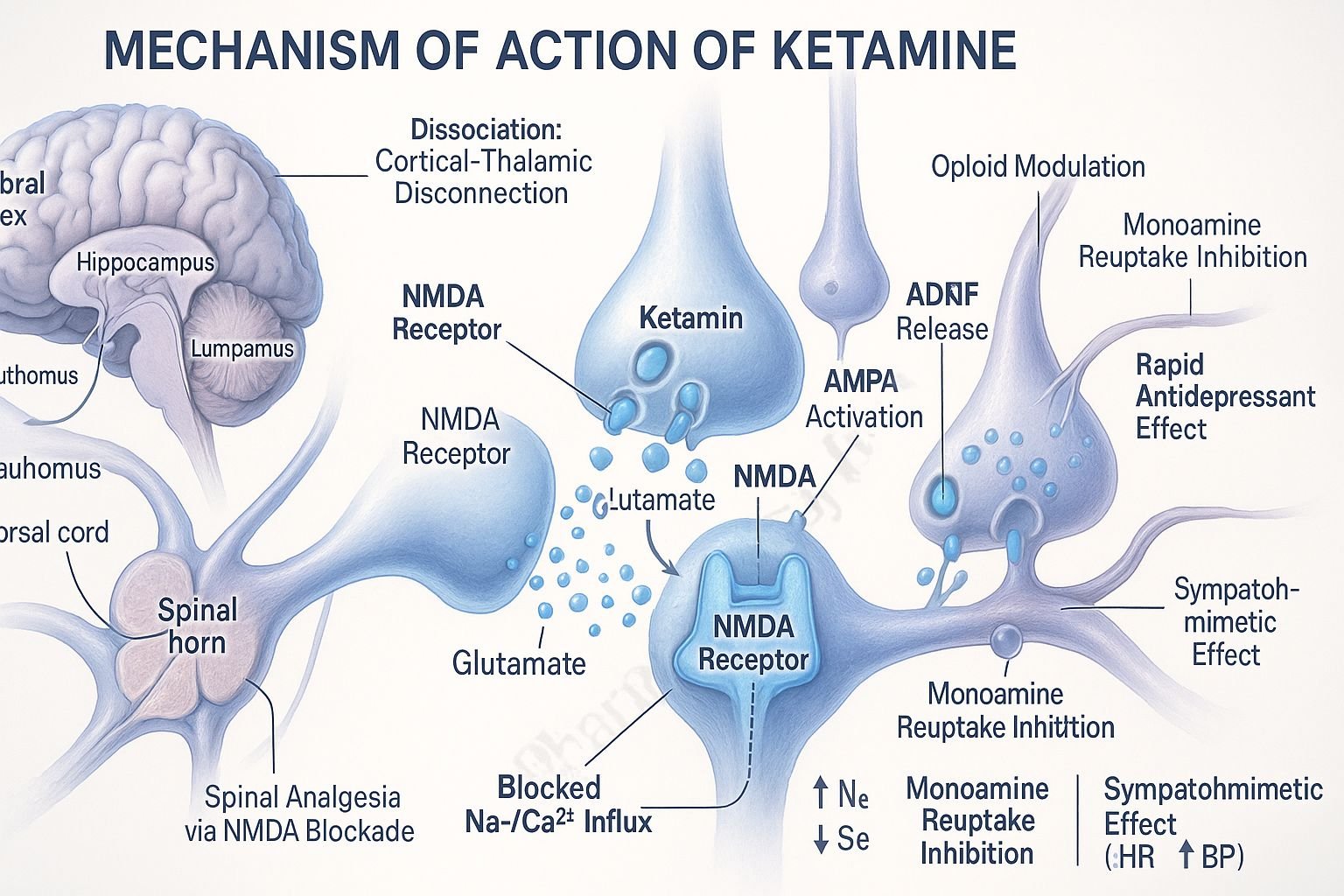
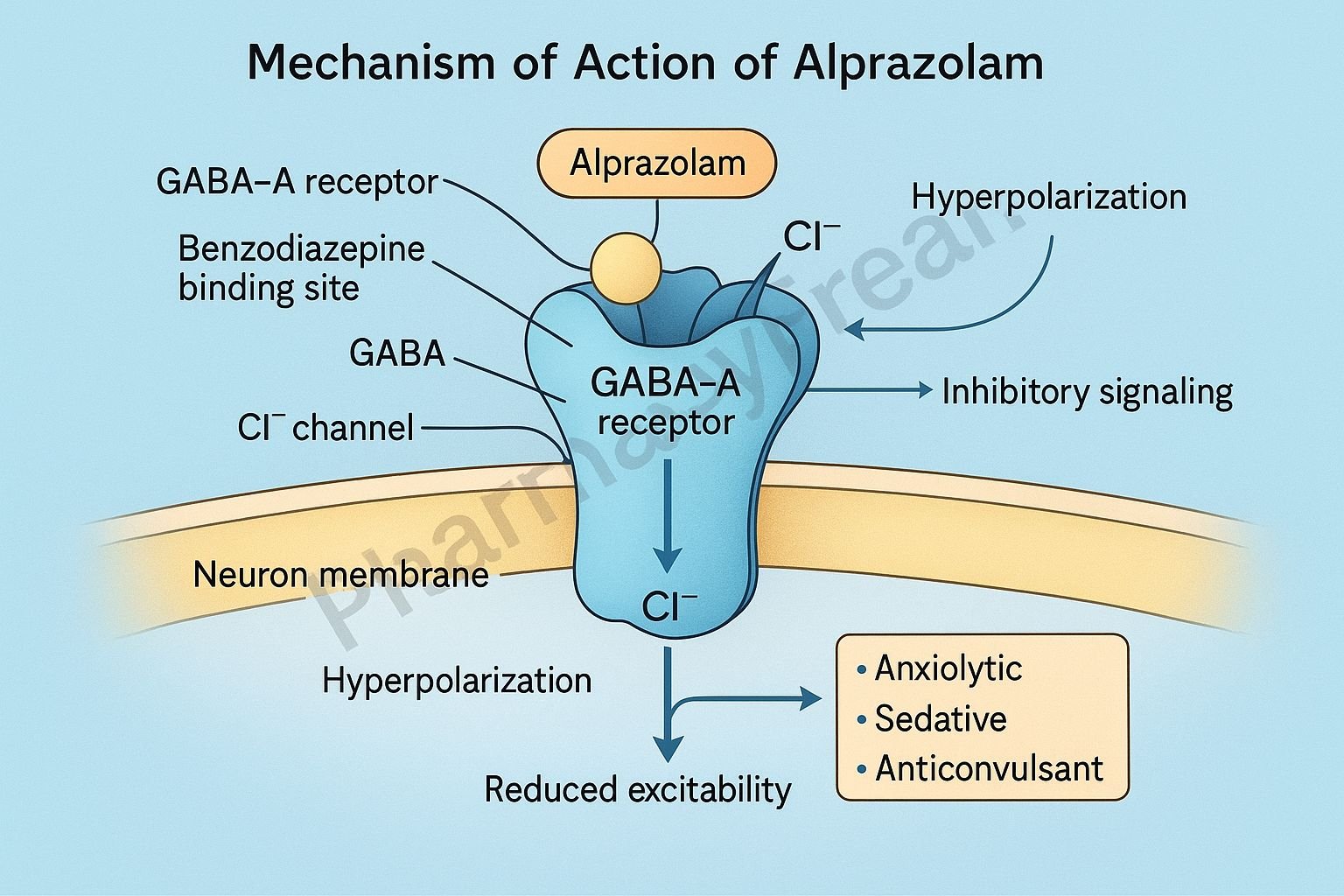
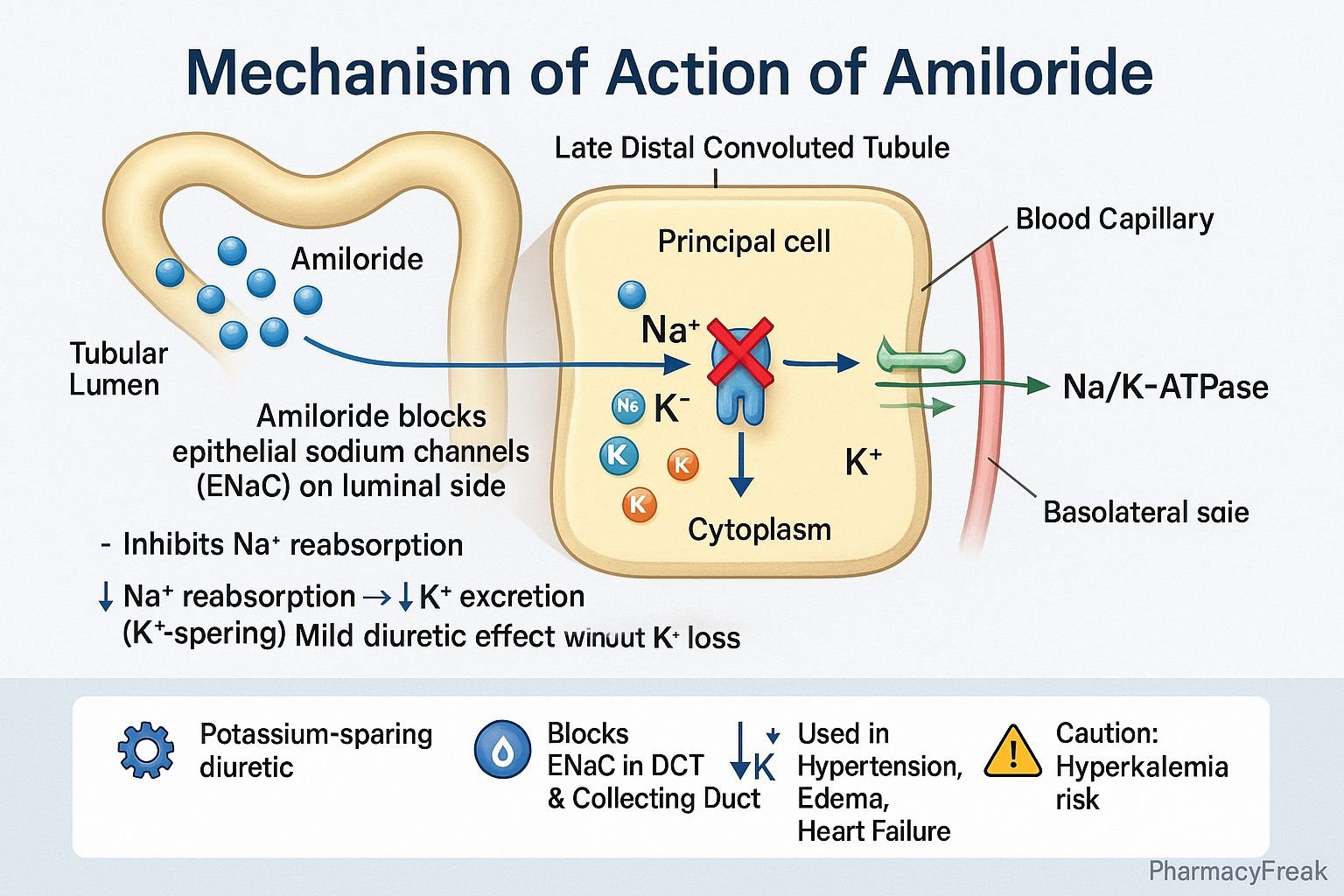
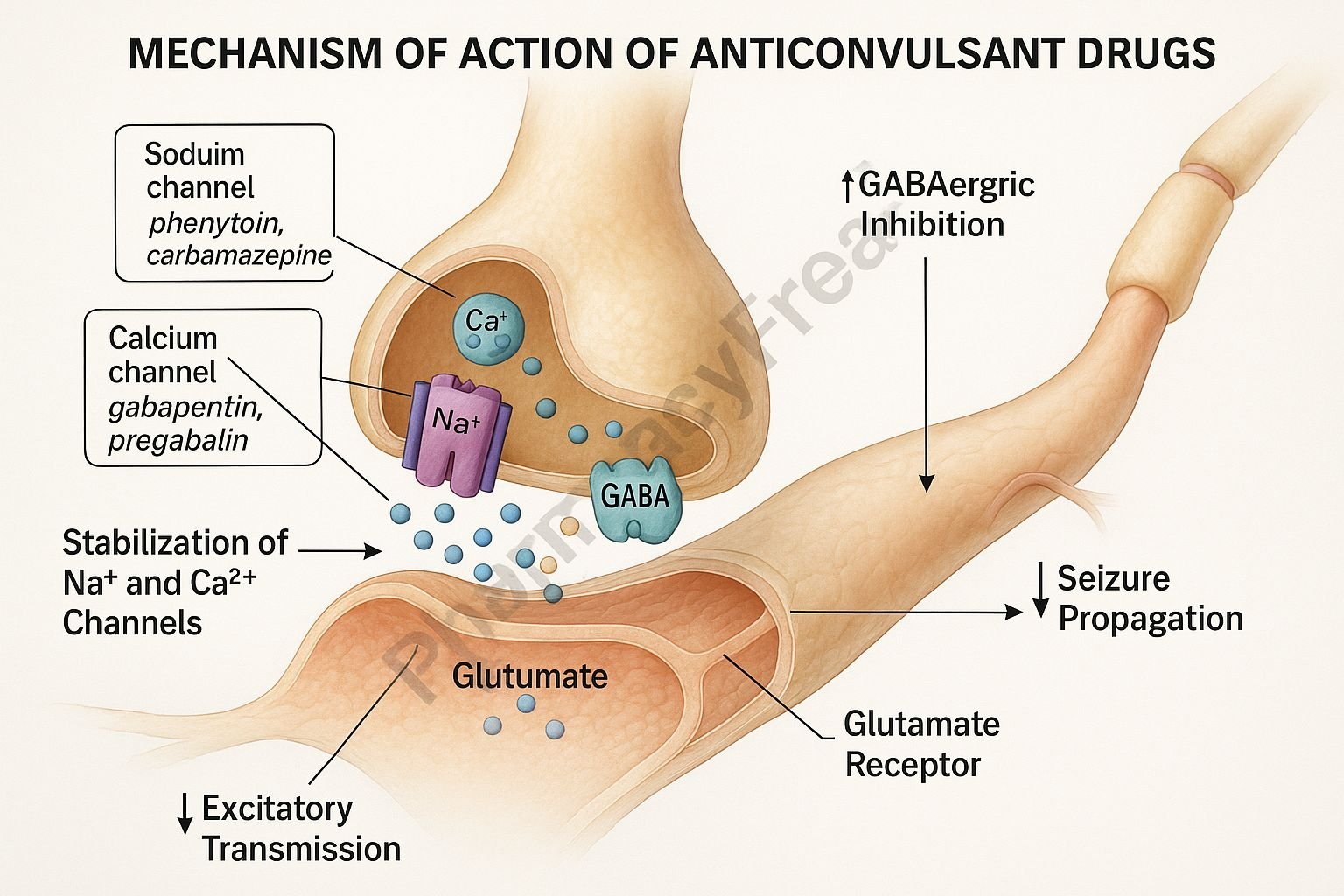
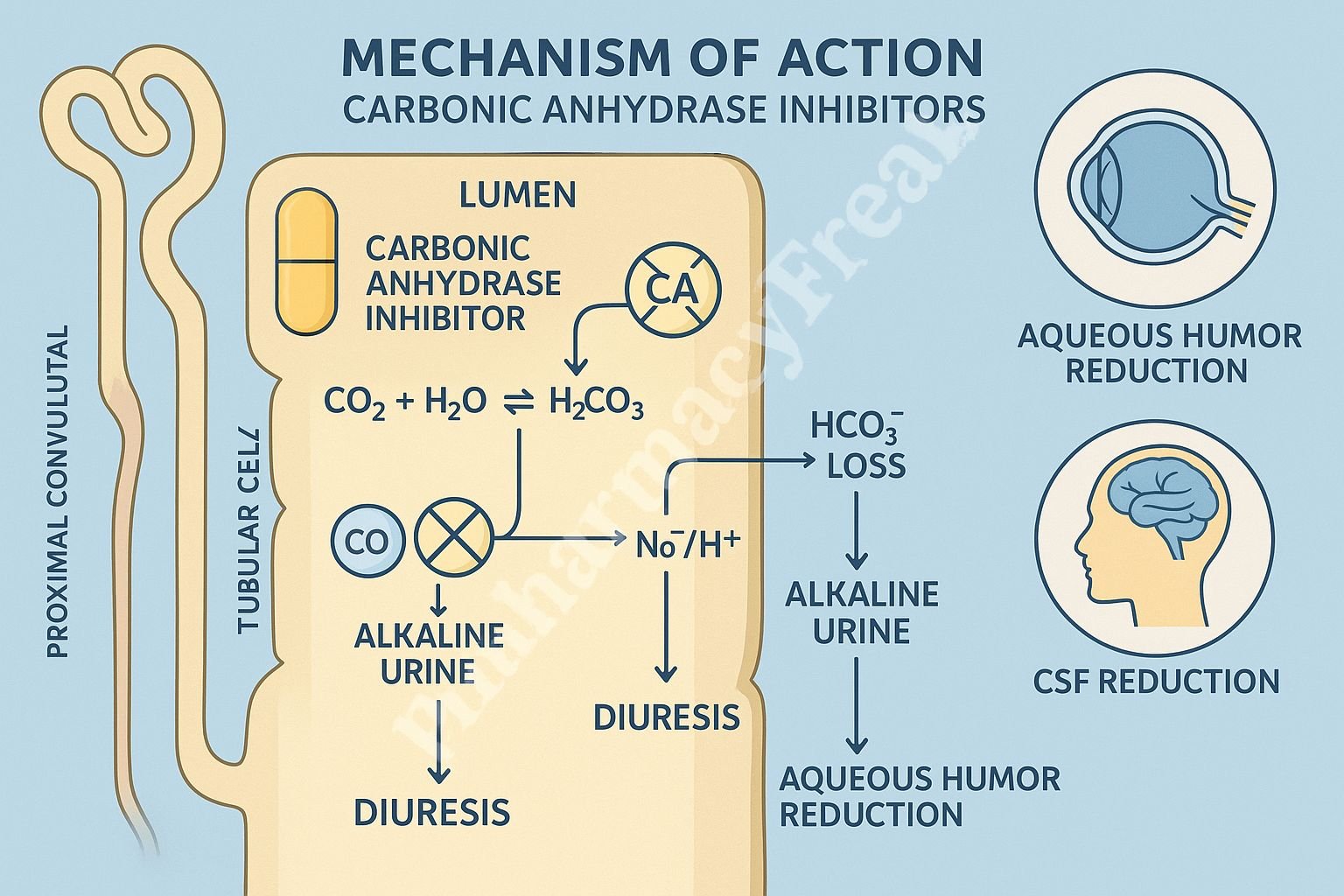
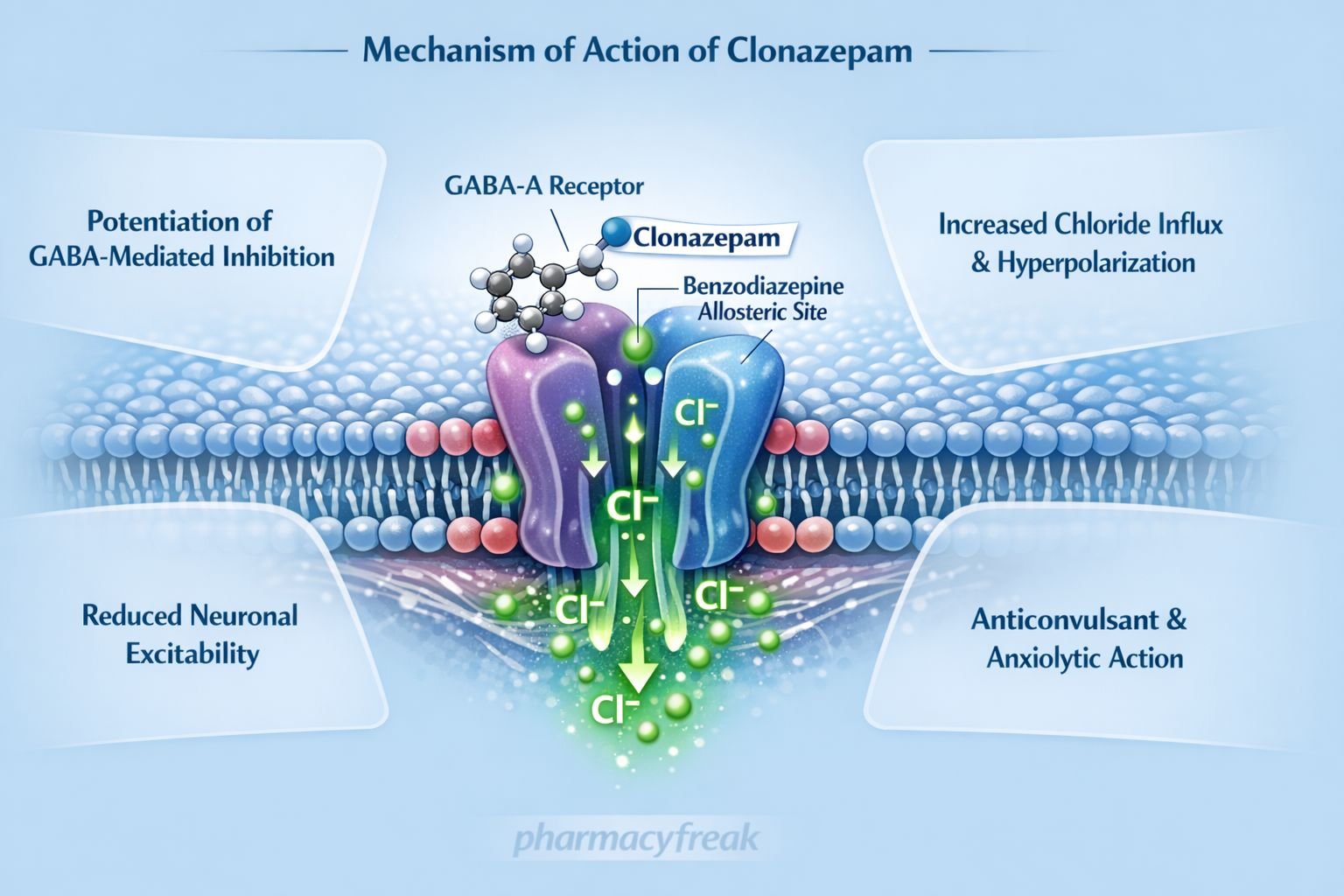
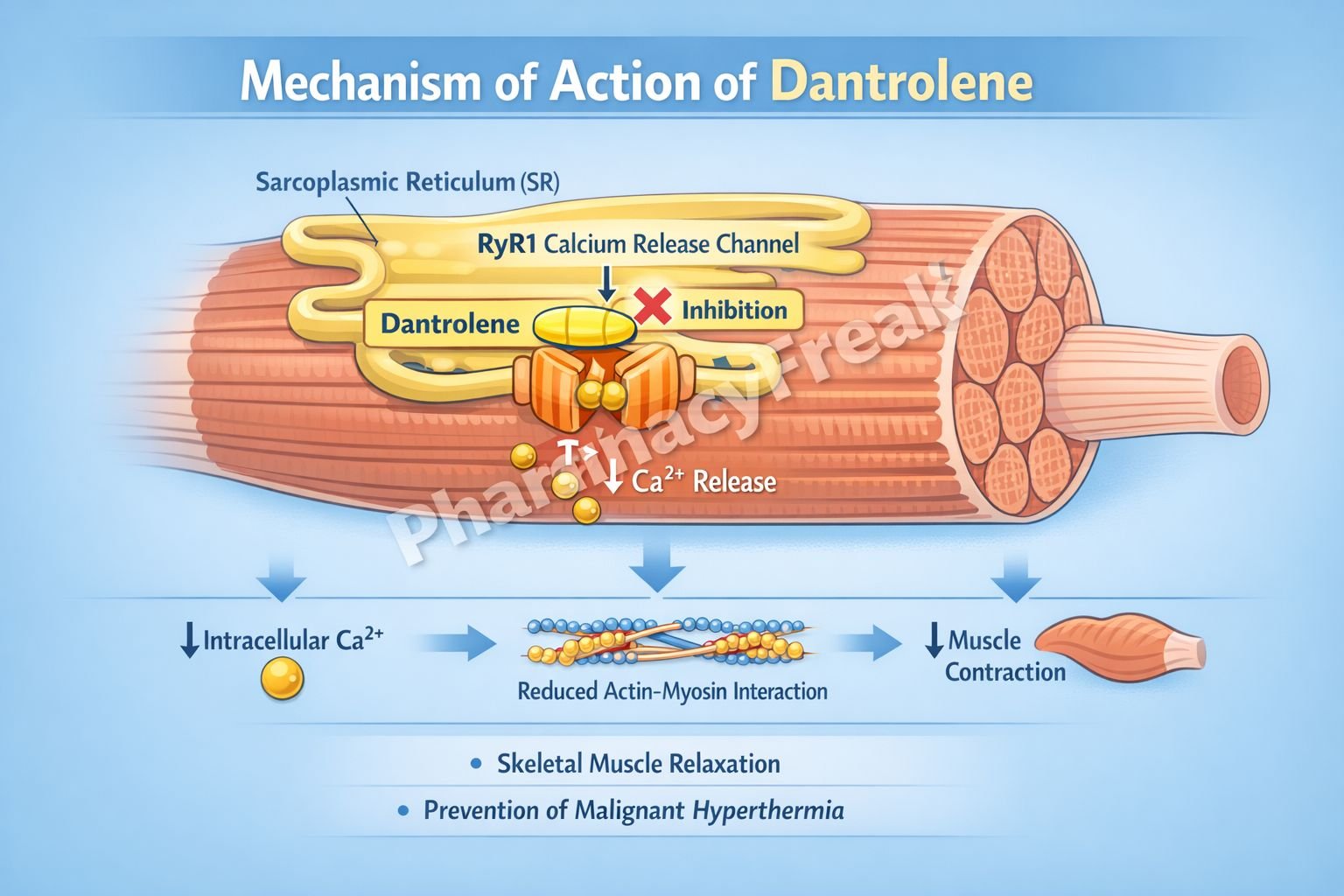
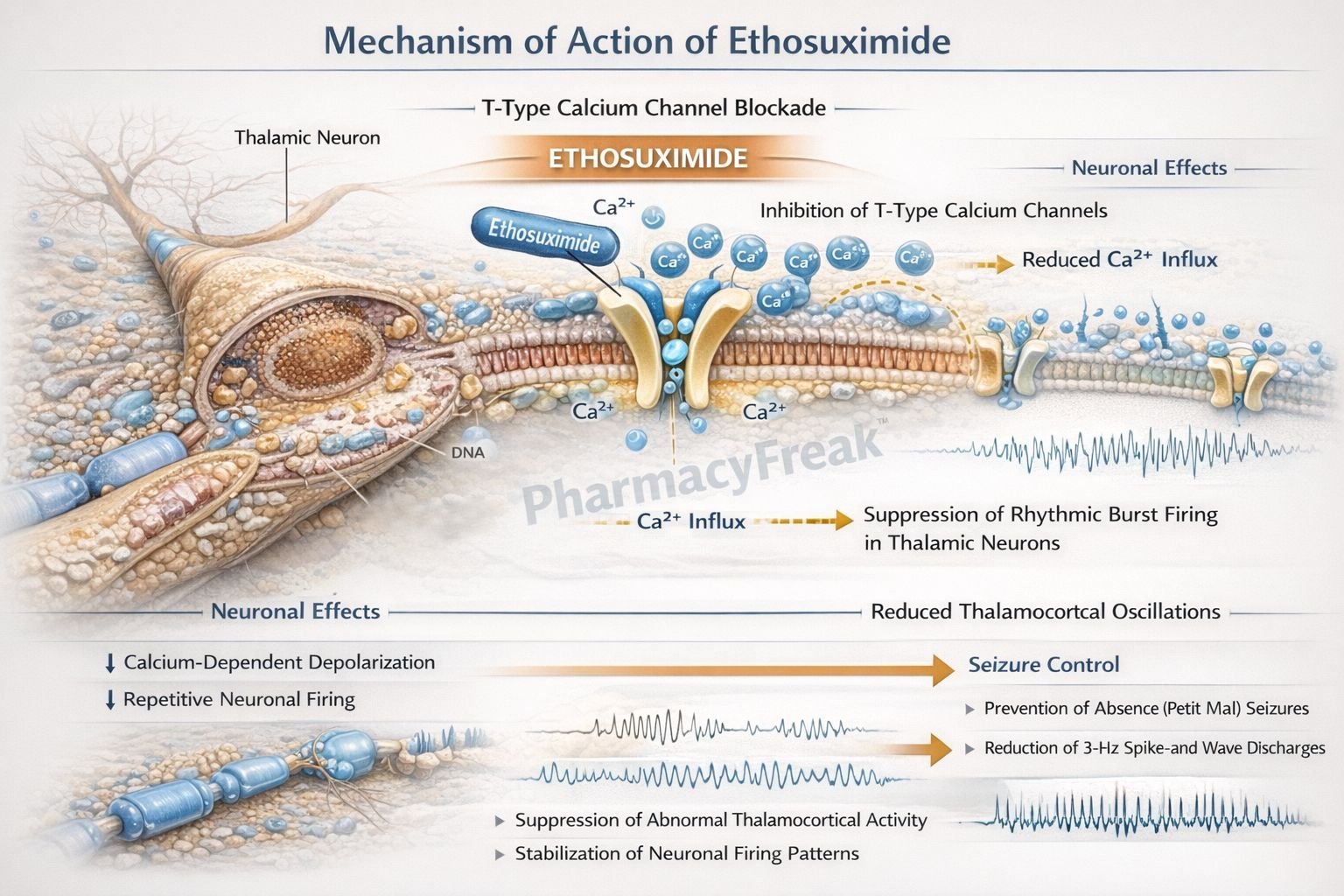
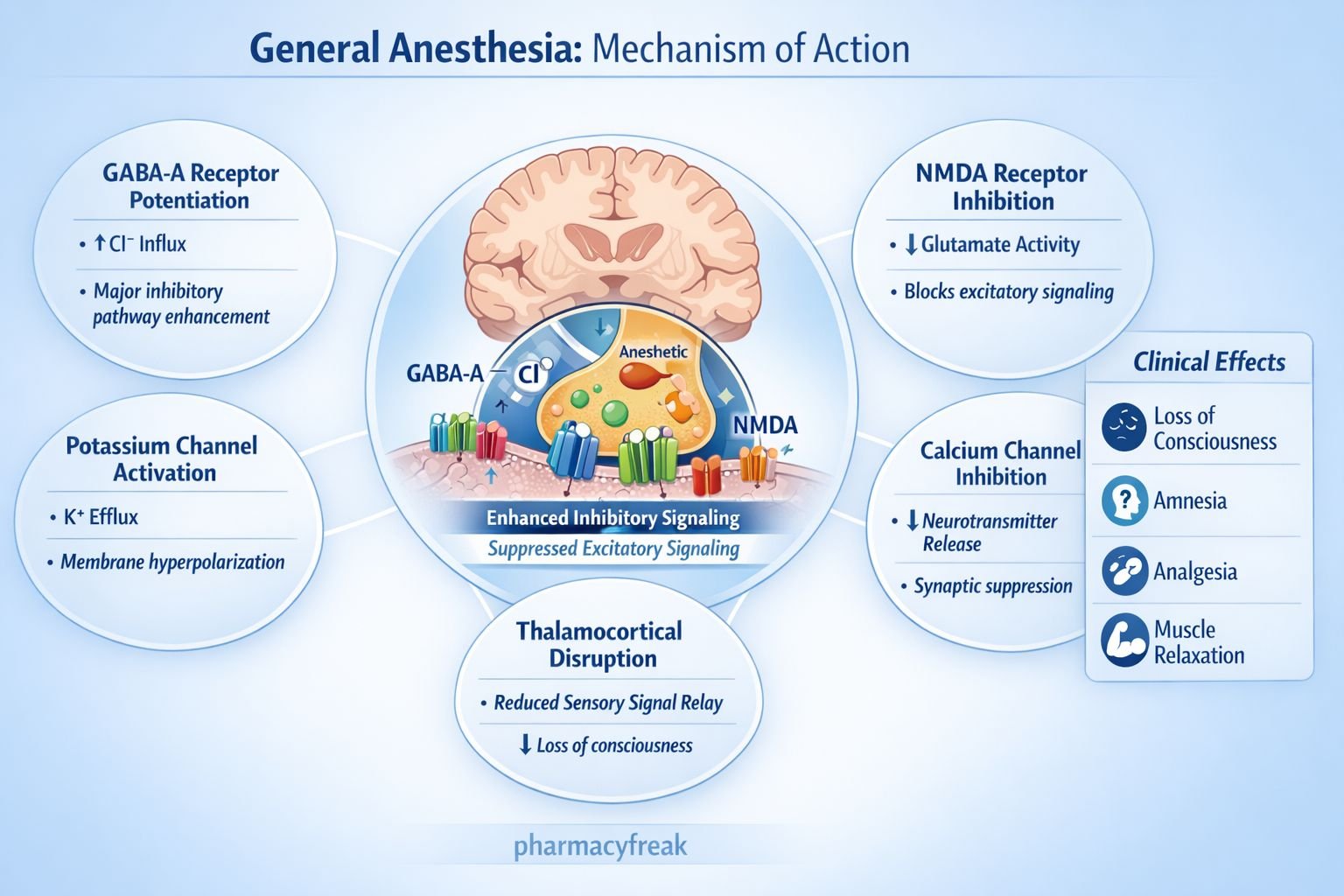
3. Ion Channels: Gatekeepers of Cell Function
What Are Ion Channels?
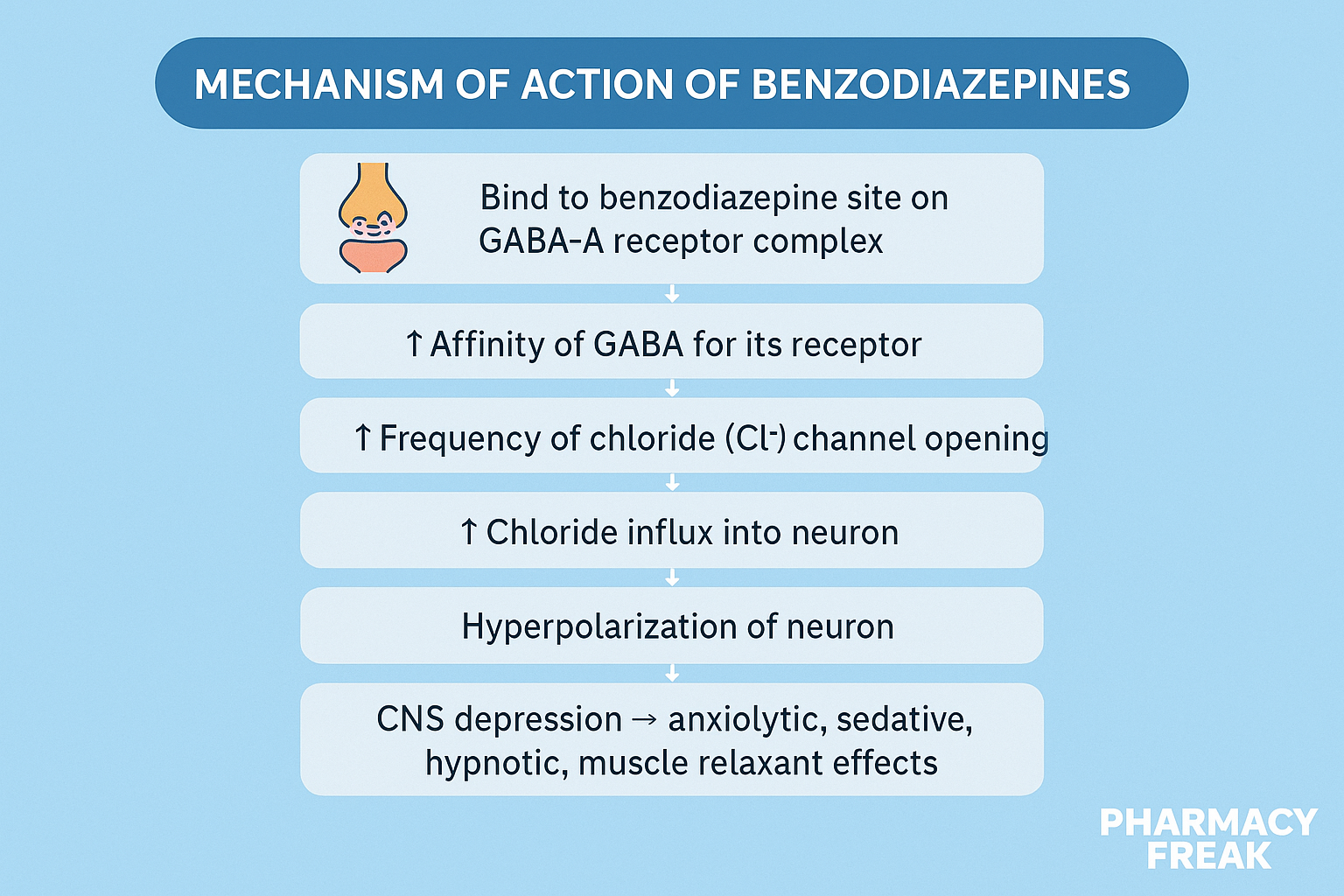
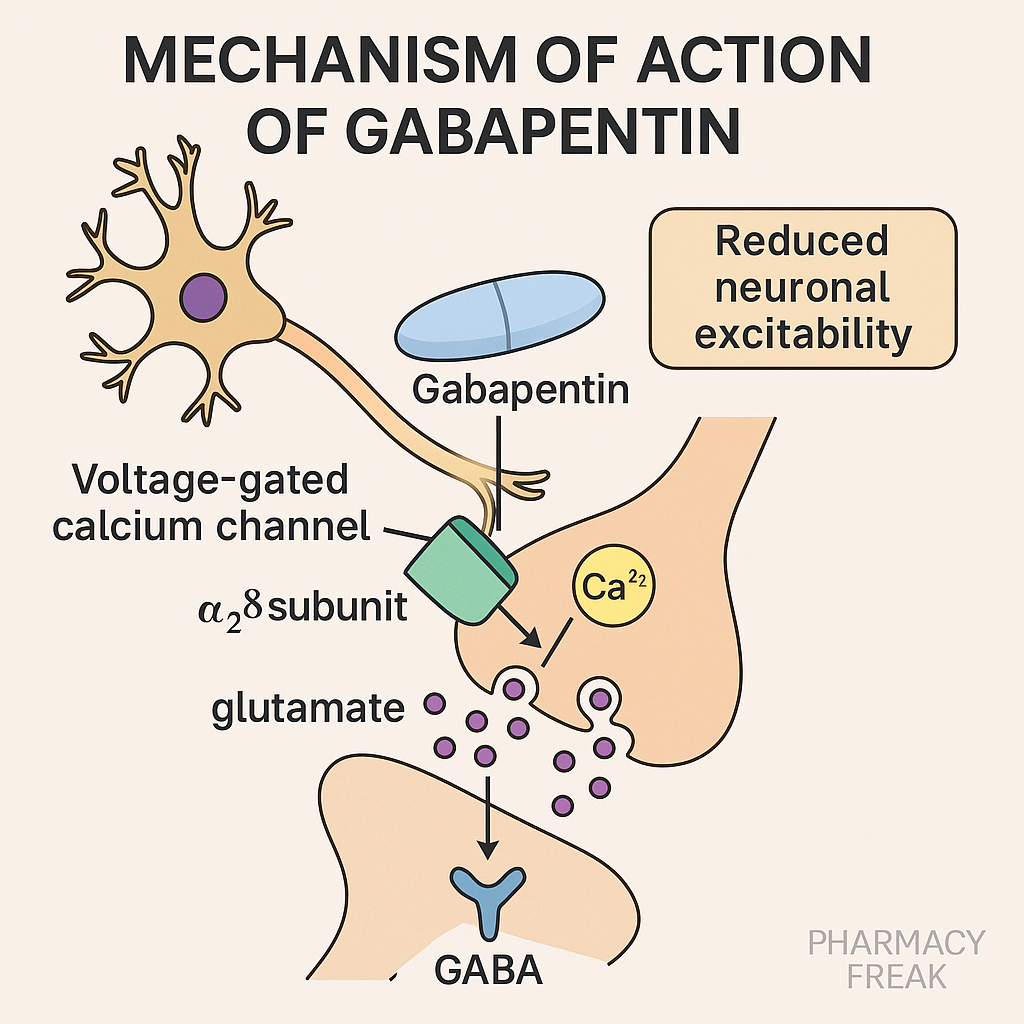
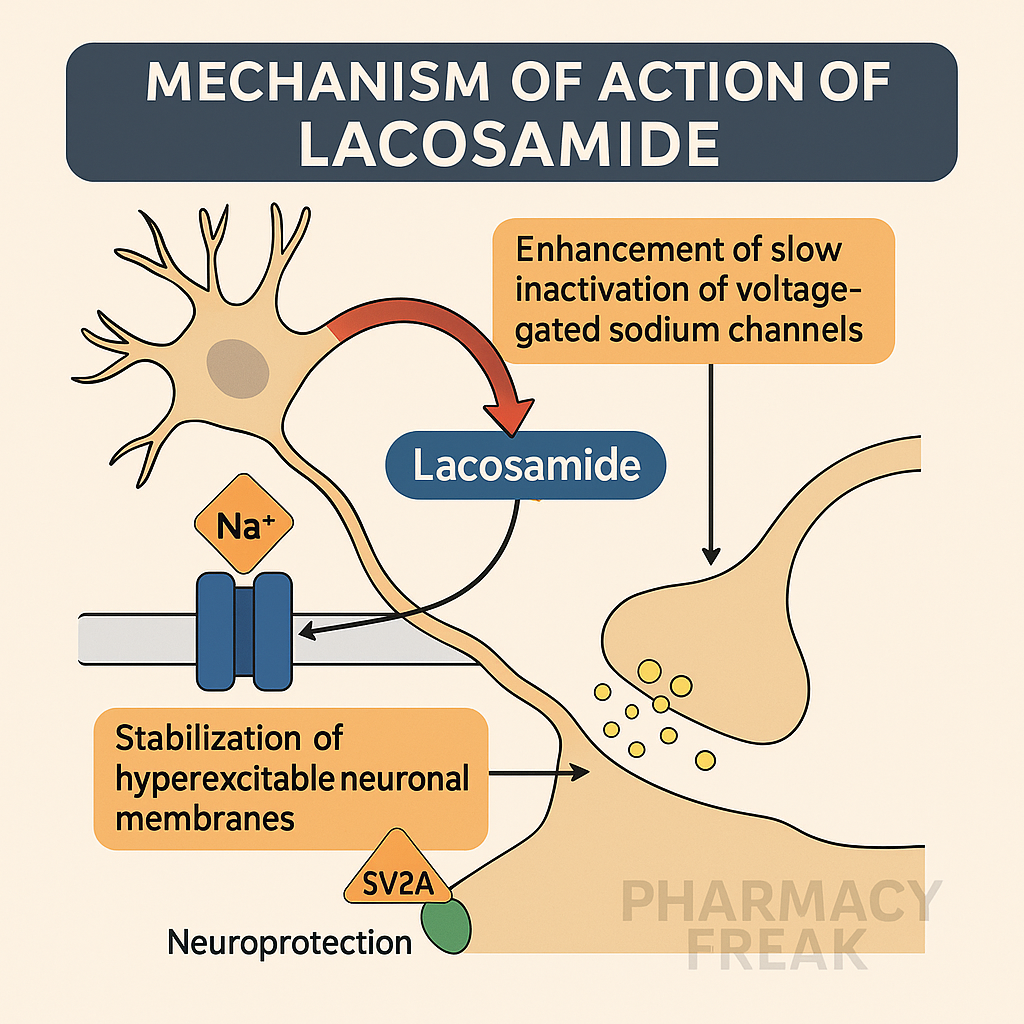
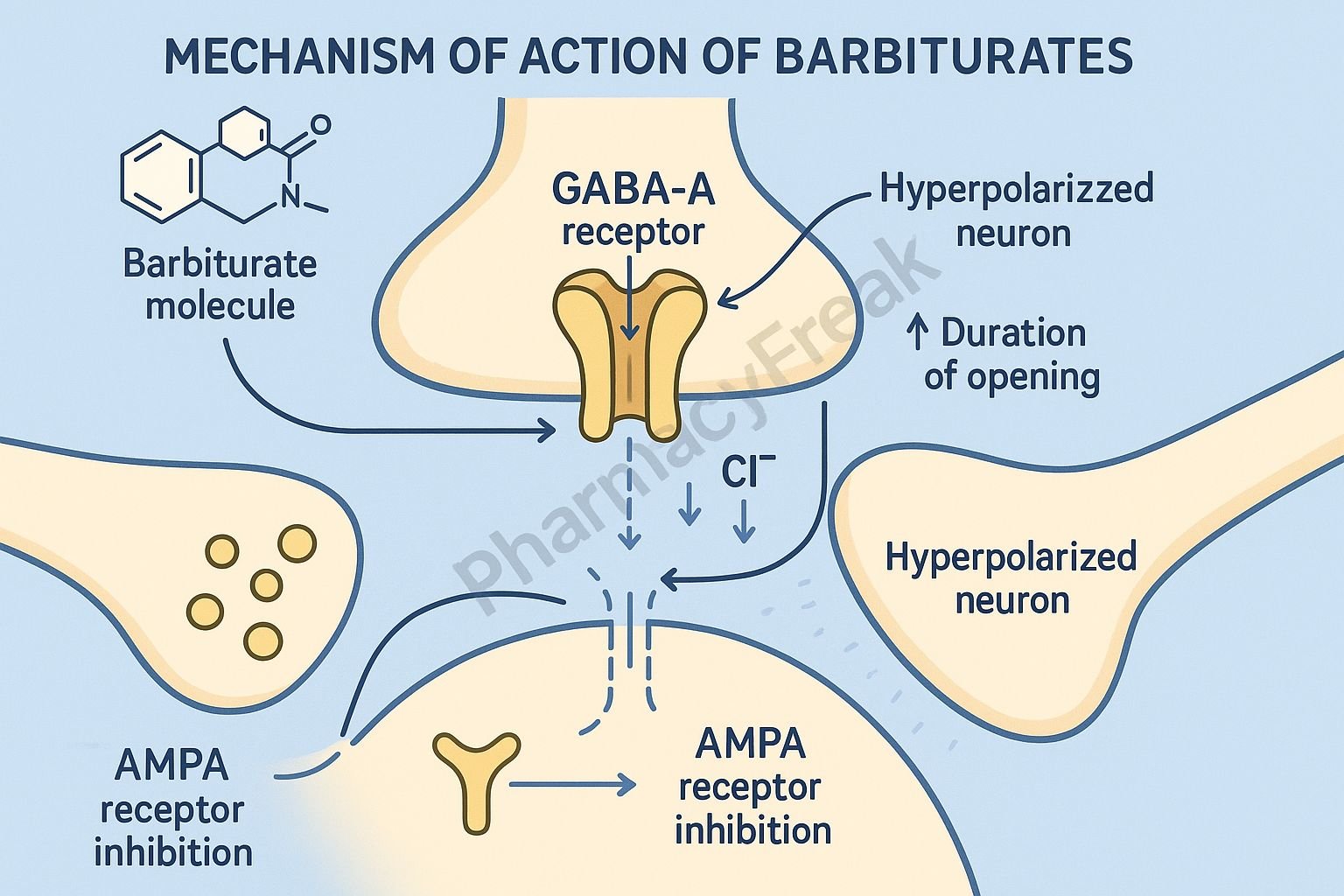
Ion channels are protein structures embedded in cell membranes that allow specific ions (such as sodium, potassium, calcium, or chloride) to pass in and out of cells. These channels play critical roles in electrical signaling in nerves and muscles.
How Drugs Work on Ion Channels
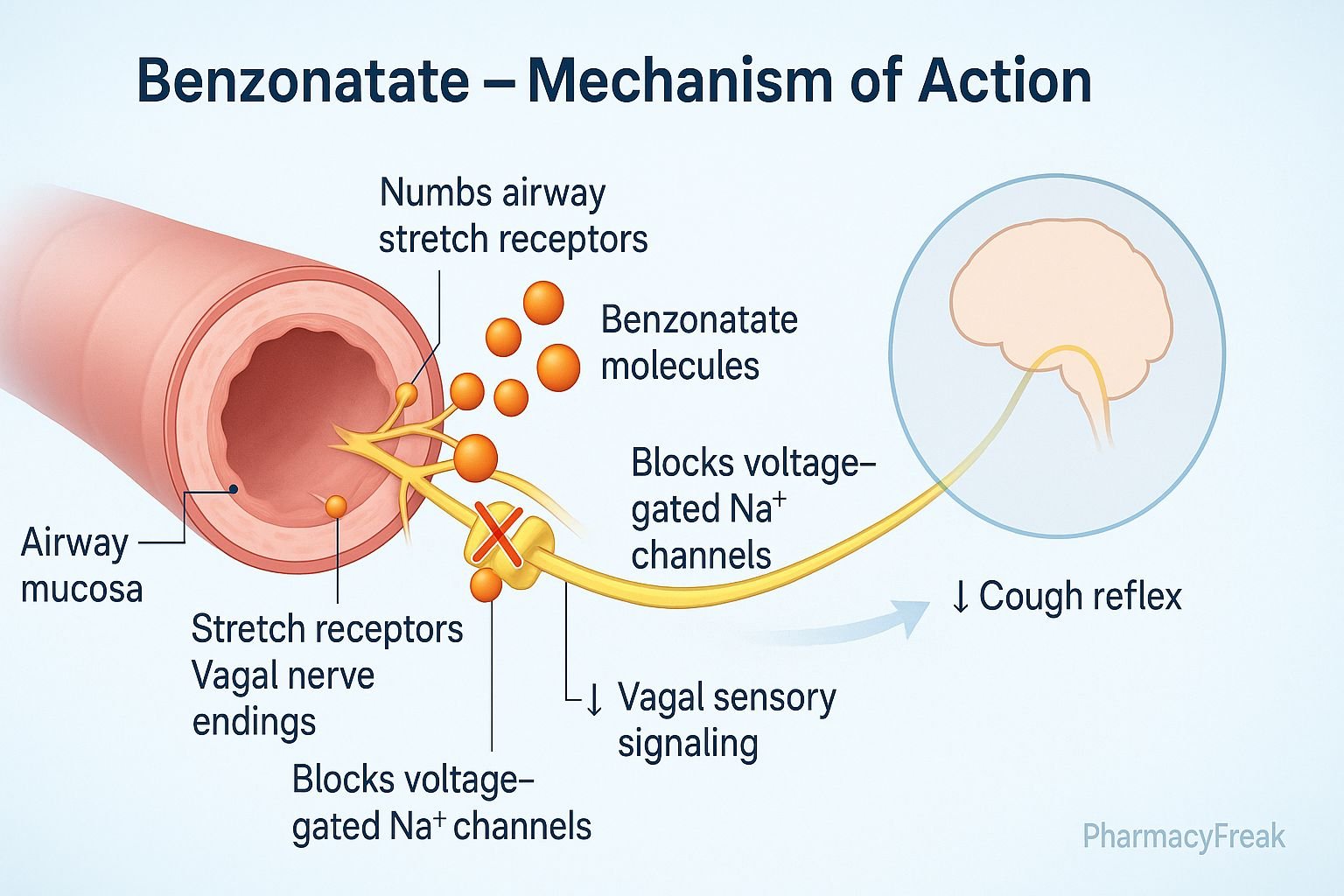
Channel Blockers: These drugs block the flow of ions through specific channels.
Channel Openers: These drugs increase the likelihood that a channel is open.
Examples
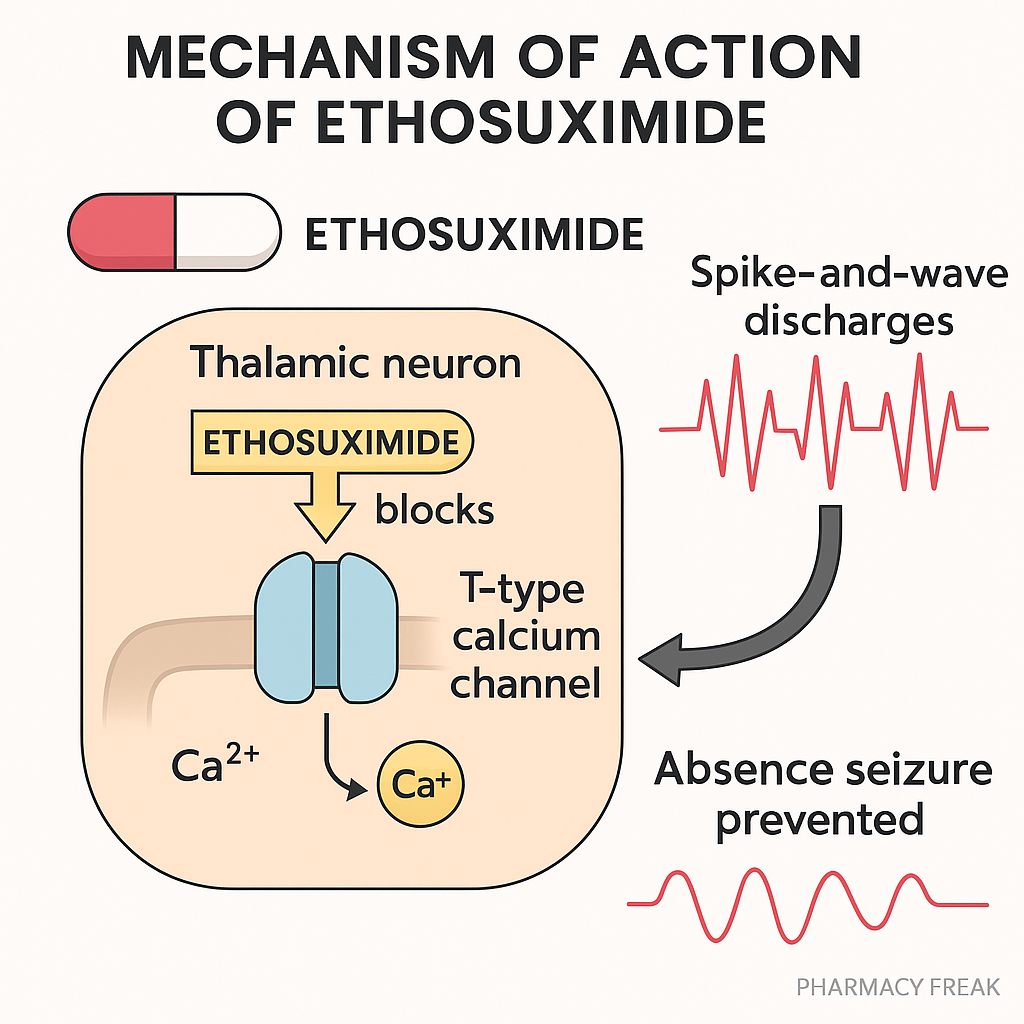
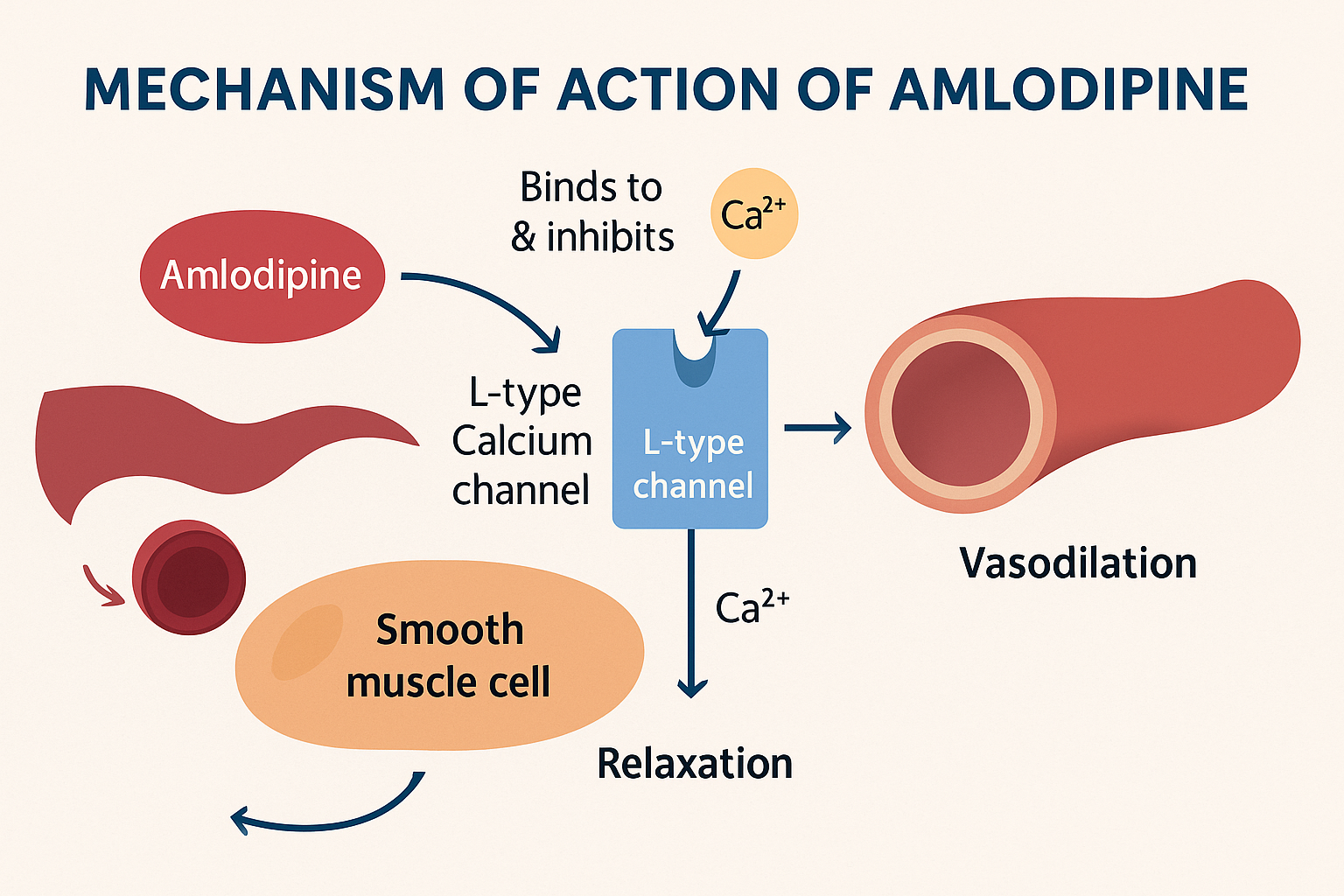
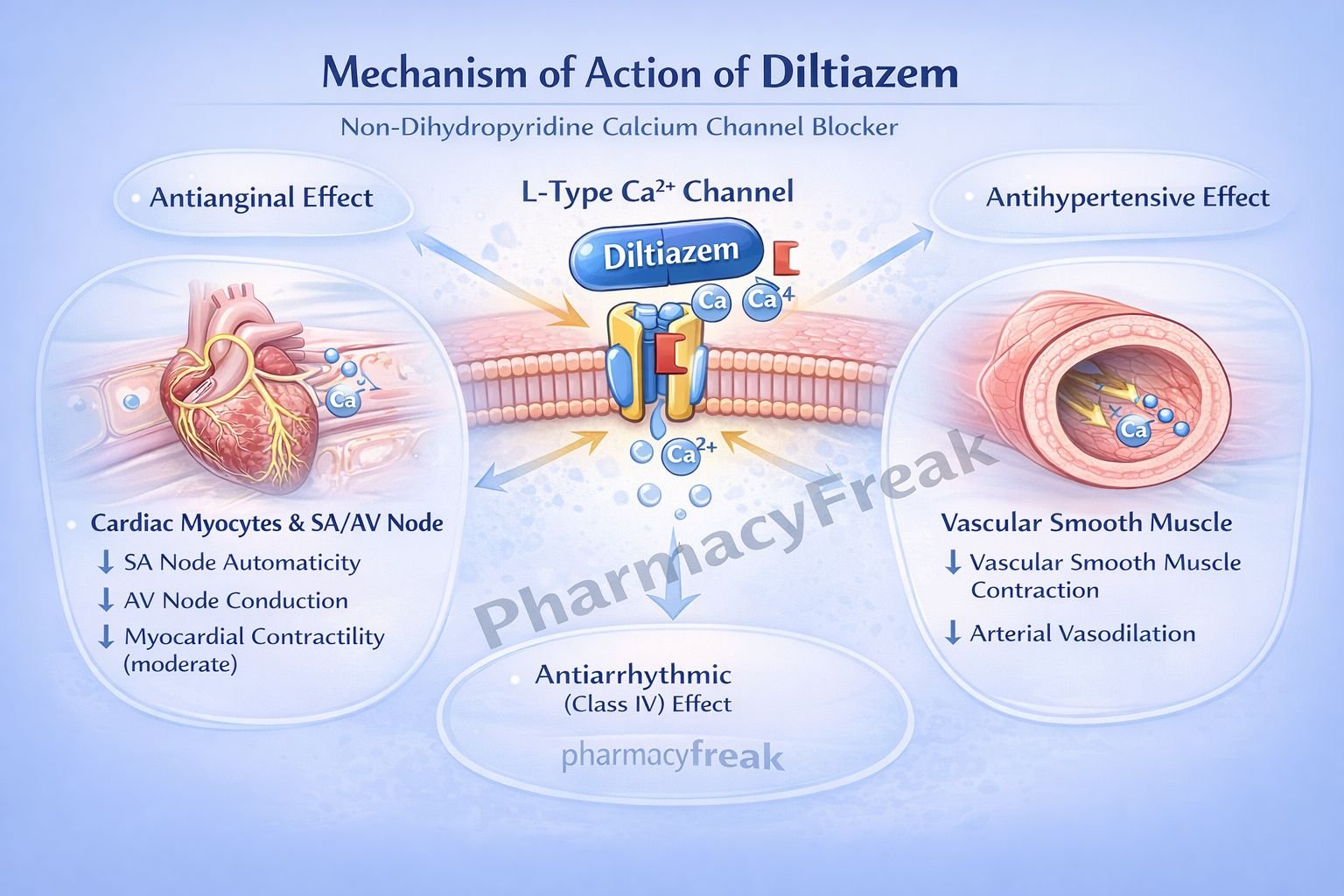
Calcium Channel Blockers (e.g., amlodipine): Block calcium entry into muscle cells of the heart and blood vessels, causing relaxation and lowering blood pressure.
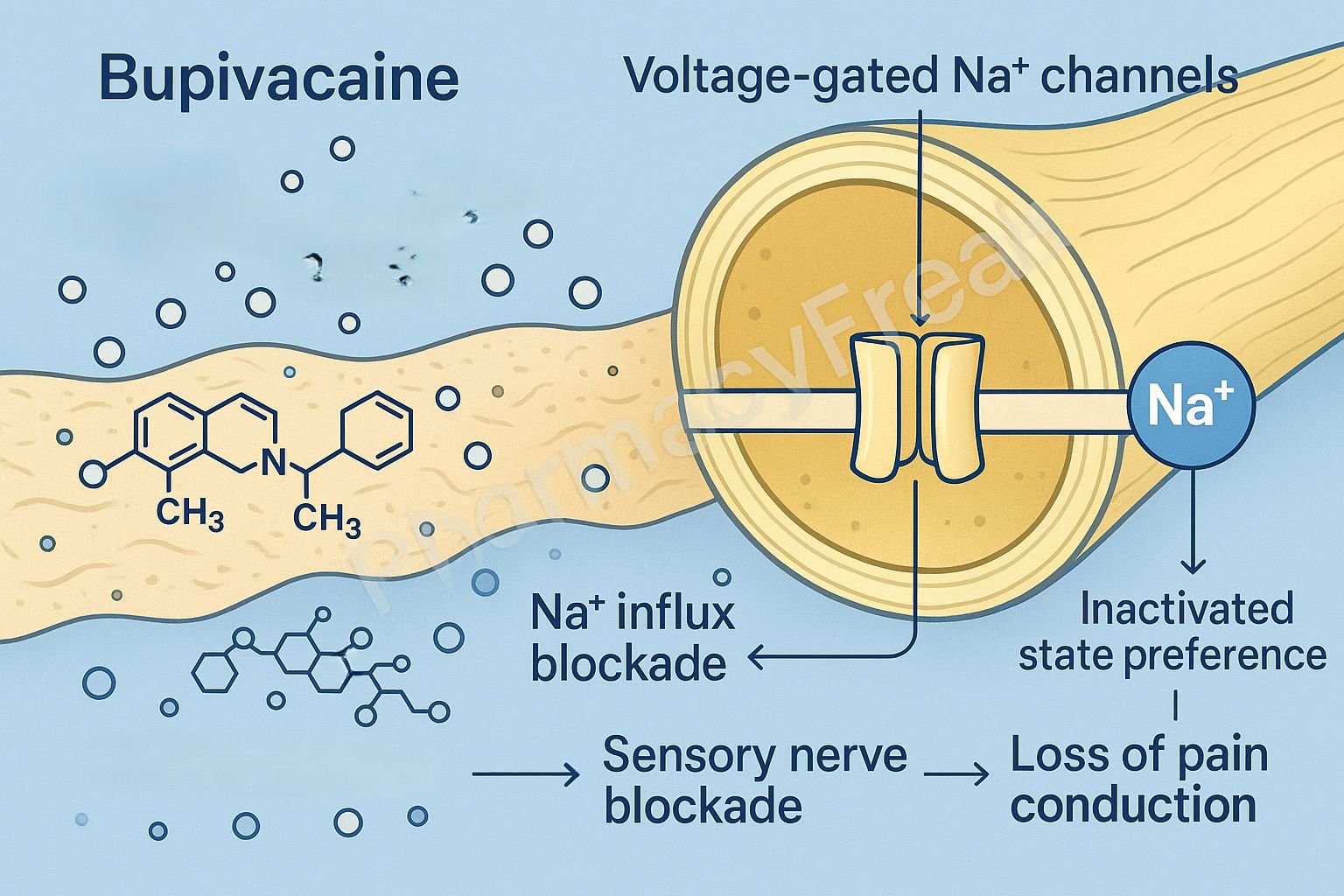
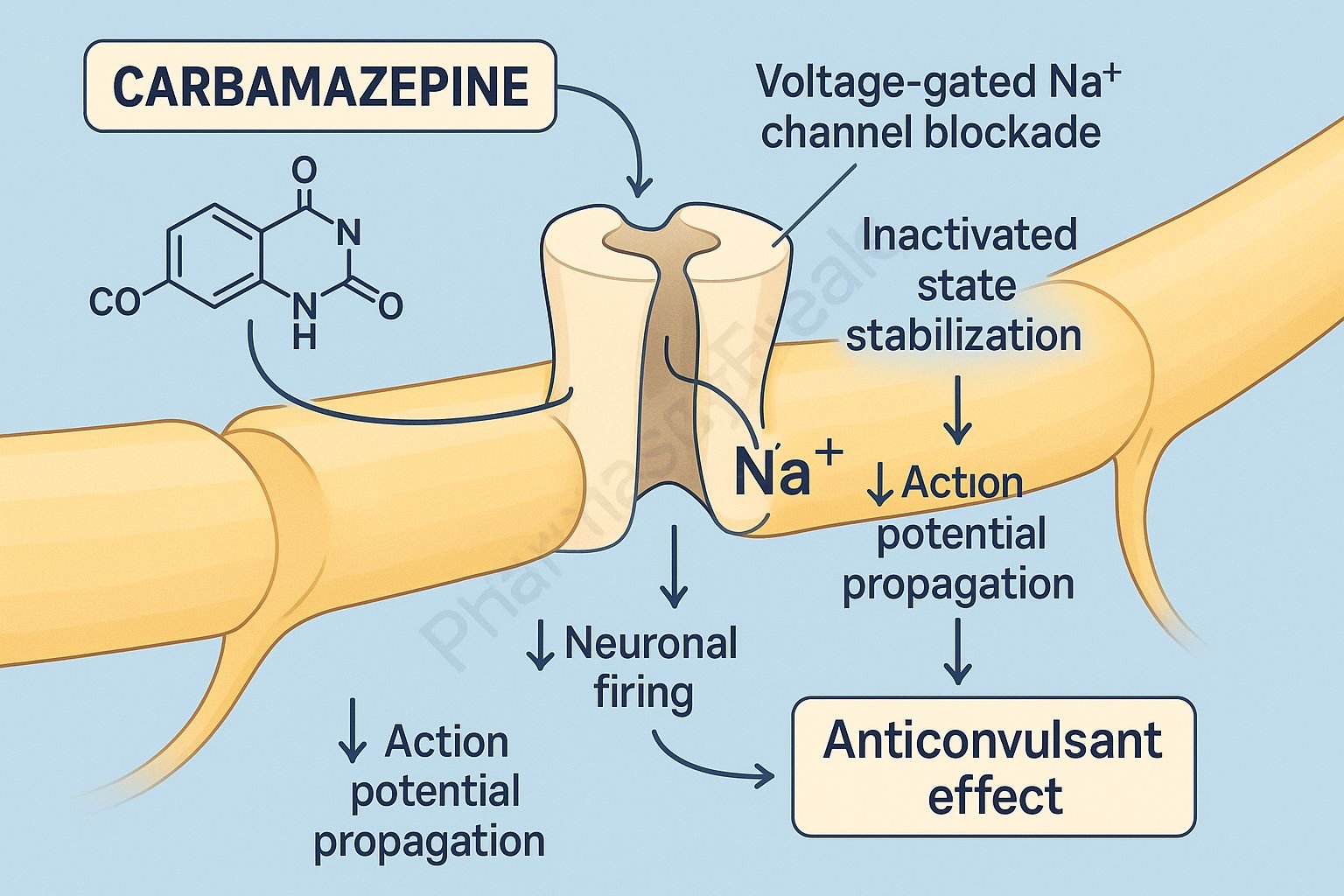
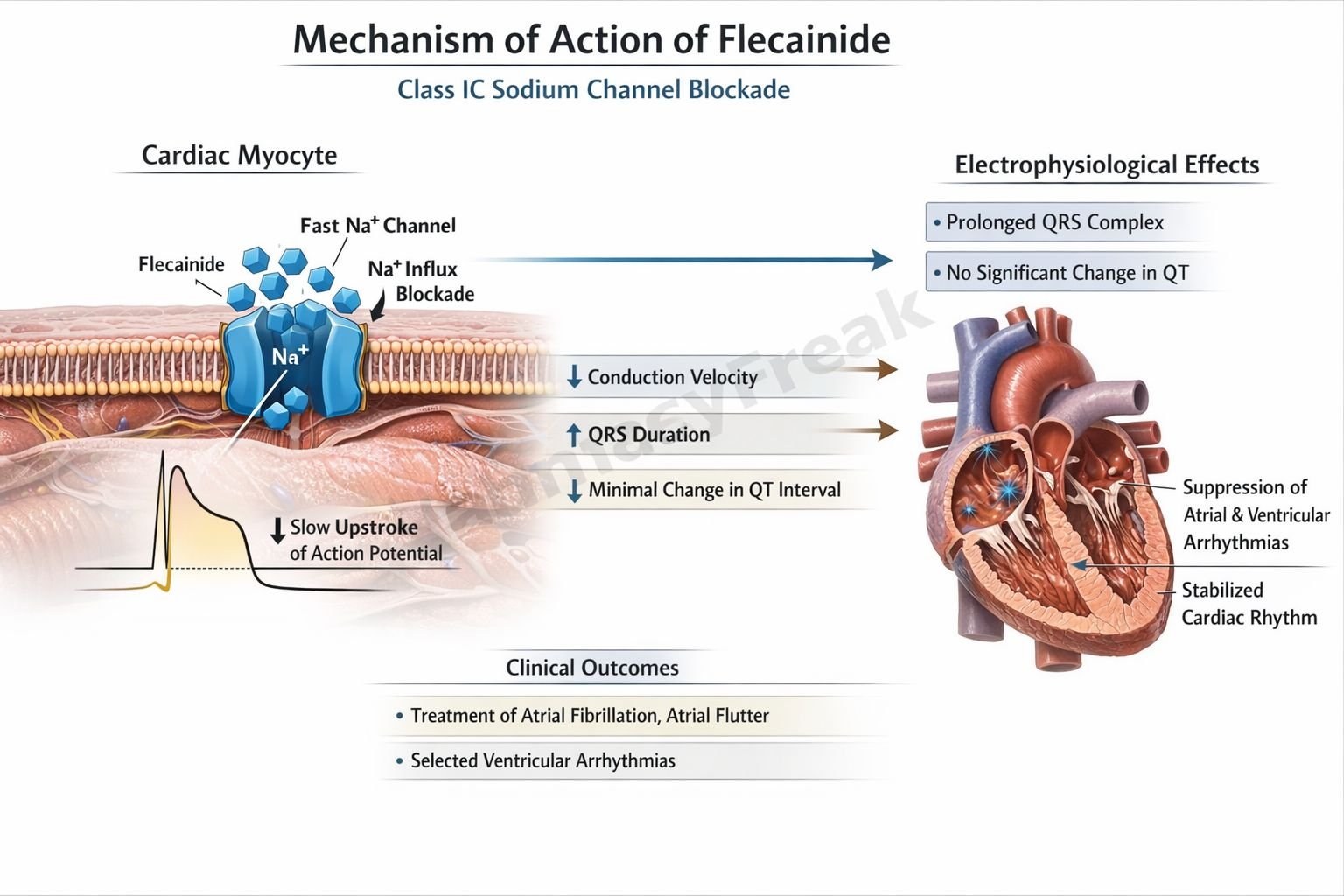
Sodium Channel Blockers (e.g., lidocaine): Used as local anesthetics and antiarrhythmics, they prevent the initiation and transmission of nerve impulses.
Potassium Channel Openers (e.g., minoxidil): Cause hyperpolarization of cell membranes, leading to vasodilation.
Clinical Relevance
Drugs targeting ion channels are crucial in managing cardiac arrhythmias, epilepsy, hypertension, and pain. Understanding which channel a drug affects helps anticipate both benefits and risks.
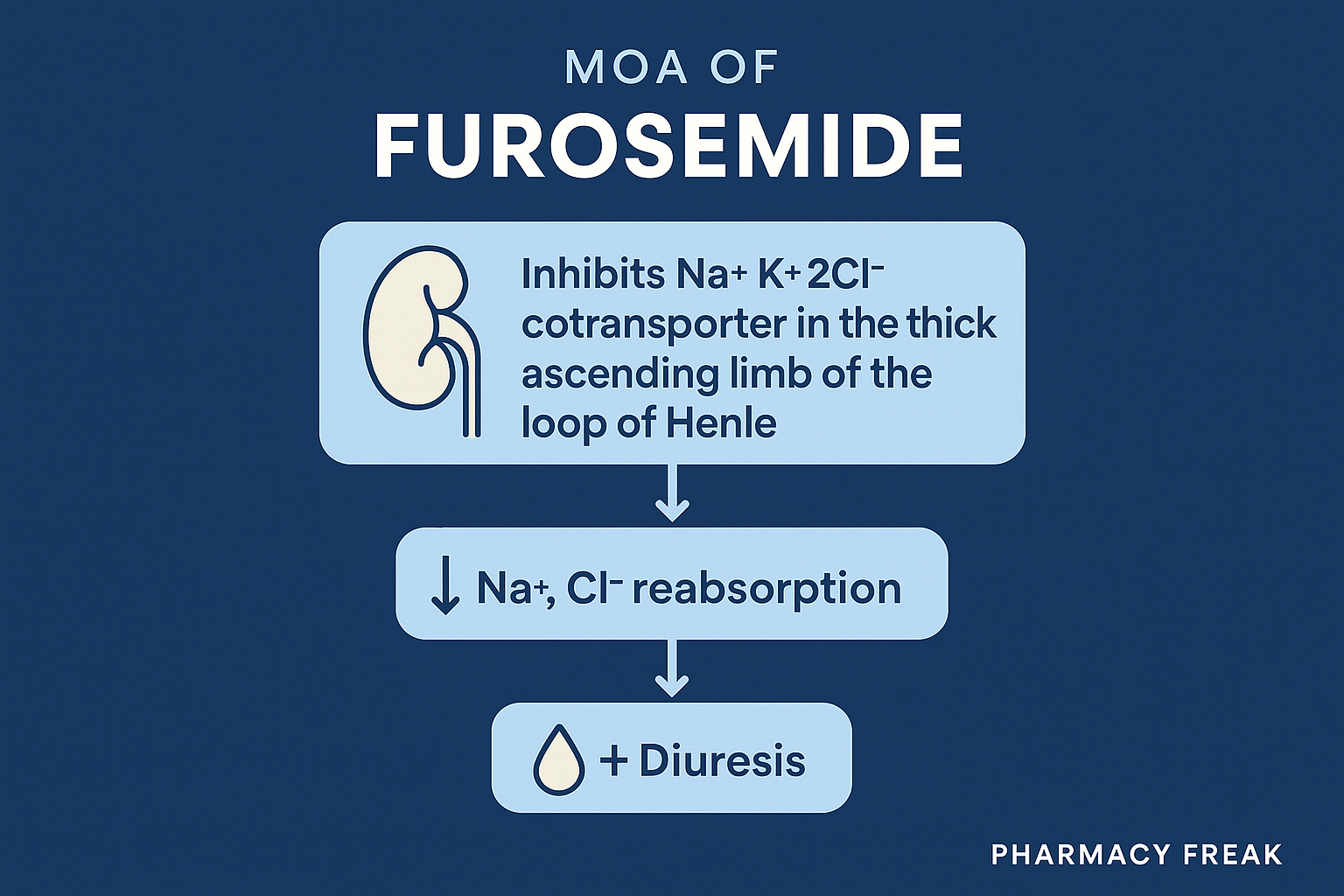
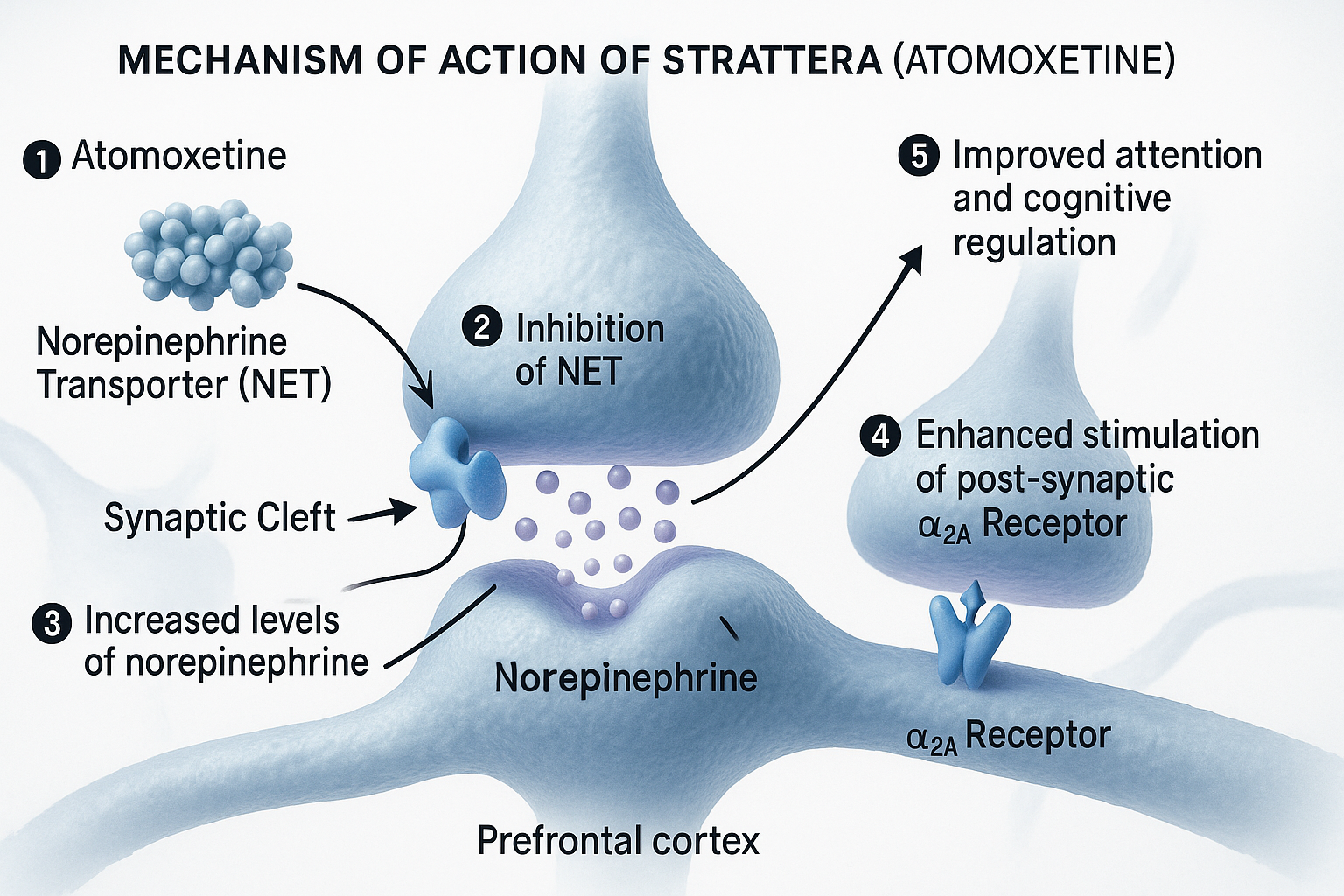
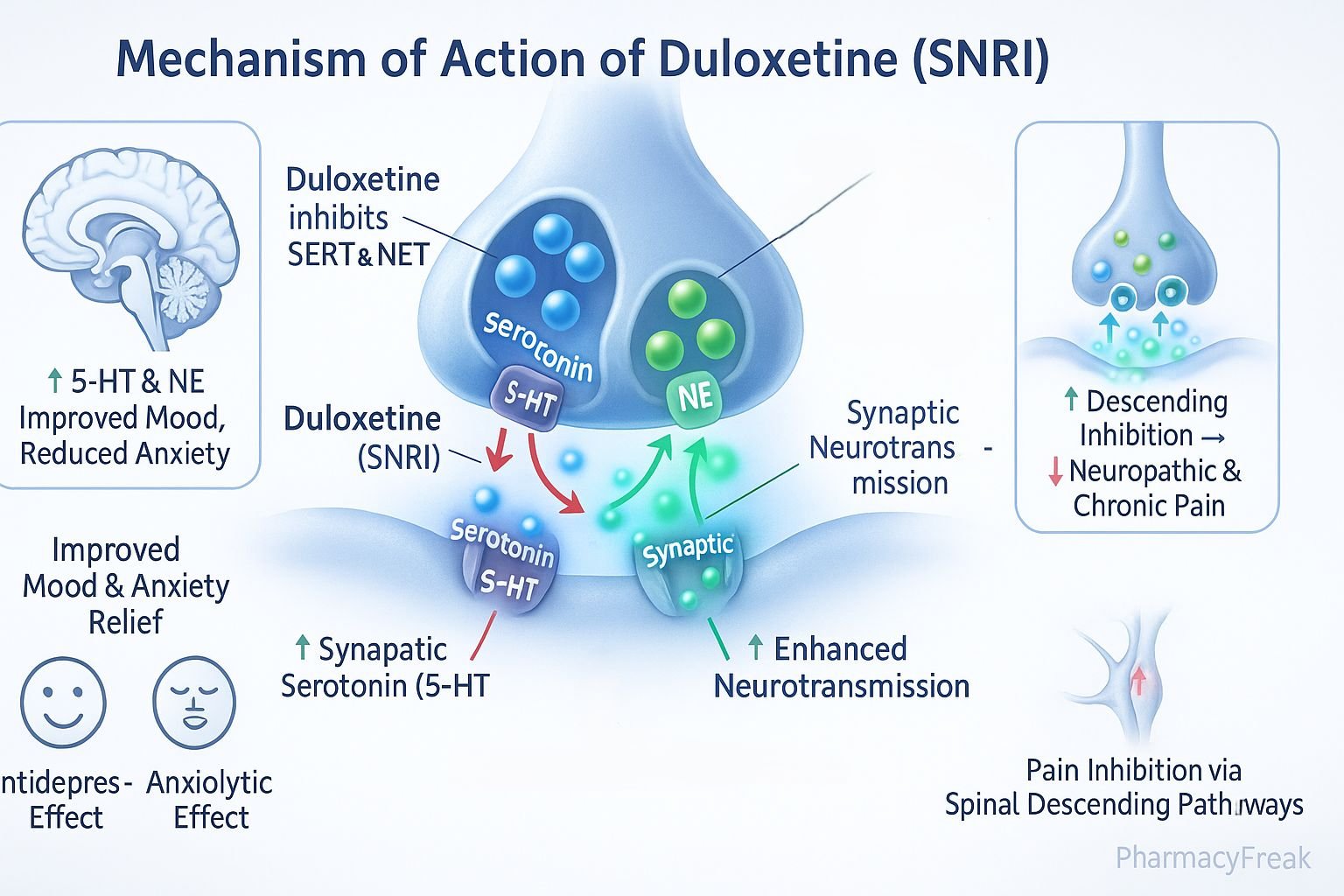
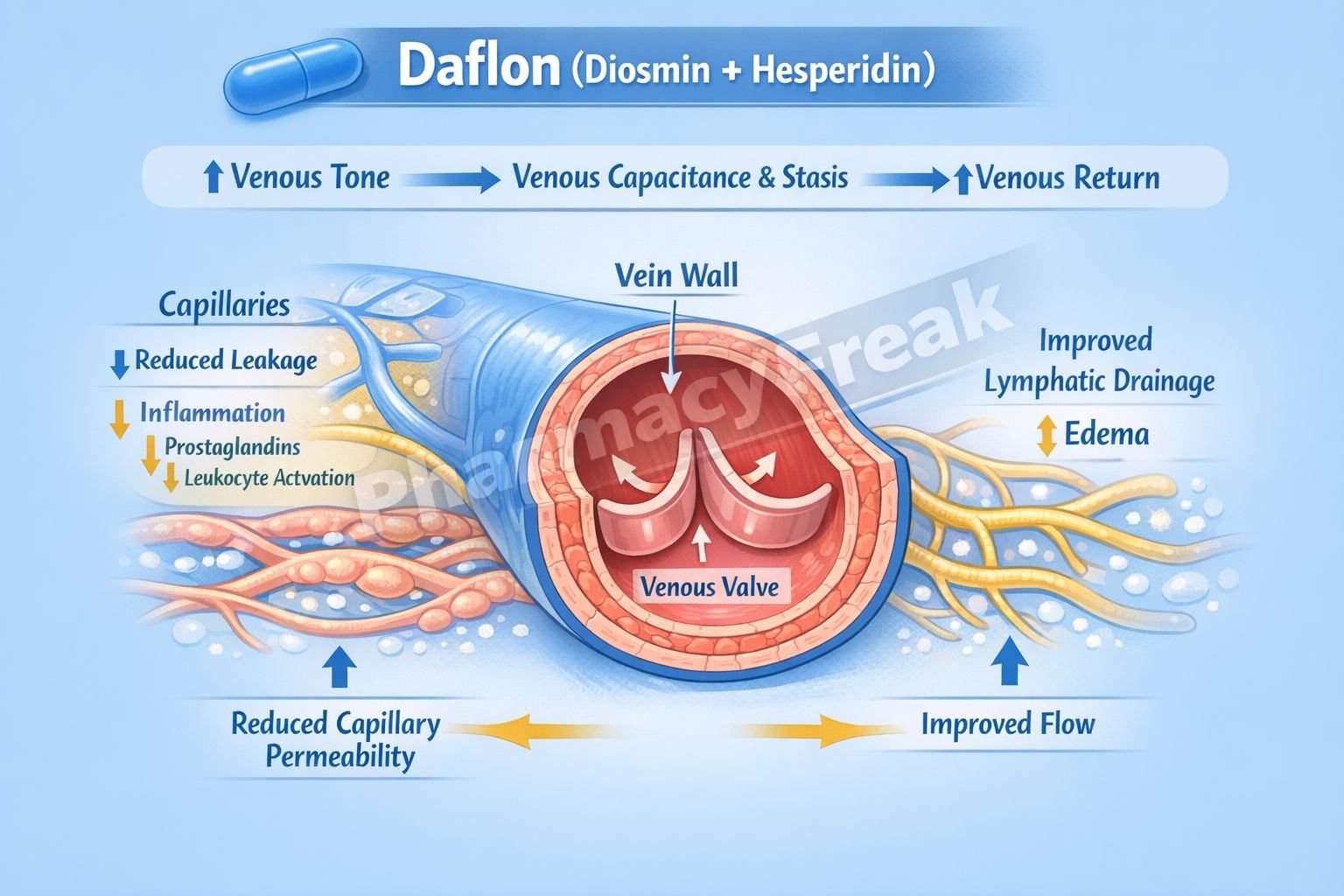
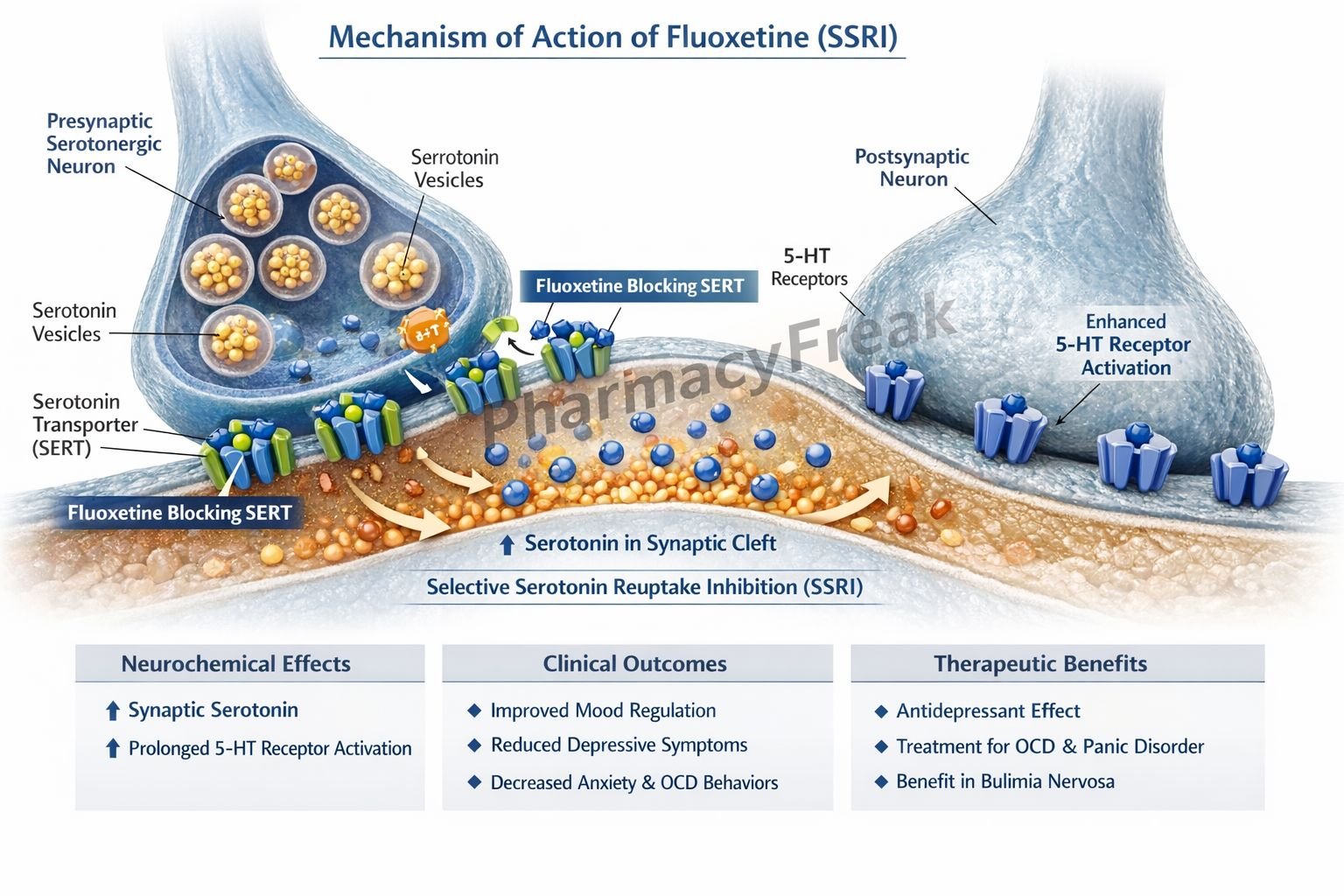
4. Transporters: Moving Molecules Across Membranes
What Are Transporters?
Transporters are proteins in cell membranes that move substances such as ions, nutrients, or neurotransmitters across the cell membrane.
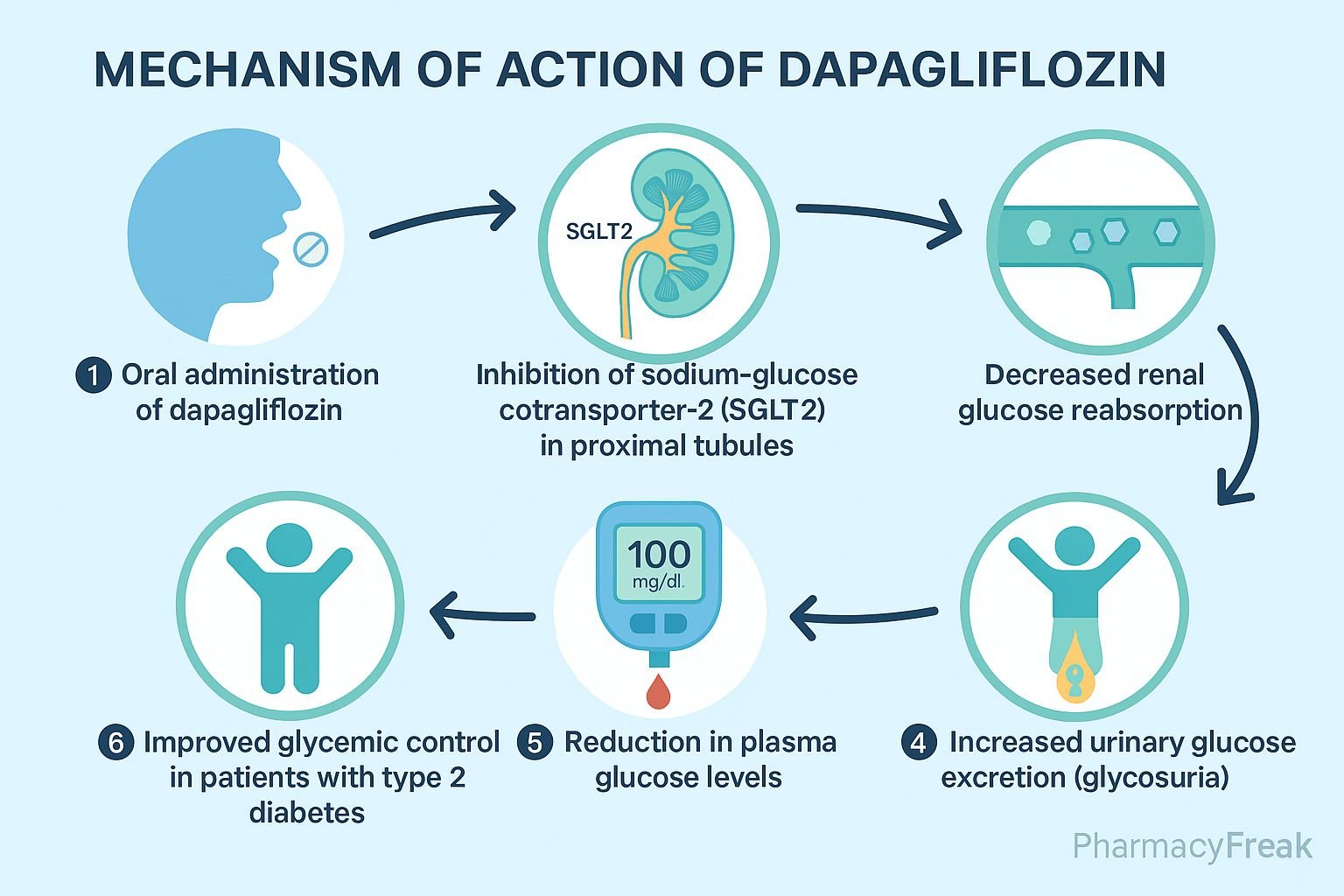
How Drugs Affect Transporters
Inhibitors: Drugs can block transporters, increasing the levels of specific substances outside cells.
Enhancers: Some drugs increase transporter activity, but these are less common.
Examples
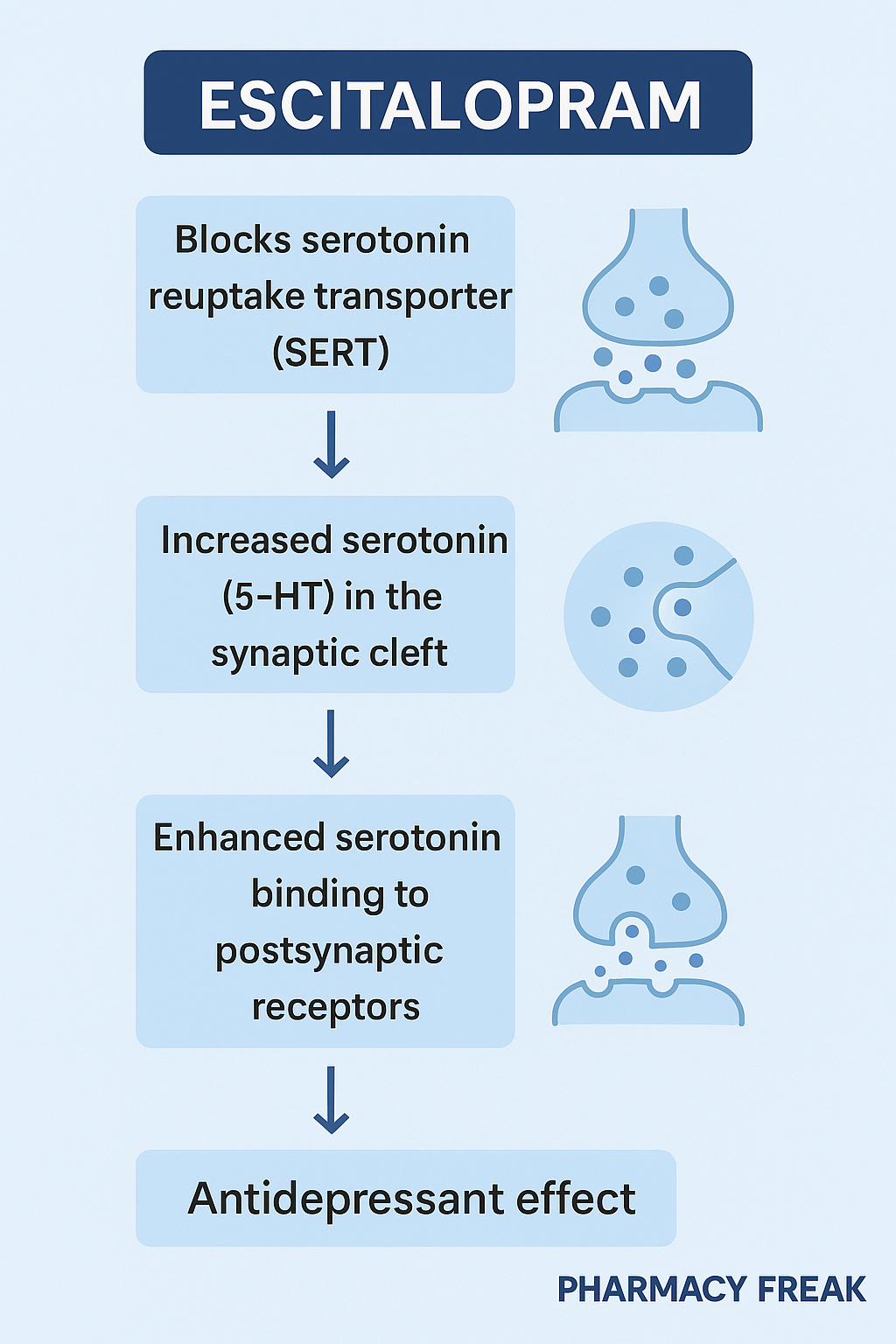
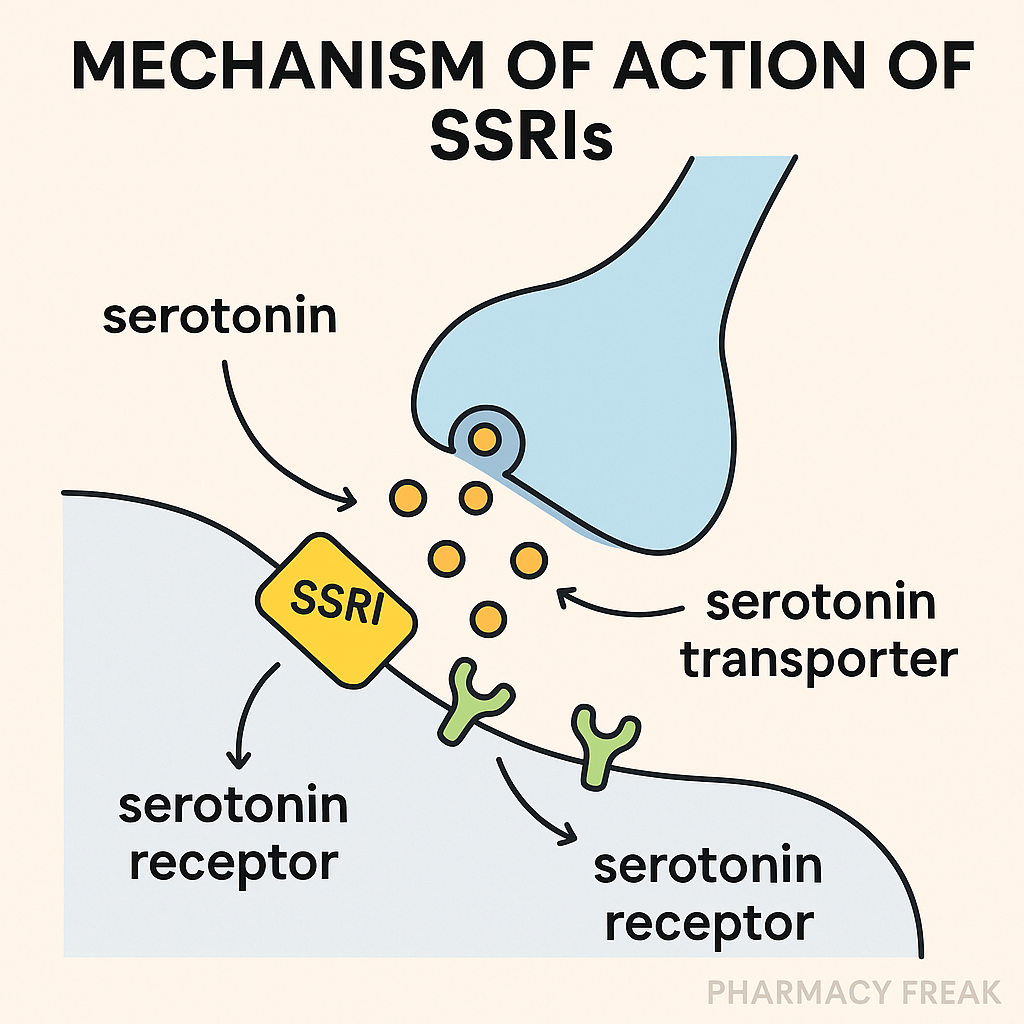
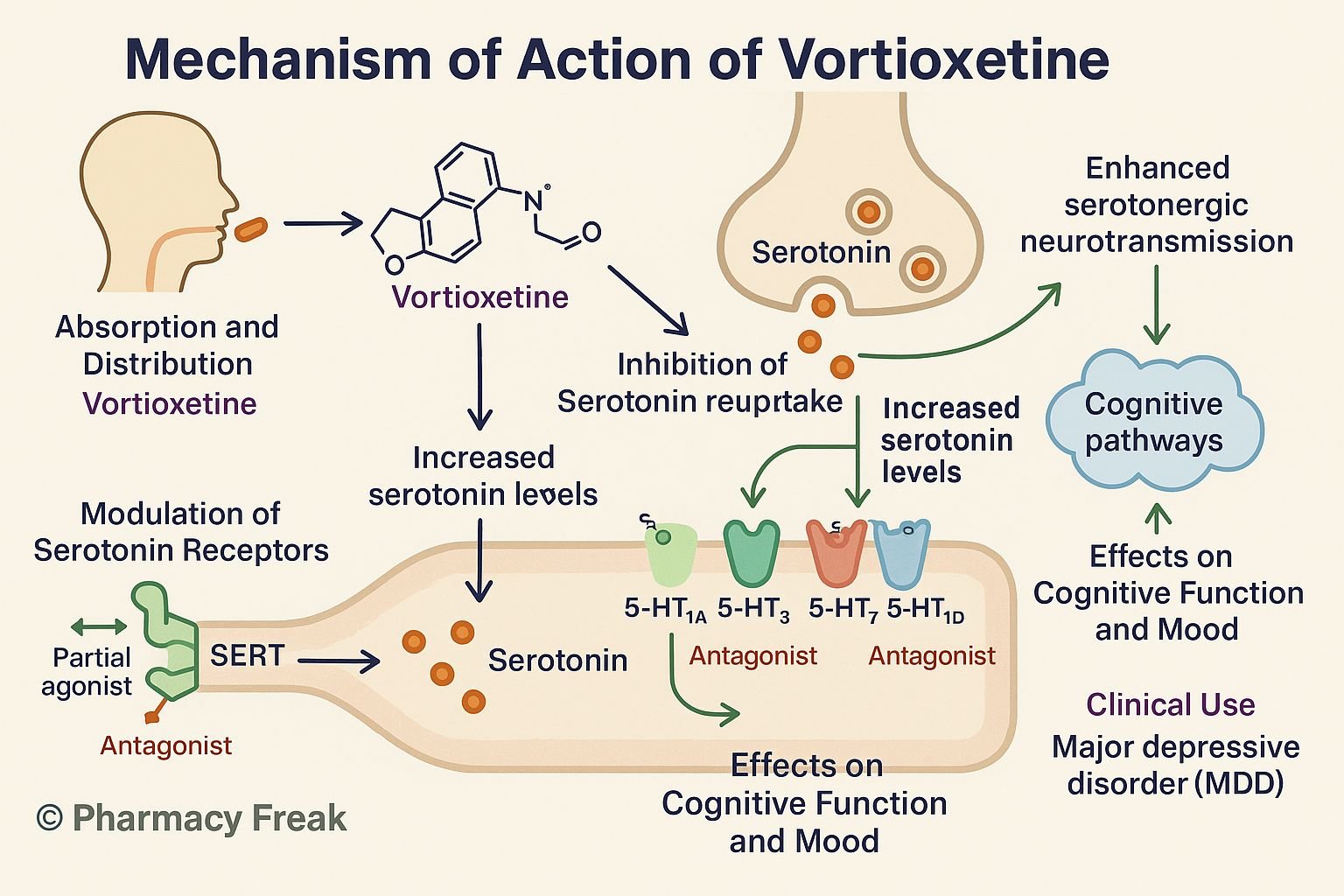
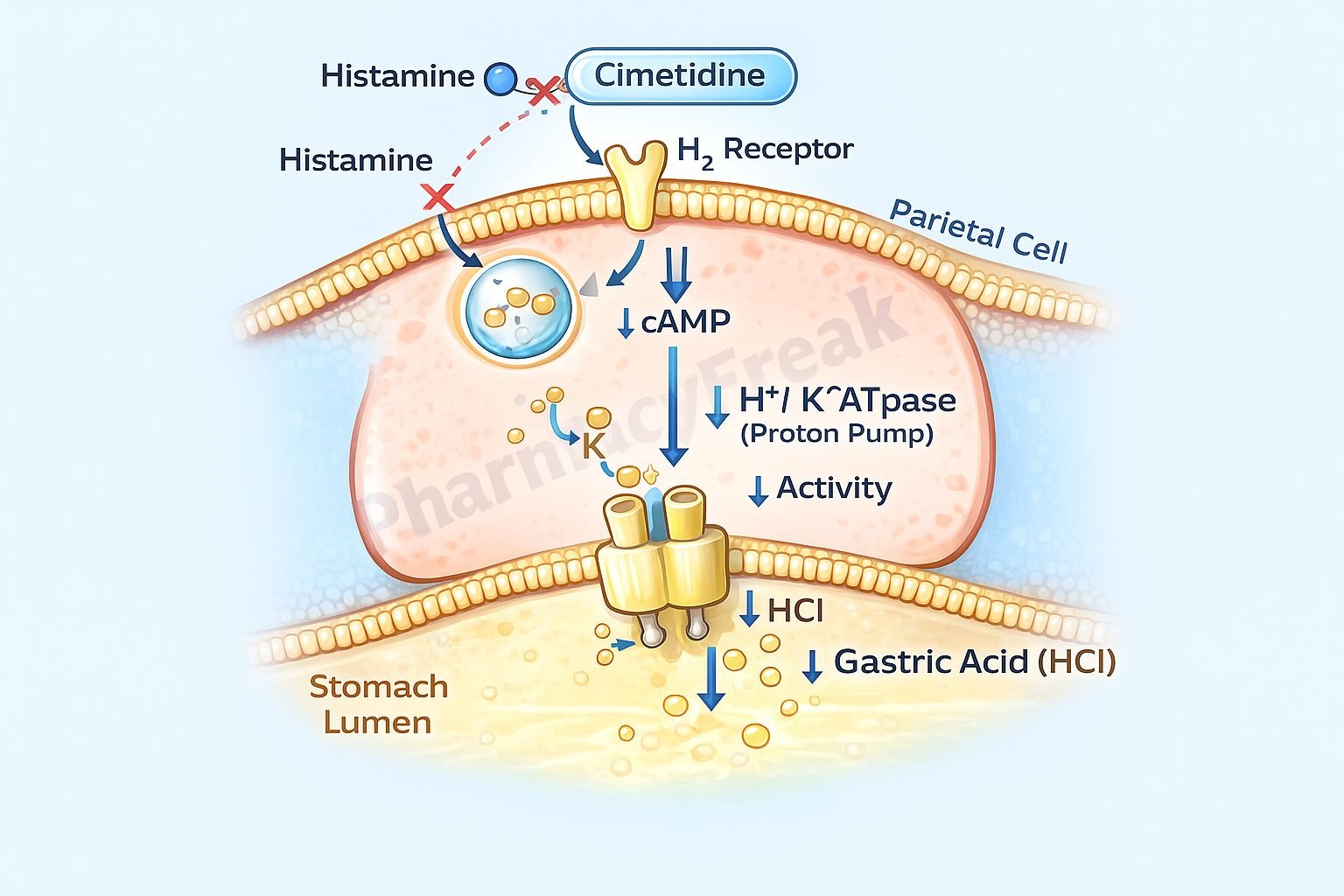
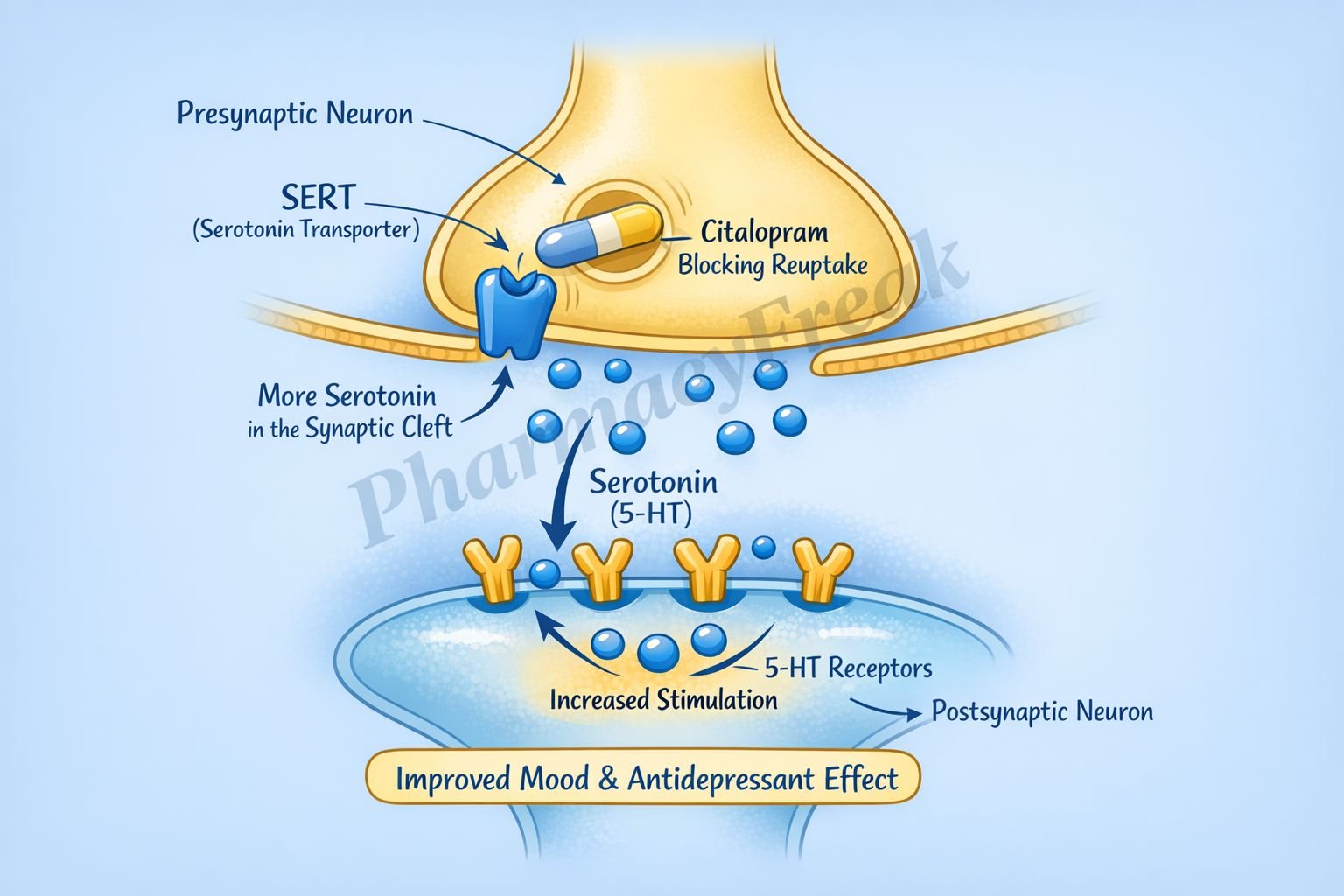
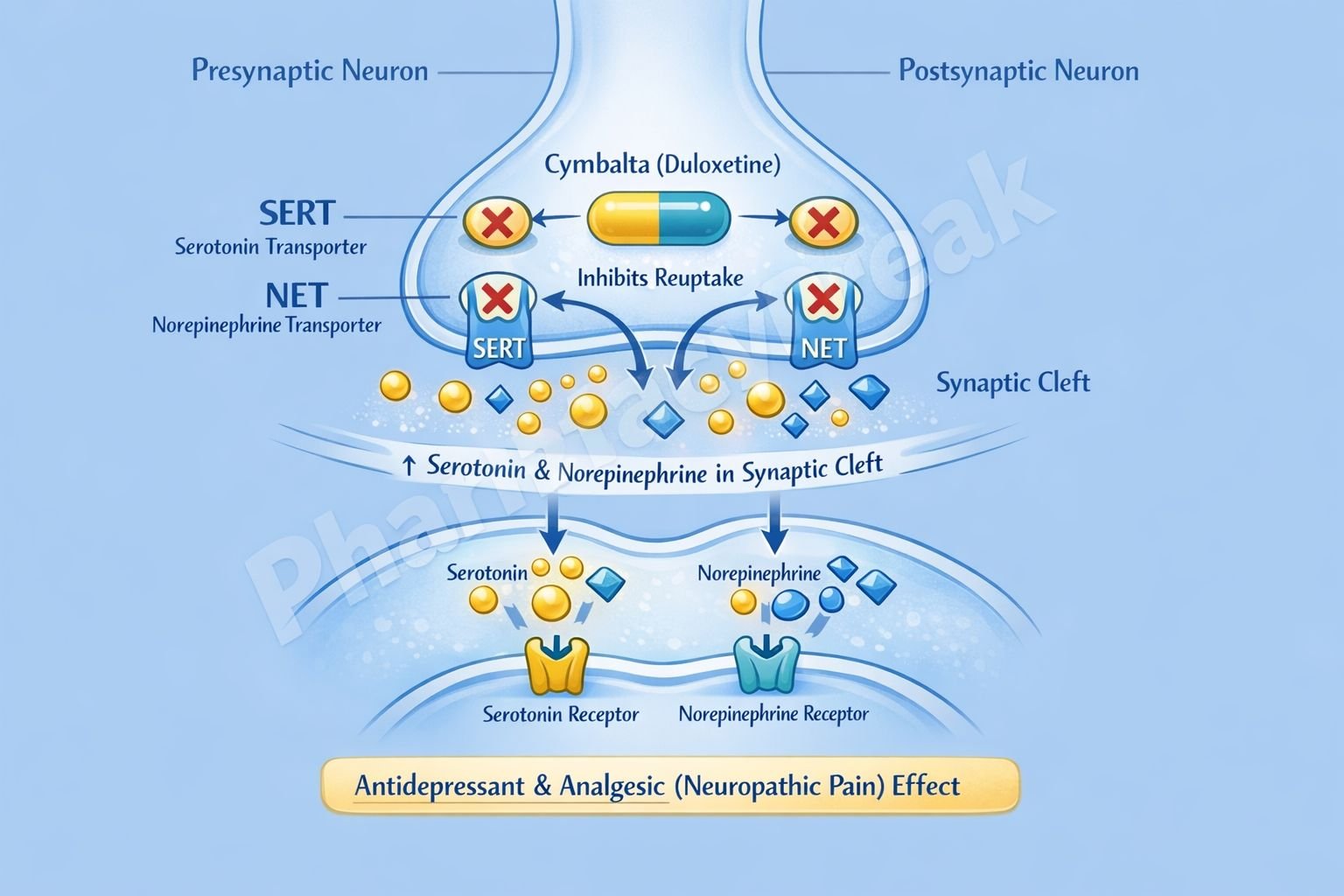
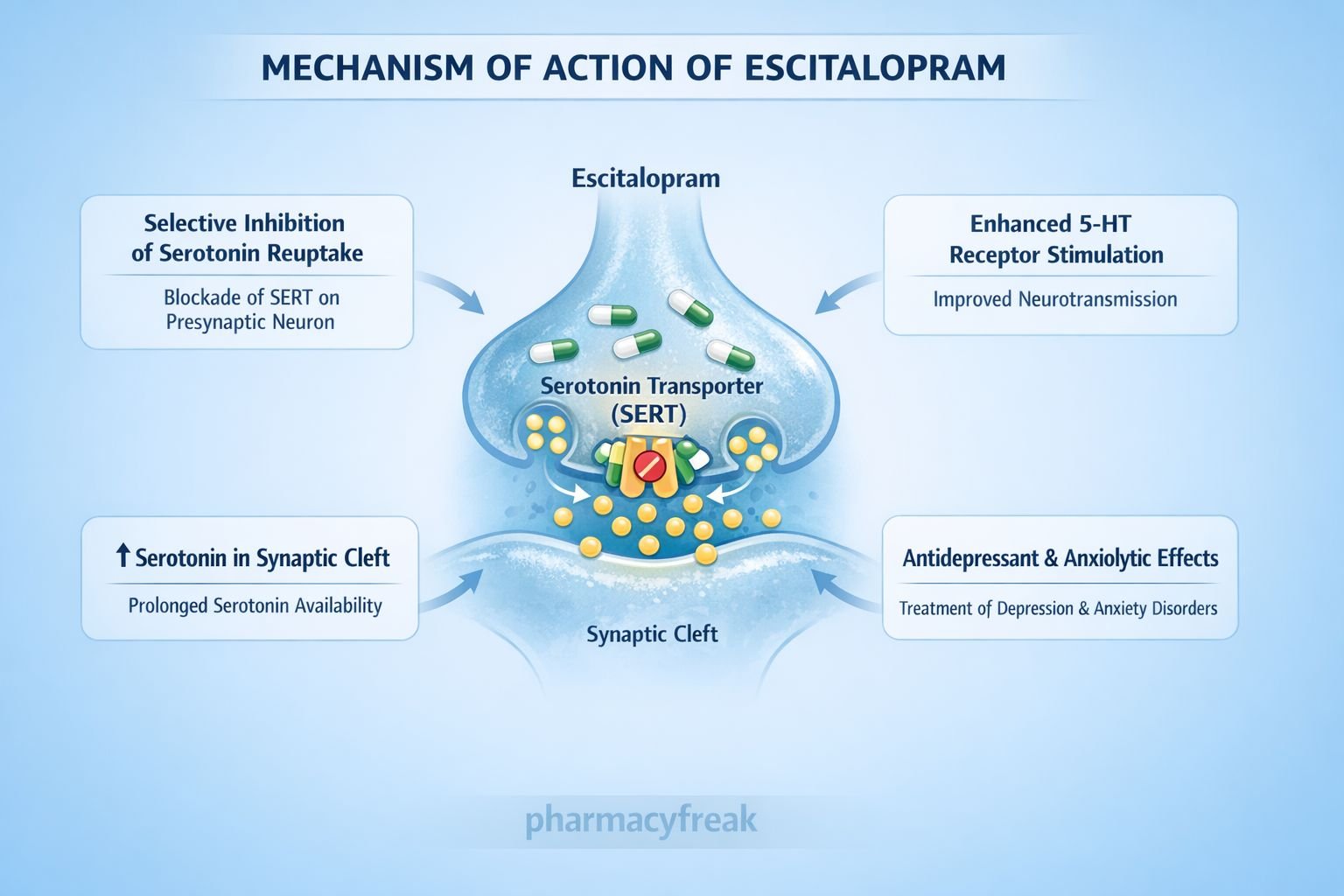
Selective Serotonin Reuptake Inhibitors (SSRIs, e.g., fluoxetine): Block the reuptake of serotonin into nerve terminals, increasing serotonin in the synaptic cleft, used in depression and anxiety disorders.
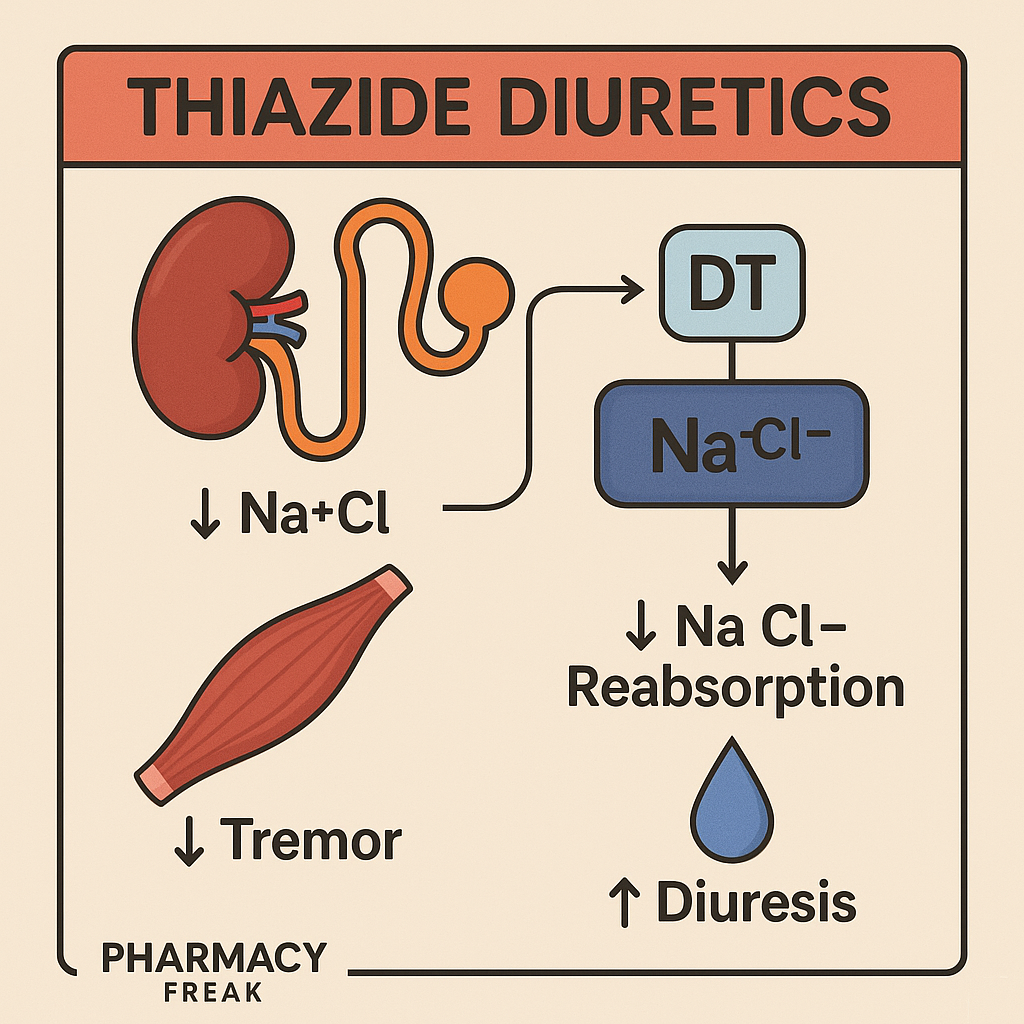
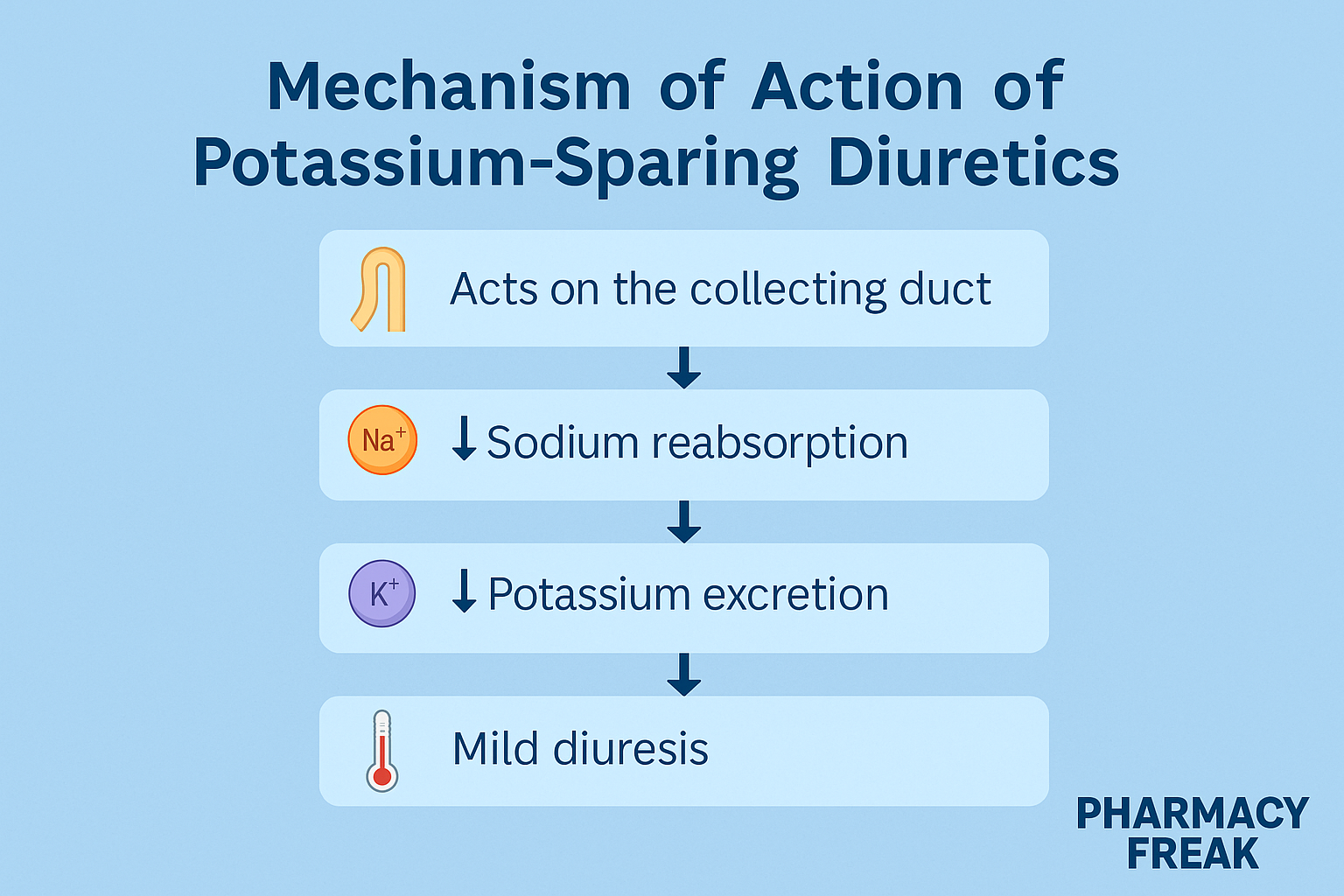
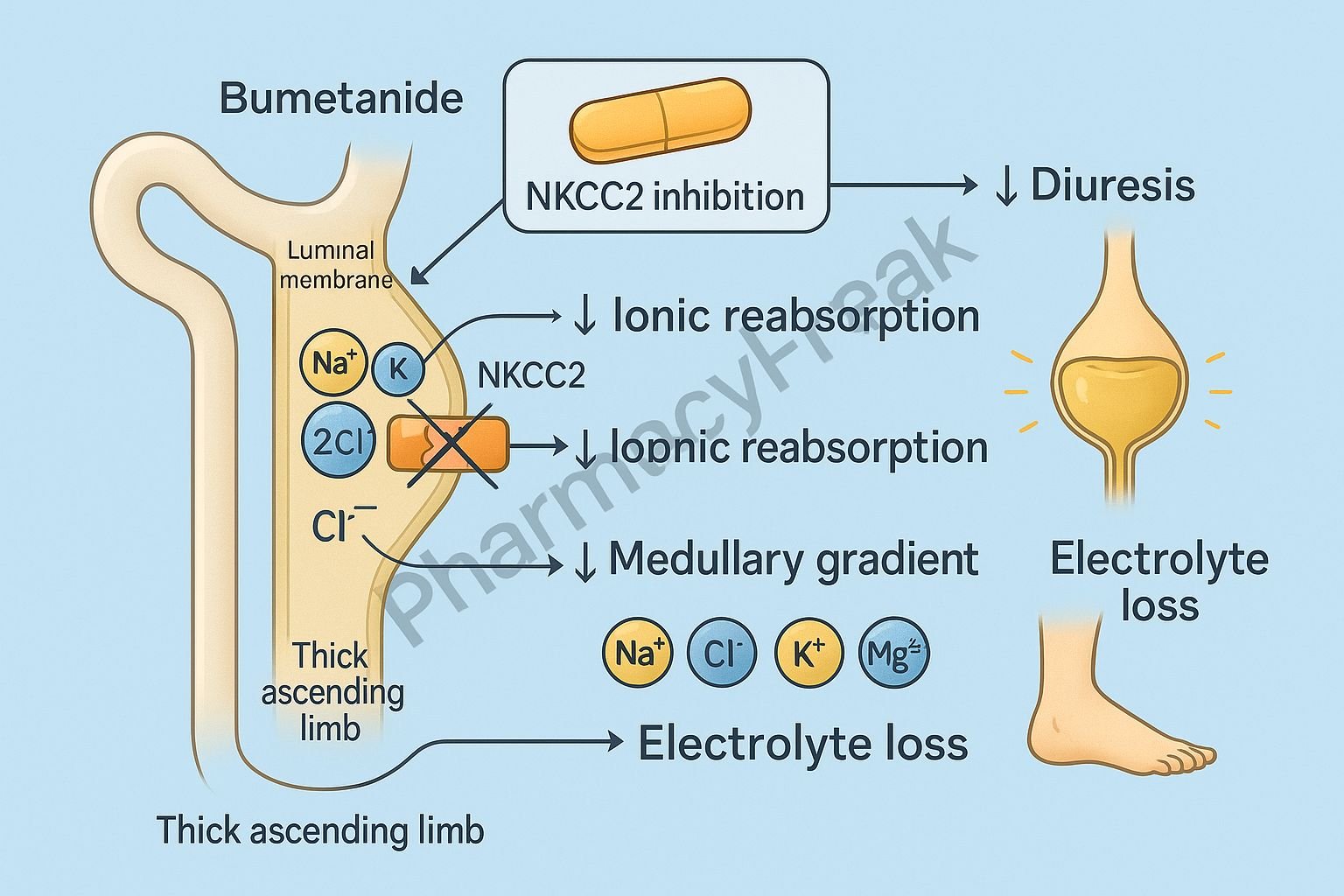
Loop Diuretics (e.g., furosemide): Inhibit sodium-potassium-chloride cotransporters in the kidney, increasing urine output.
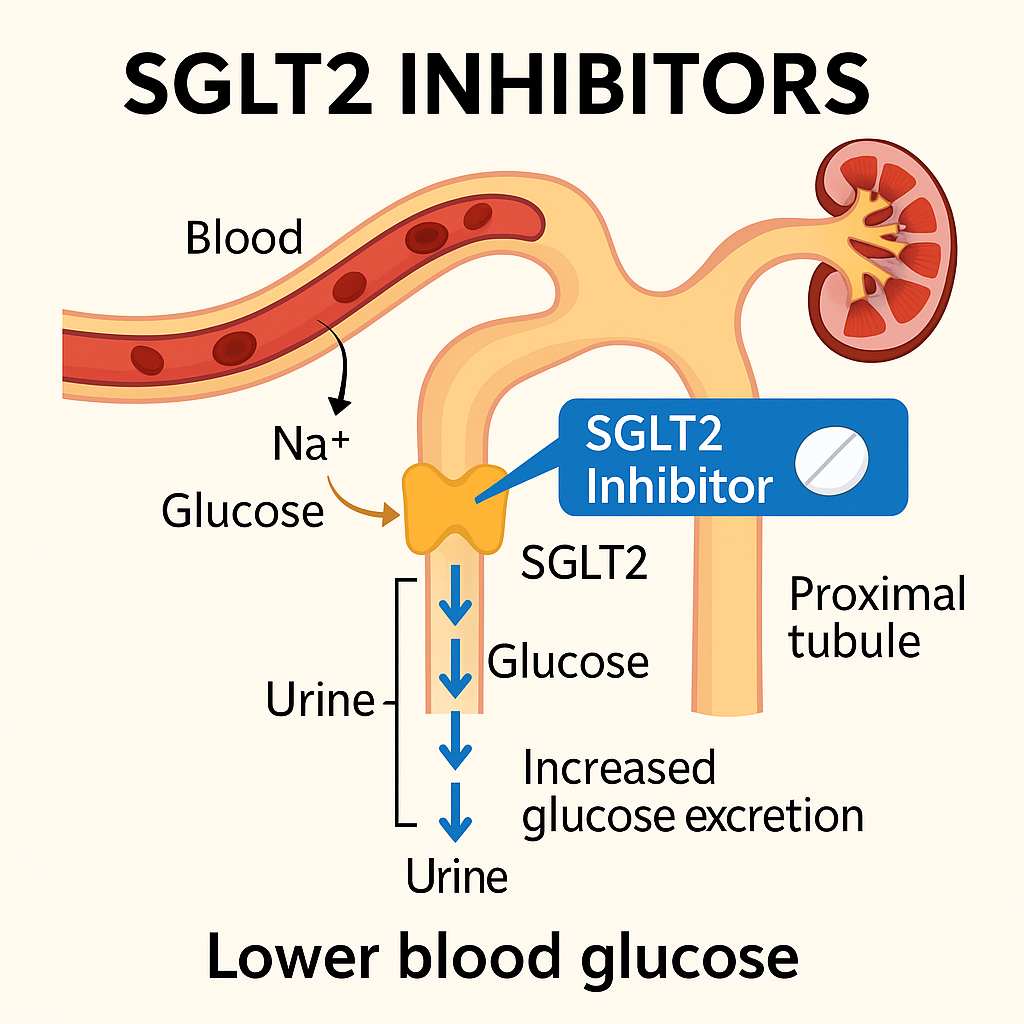
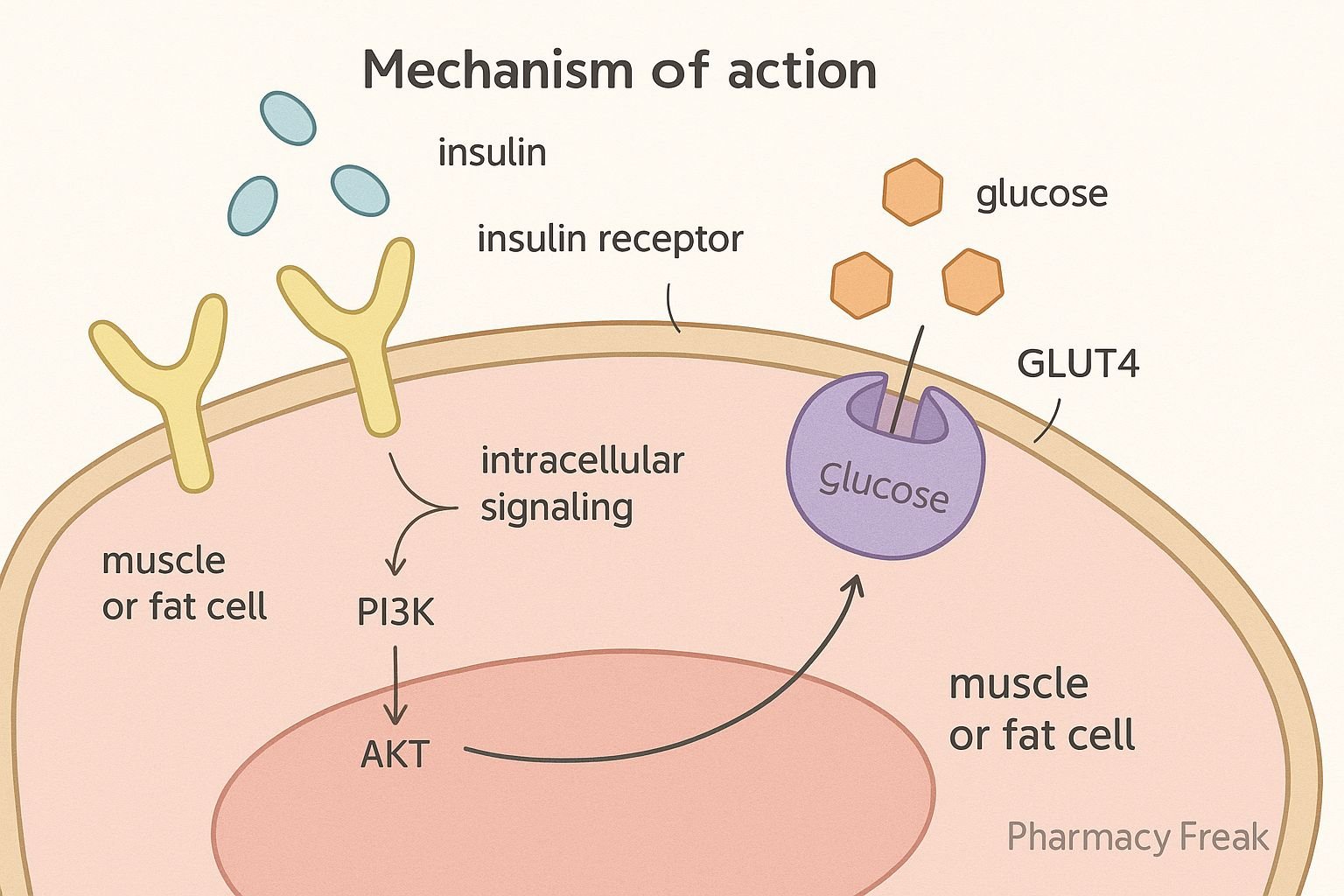
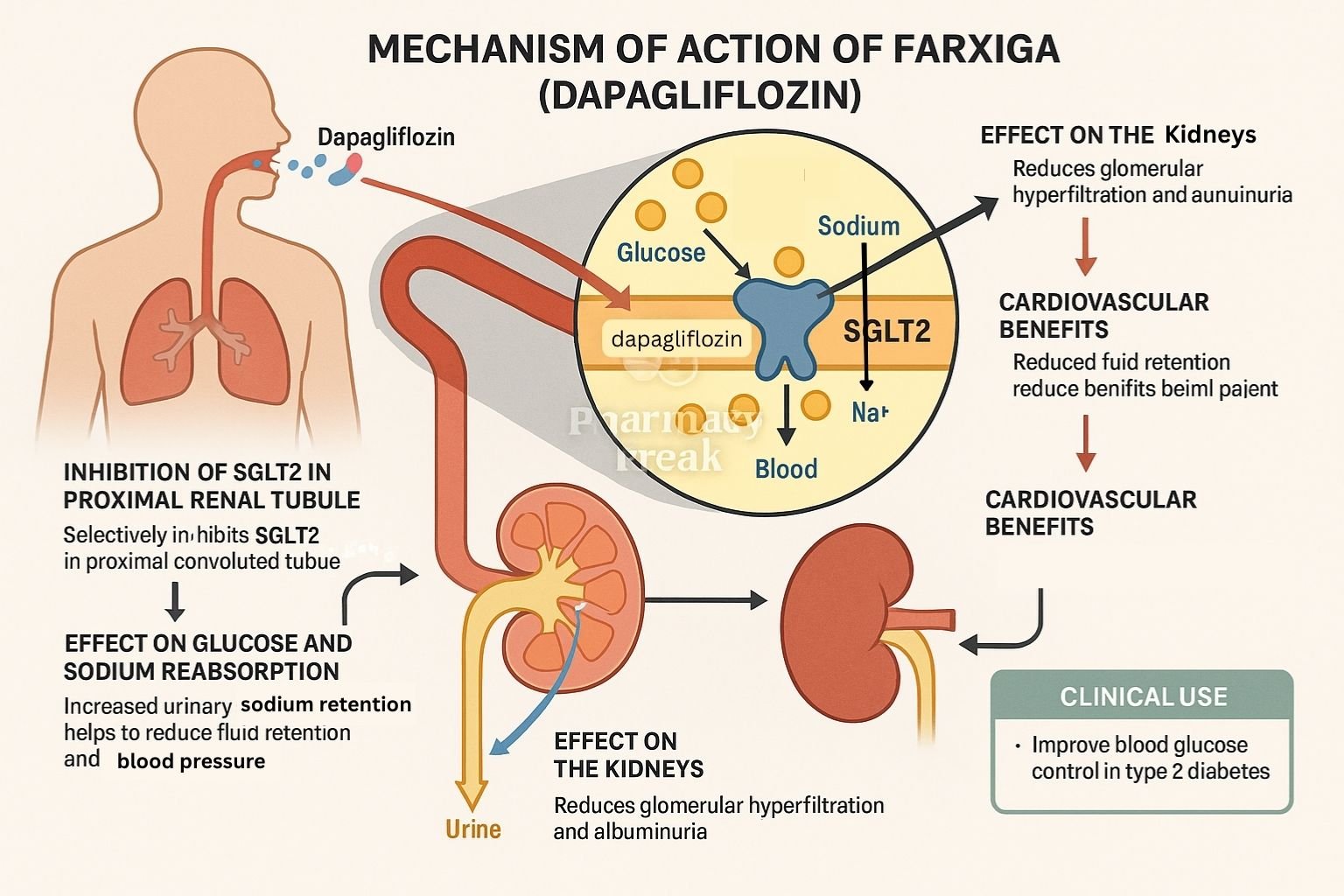
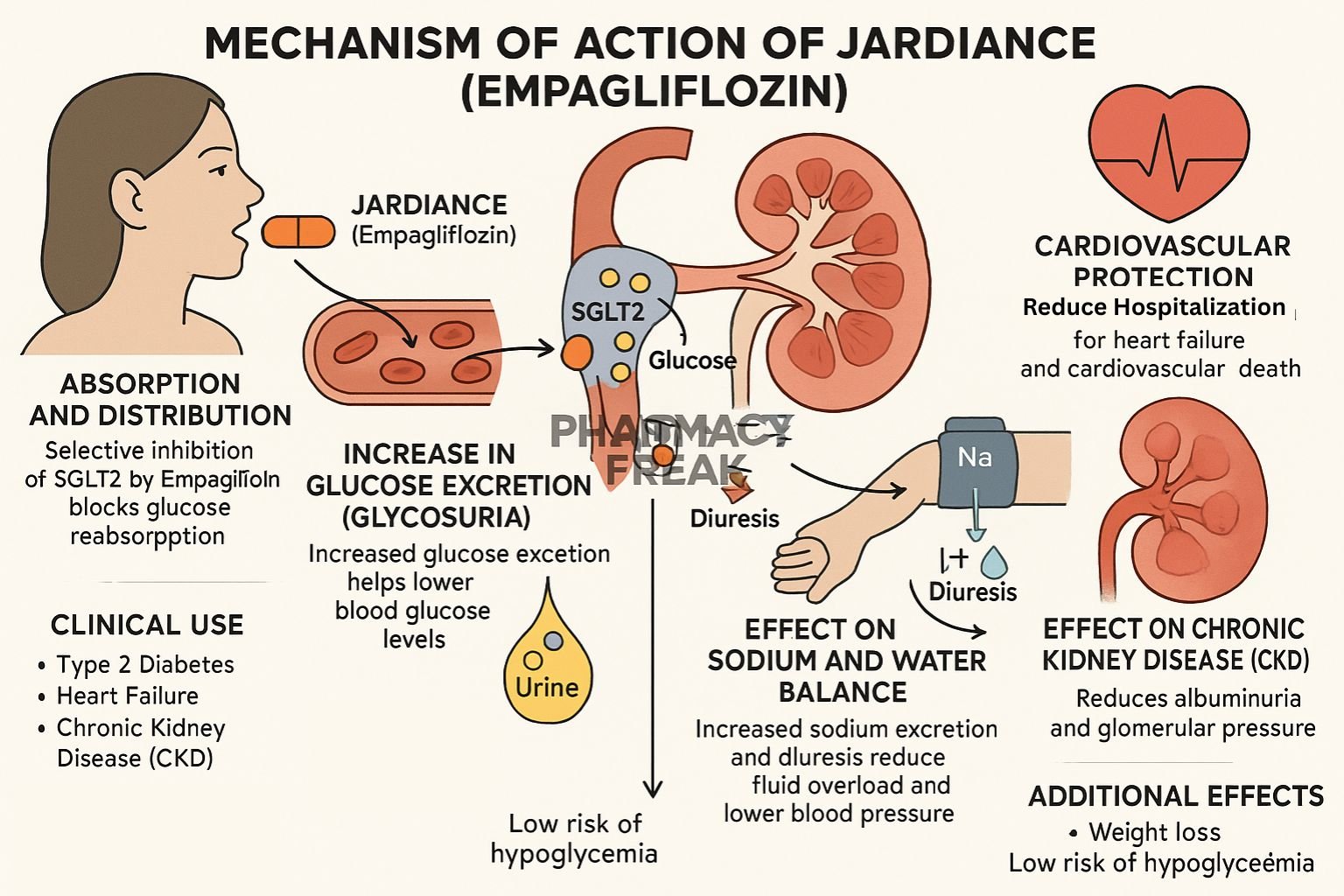
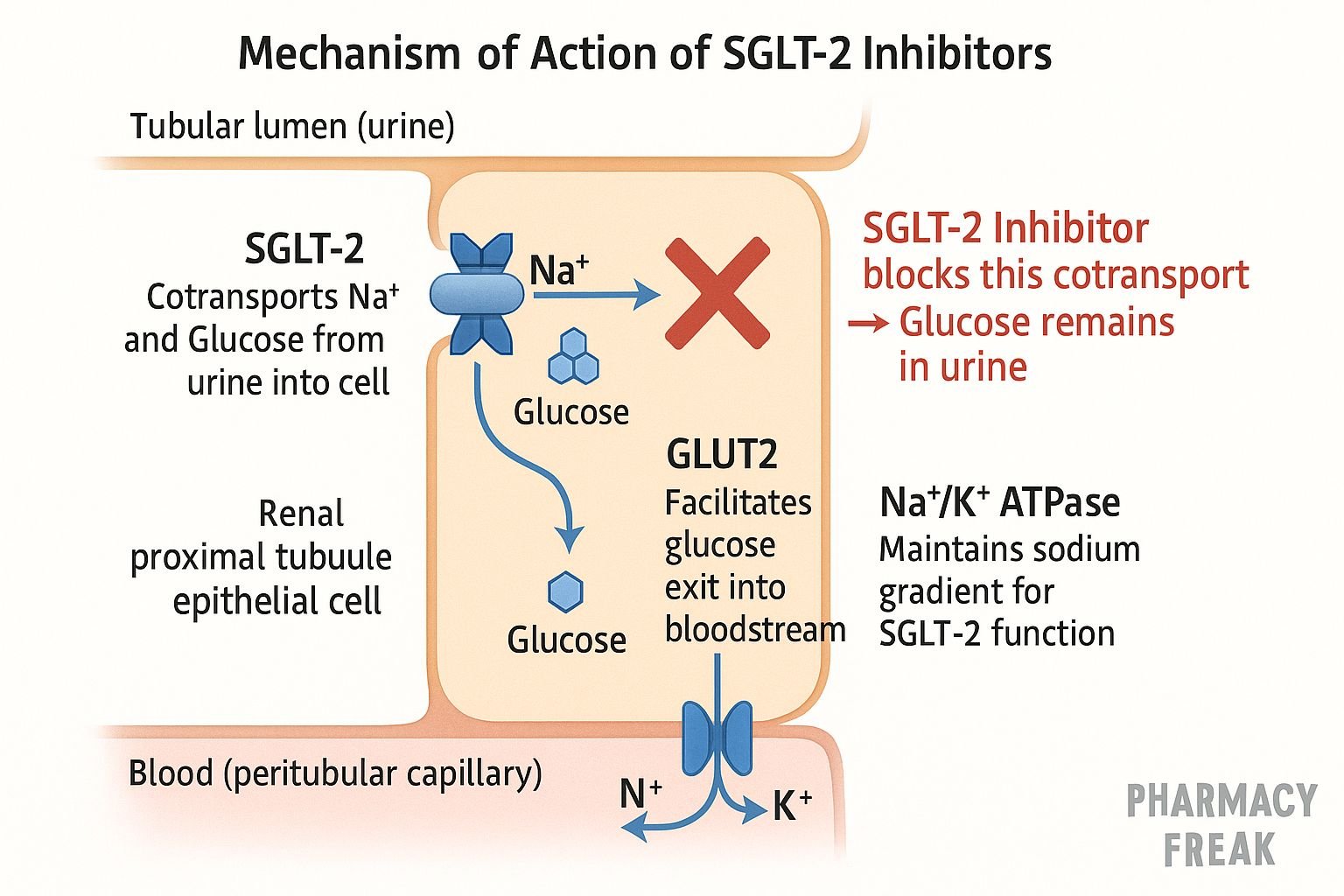
SGLT2 Inhibitors (e.g., empagliflozin): Block glucose reabsorption in the kidney, helping lower blood sugar in diabetes.
Clinical Relevance
Transporter-targeting drugs are especially important in psychiatry, nephrology, and endocrinology. Their specificity for certain transporters explains many therapeutic and side effects.
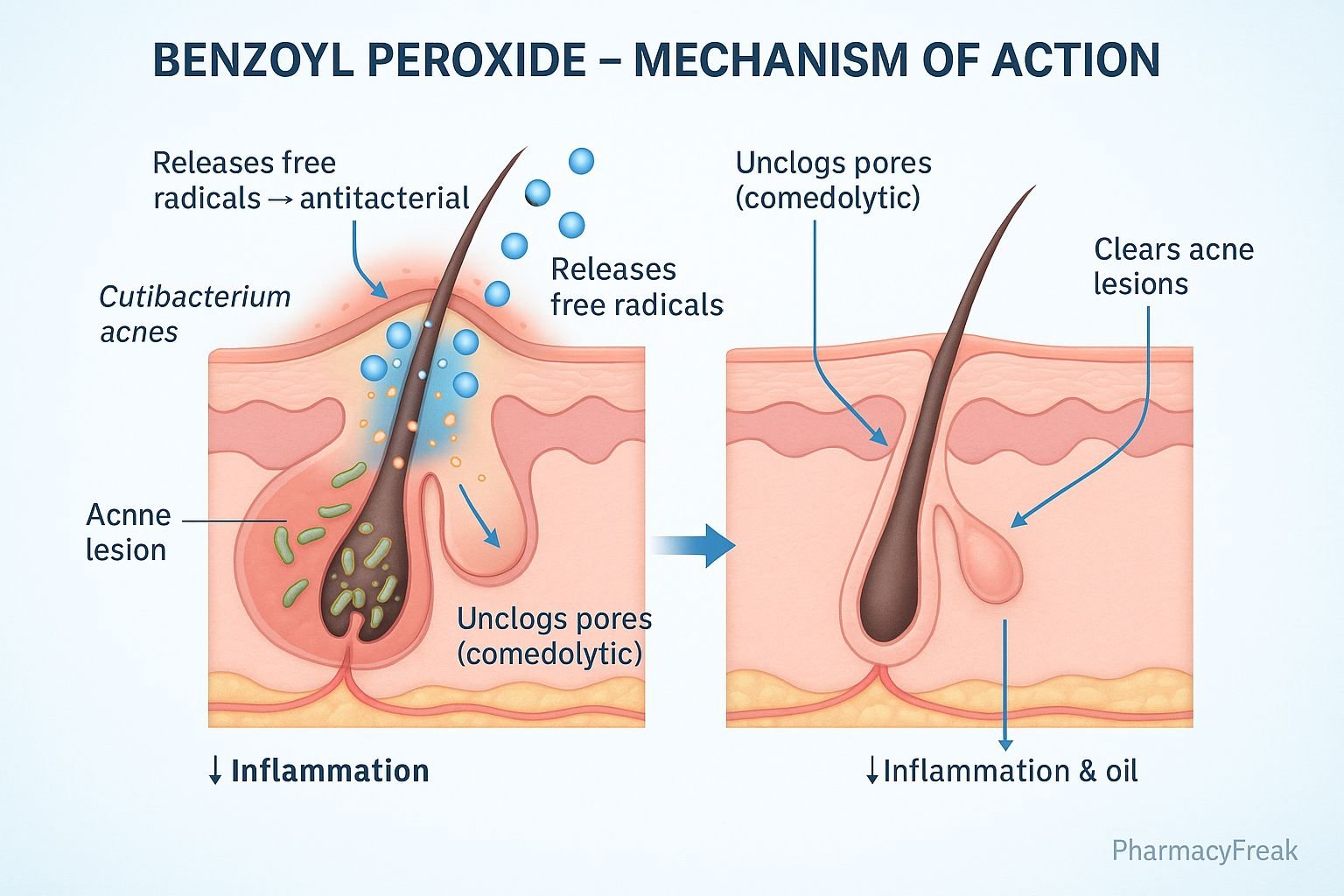
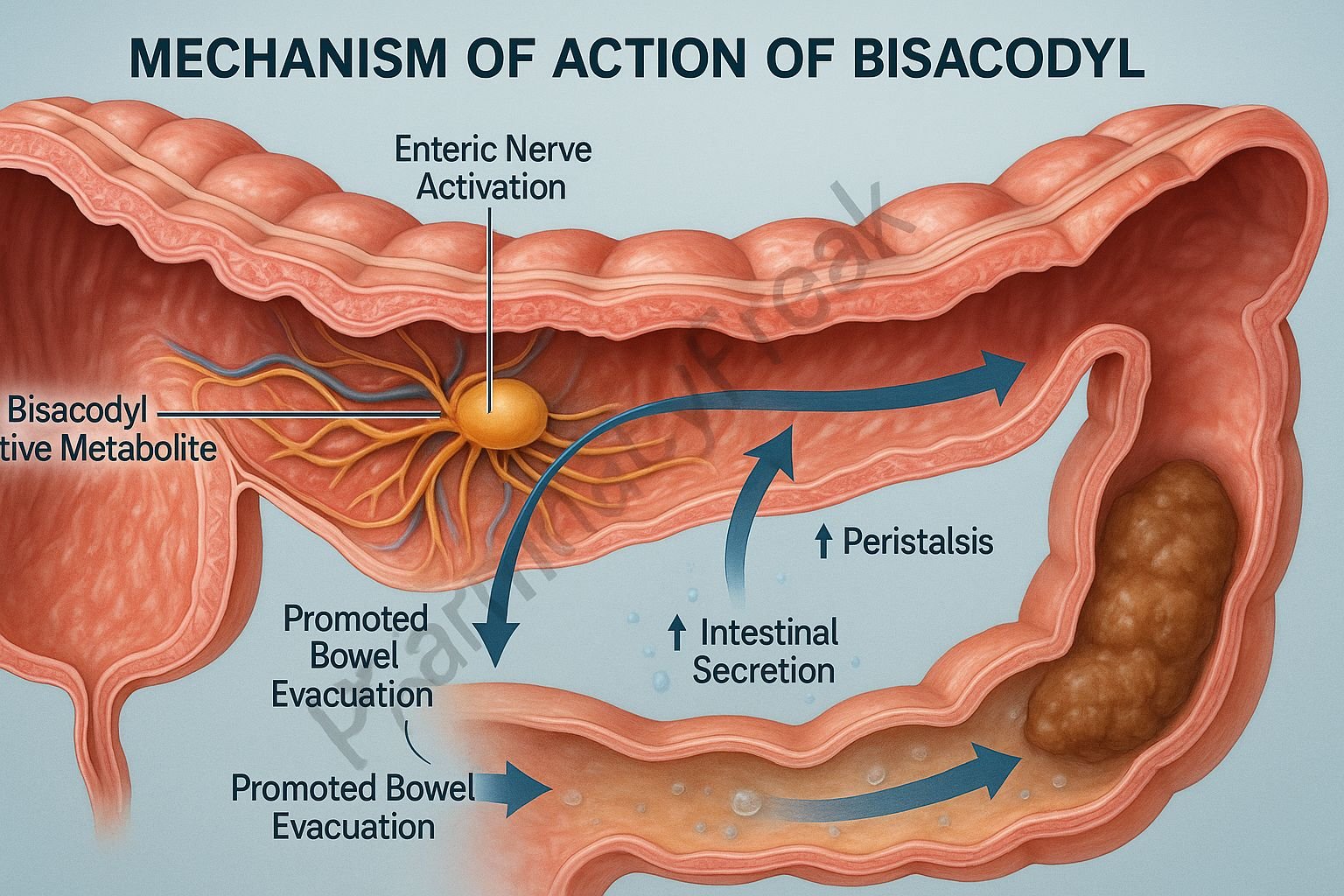
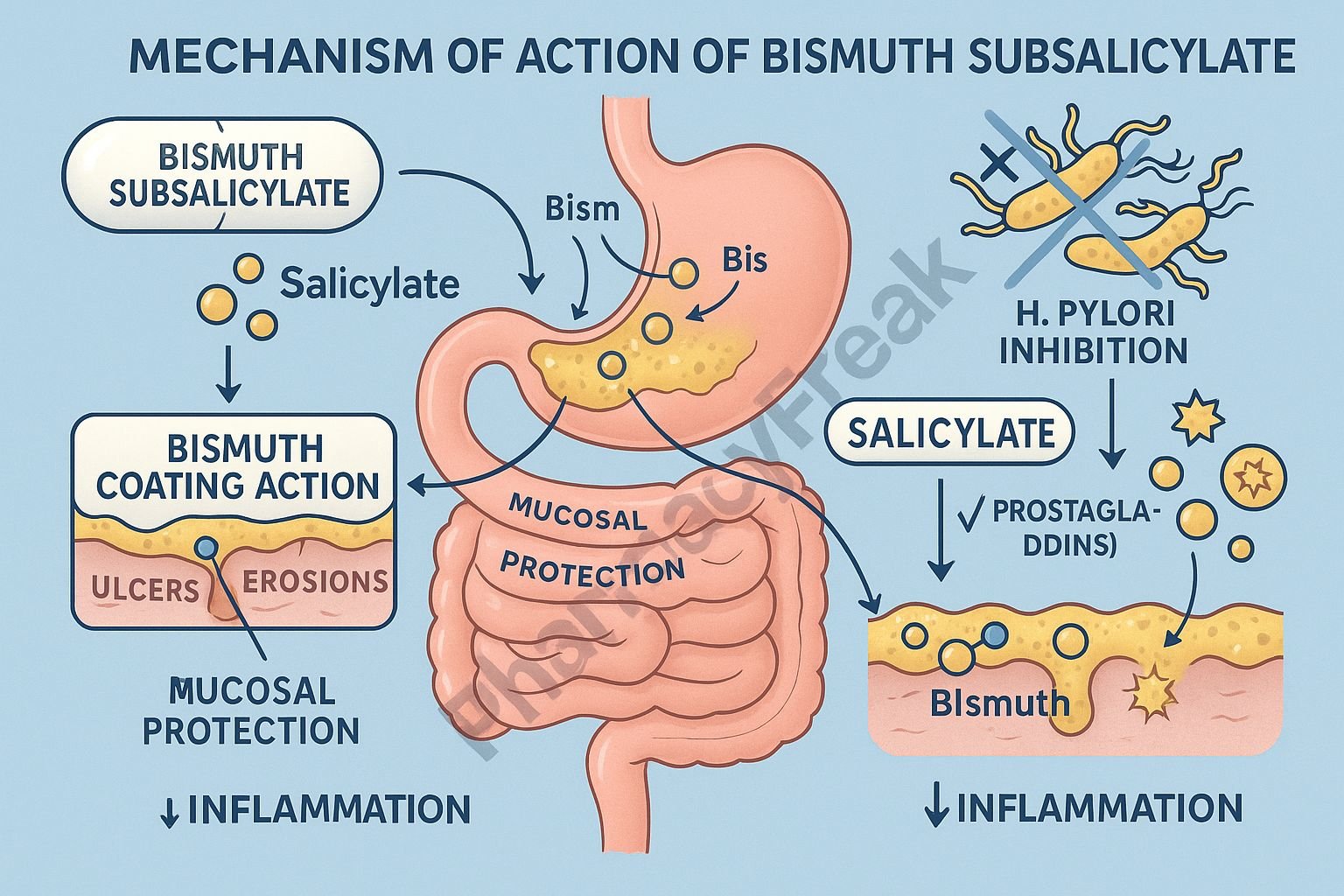
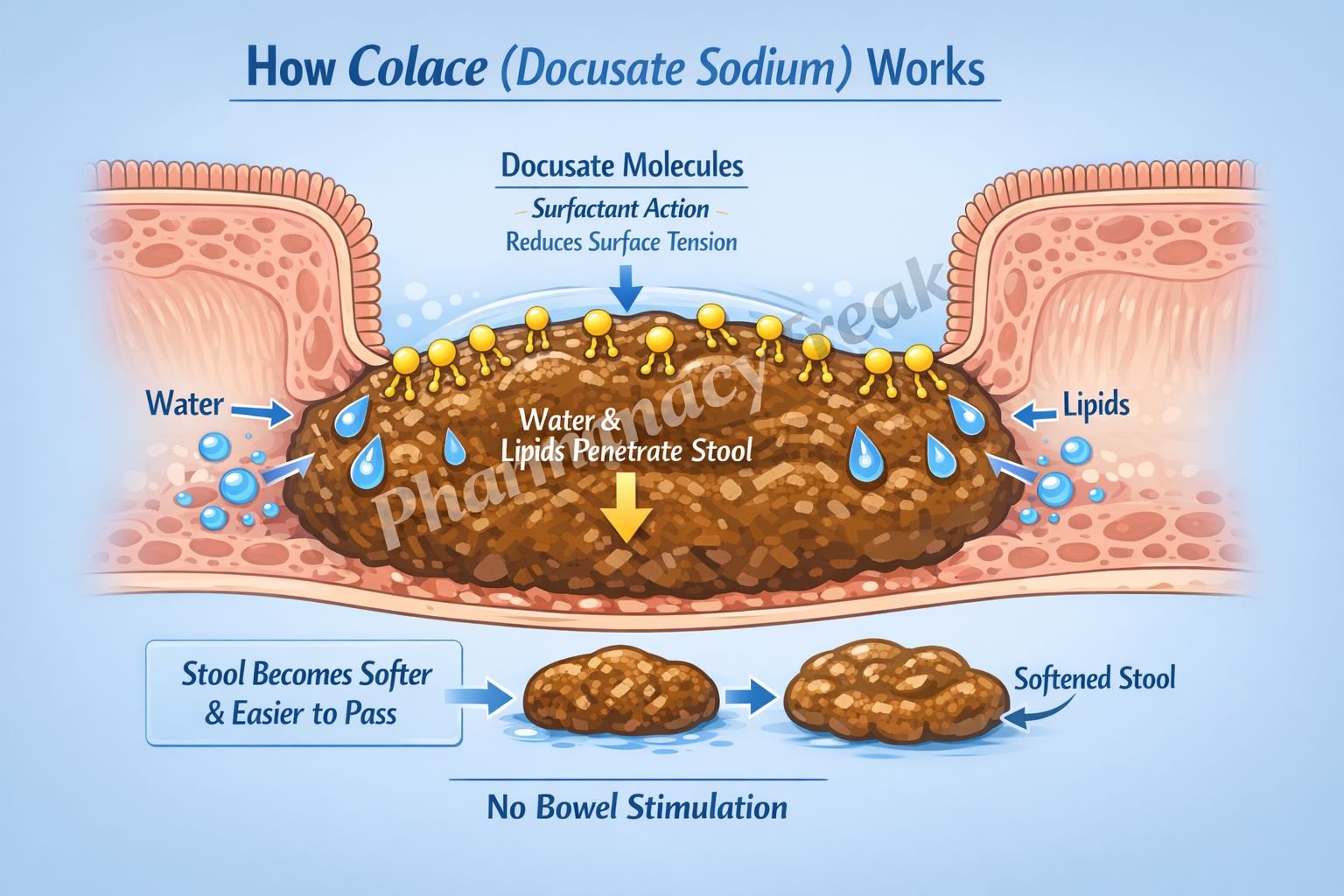
5. Direct Physical or Chemical Action
What Is Direct Action?
Some drugs act through physical or chemical properties rather than binding to receptors, enzymes, or transporters.
Examples
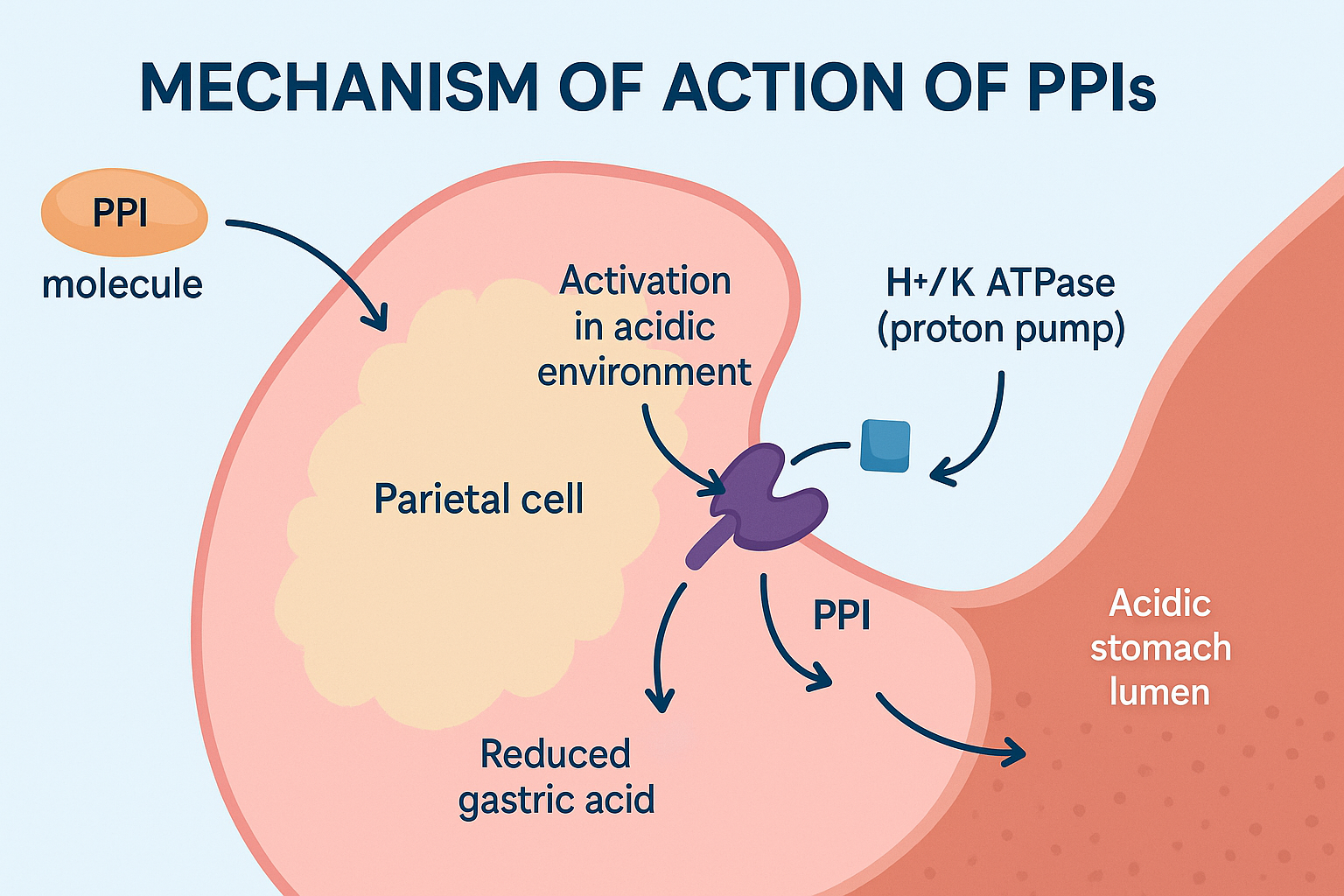
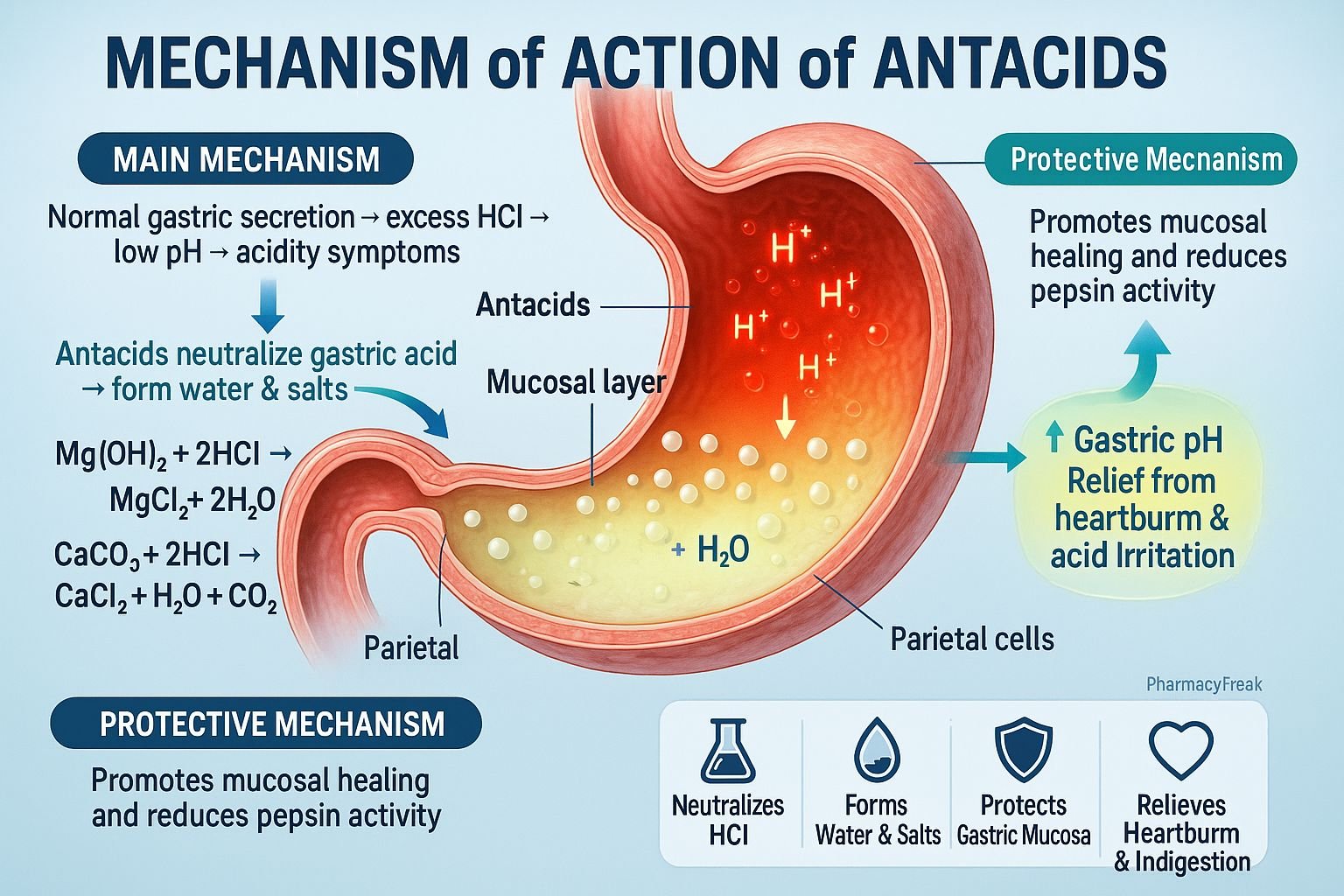
Antacids (e.g., magnesium hydroxide): Neutralize stomach acid by direct chemical reaction.
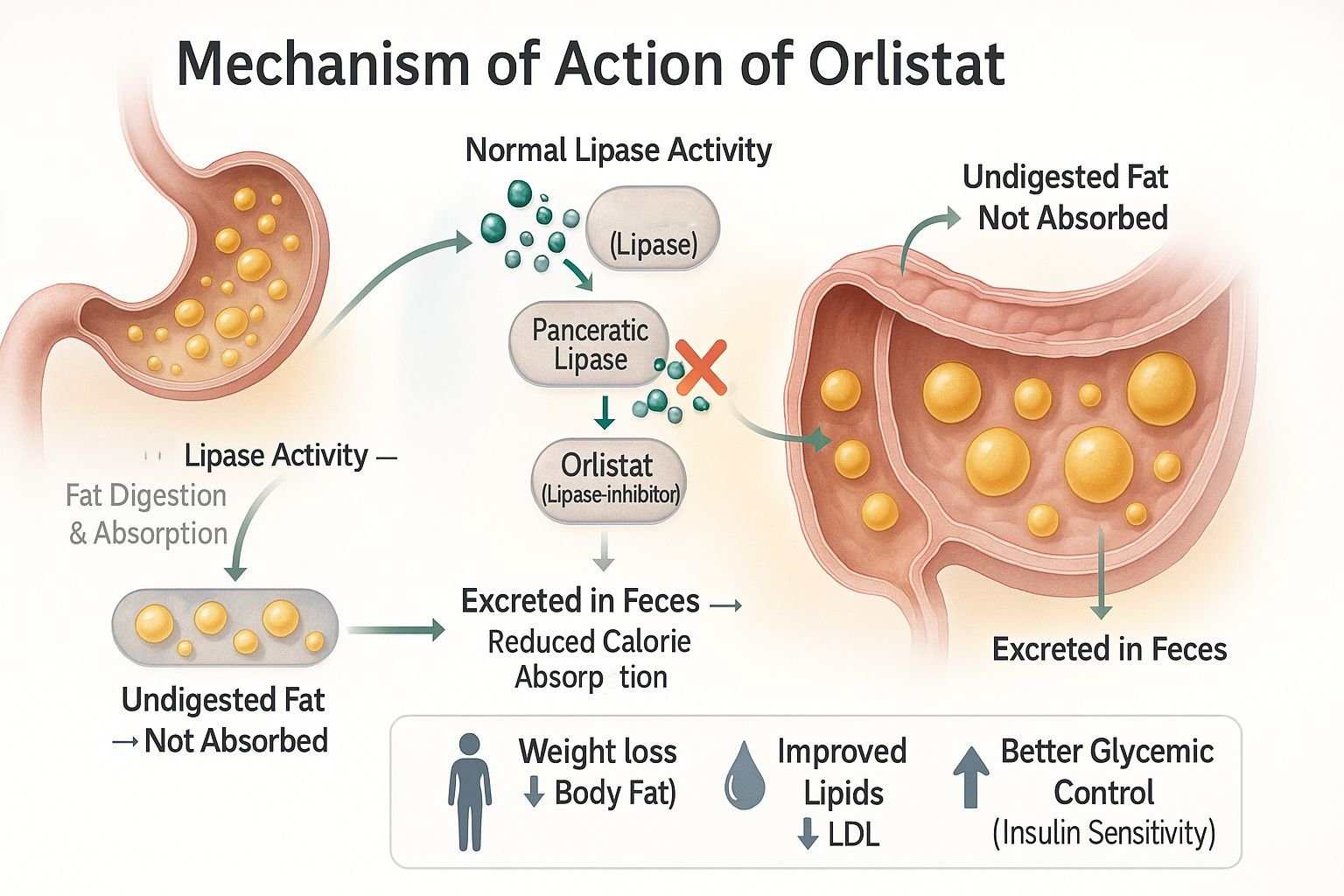
Osmotic laxatives (e.g., lactulose): Draw water into the intestine through osmosis to promote bowel movement.
Chelating agents (e.g., EDTA): Bind heavy metals in the blood for removal from the body.
Clinical Relevance
Drugs with direct actions tend to have quick, predictable effects. However, they are often less specific than drugs that act on biological targets.
Drug-Receptor Interactions: Key Concepts
Affinity and Efficacy
Affinity: The strength with which a drug binds to its target.
Efficacy: The ability of a drug, once bound, to produce a maximum response.
Potency and Selectivity
Potency: How much drug is needed to produce an effect.
Selectivity: The degree to which a drug acts on a particular target, which helps minimize side effects.
Dose-Response Relationship
This relationship explains how the magnitude of drug effect changes with dose. It is key to understanding therapeutic windows, toxicity, and effective dosing.
Factors Affecting Mechanism of Action
Several factors can modify how drugs exert their effects, including:
Genetic differences: Affect drug targets and metabolism.
Age and sex: Influence receptor sensitivity and organ function.
Disease states: Can alter drug targets or how drugs are handled by the body.
Drug interactions: Other medications may increase or decrease a drug’s effectiveness.
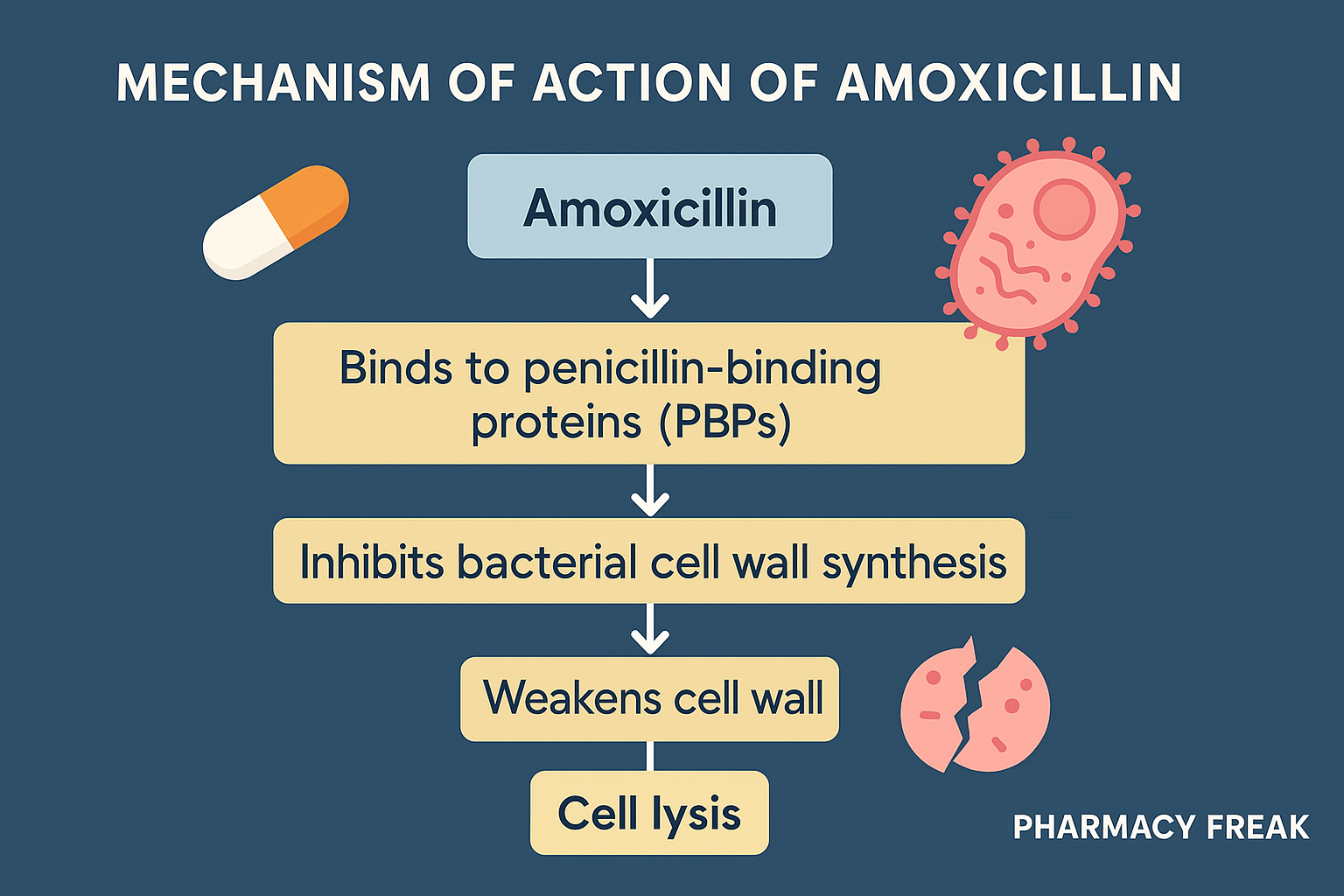
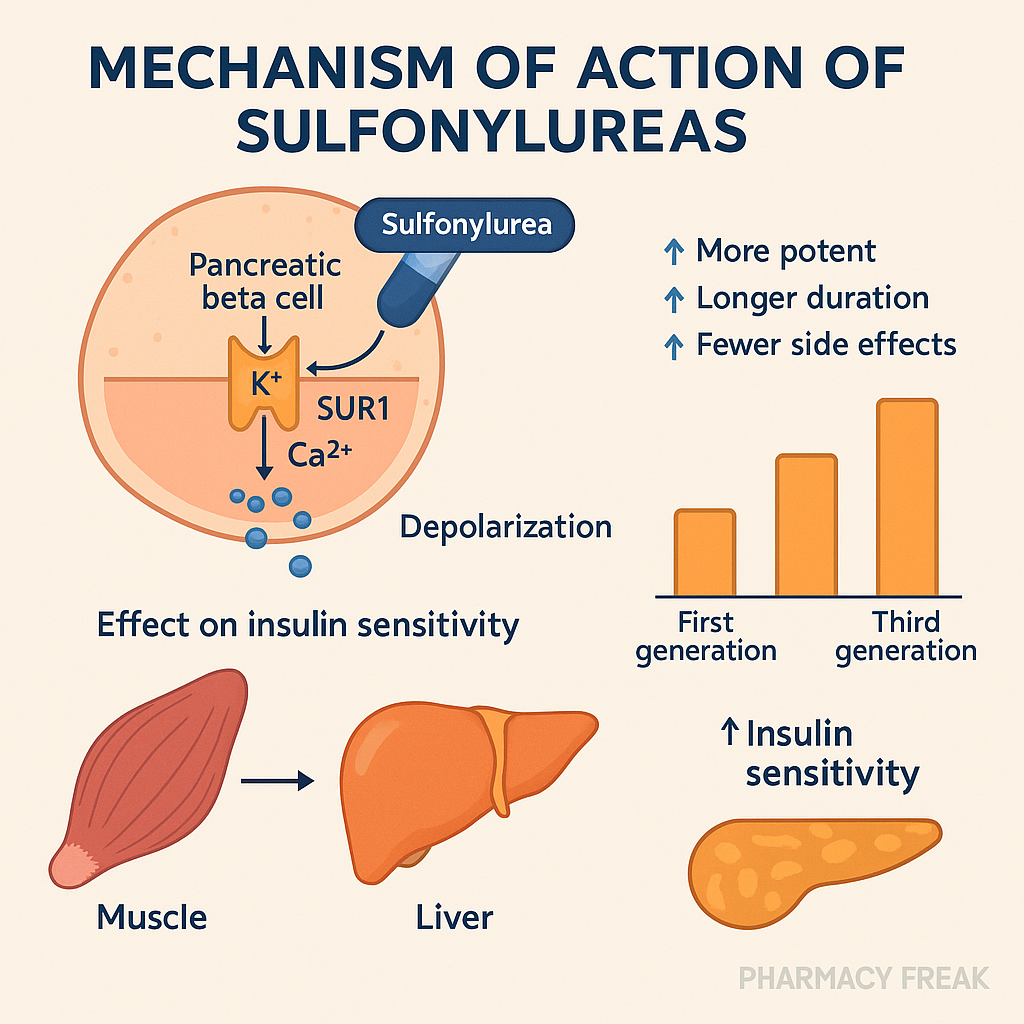
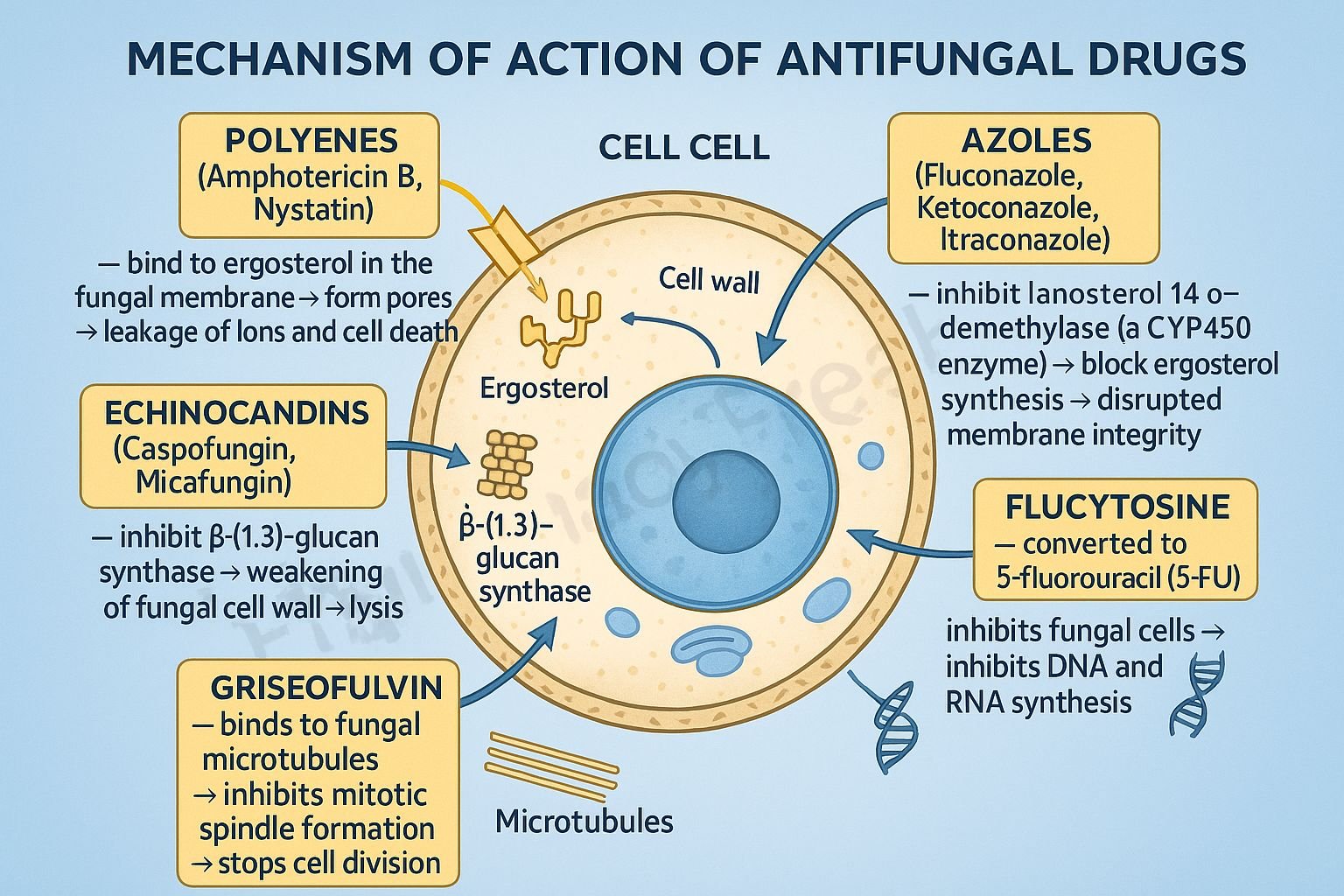
Examples of Mechanism of Action for Major Drug Classes
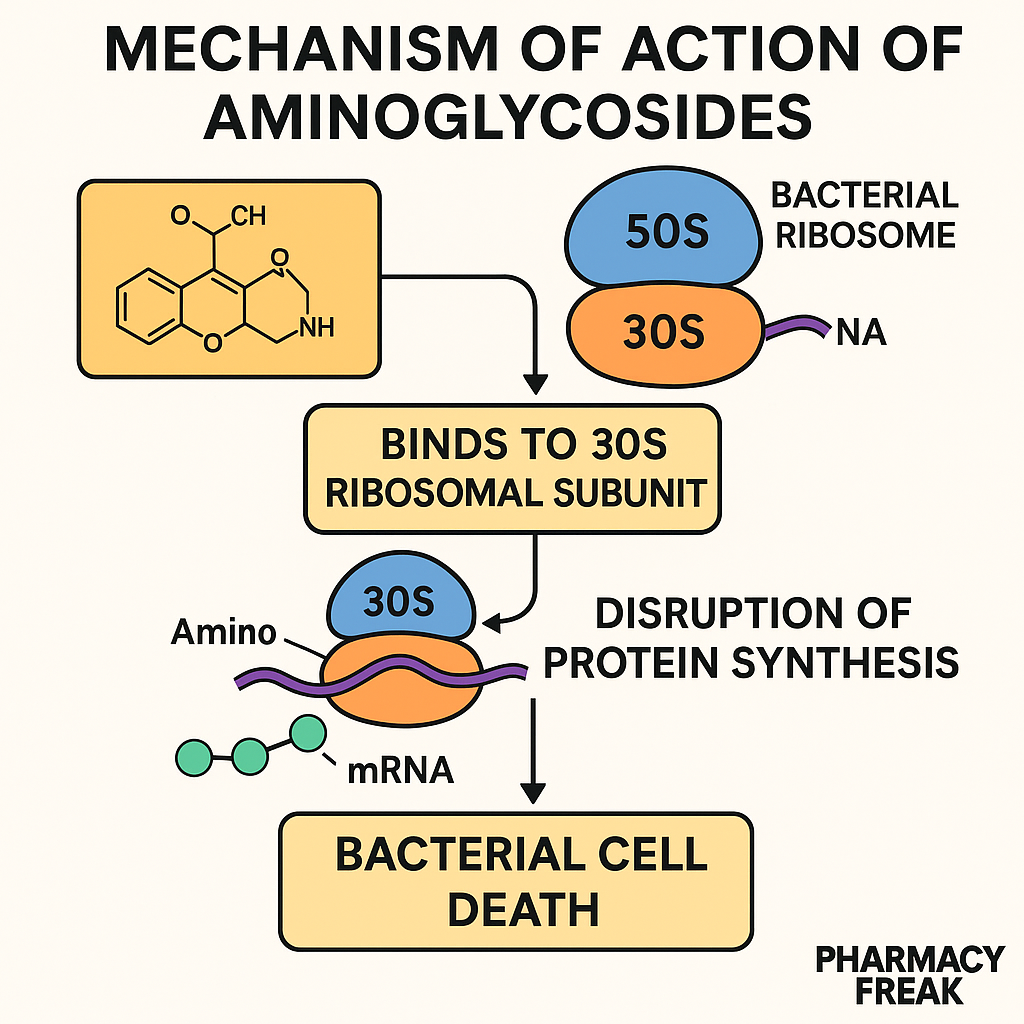
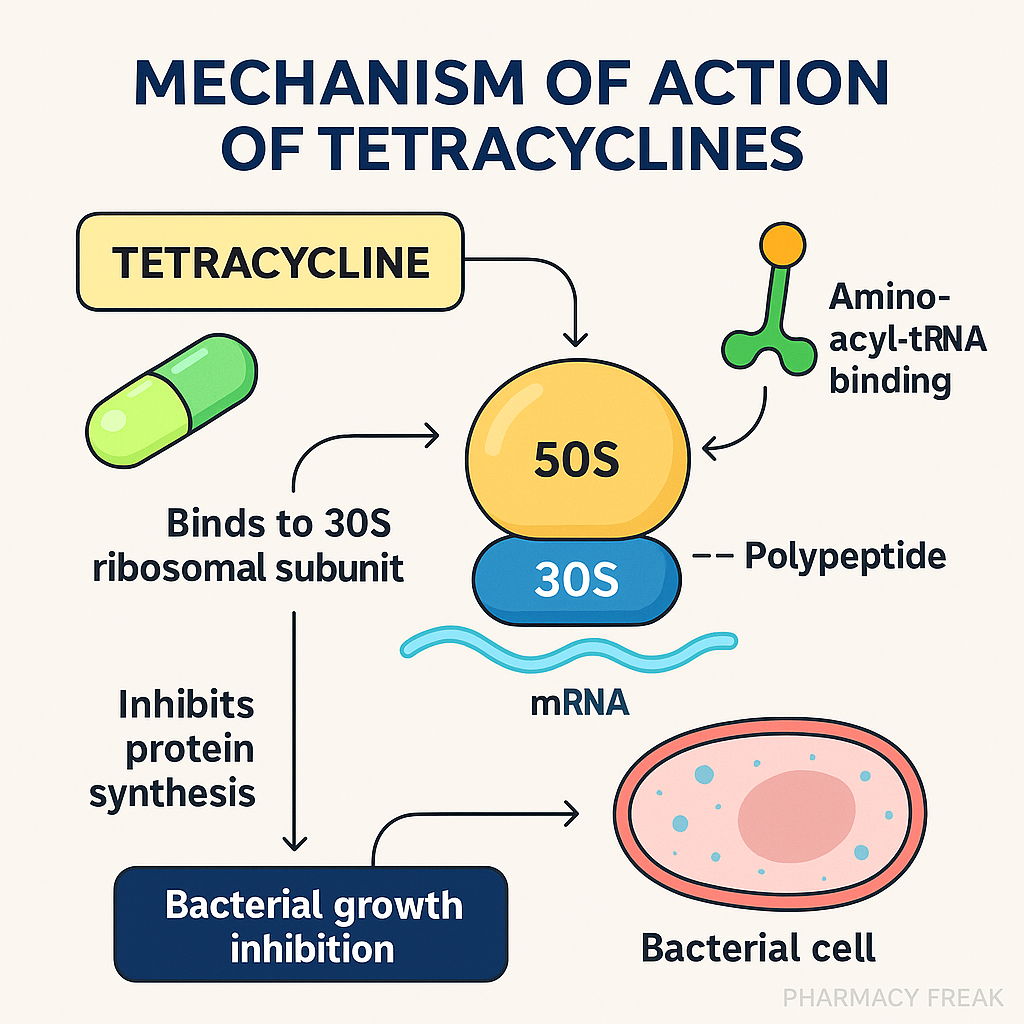
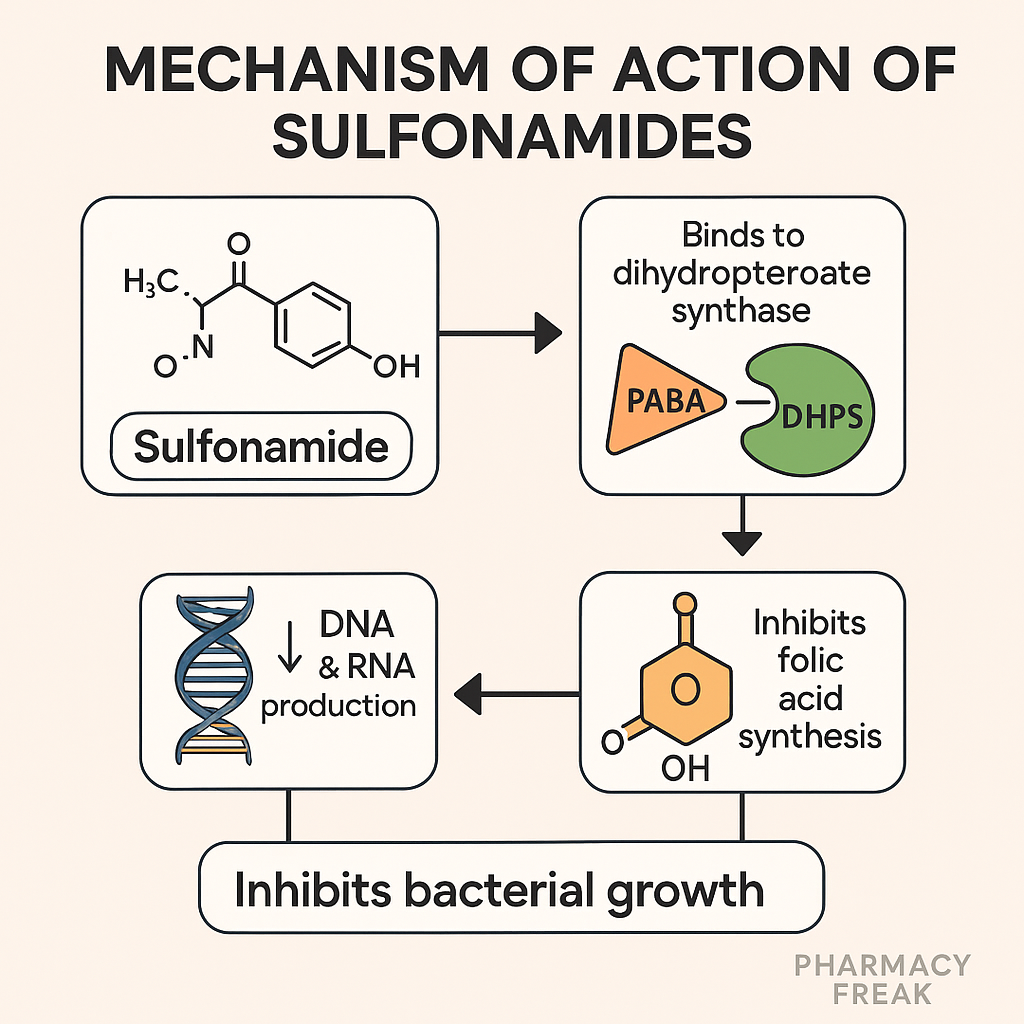
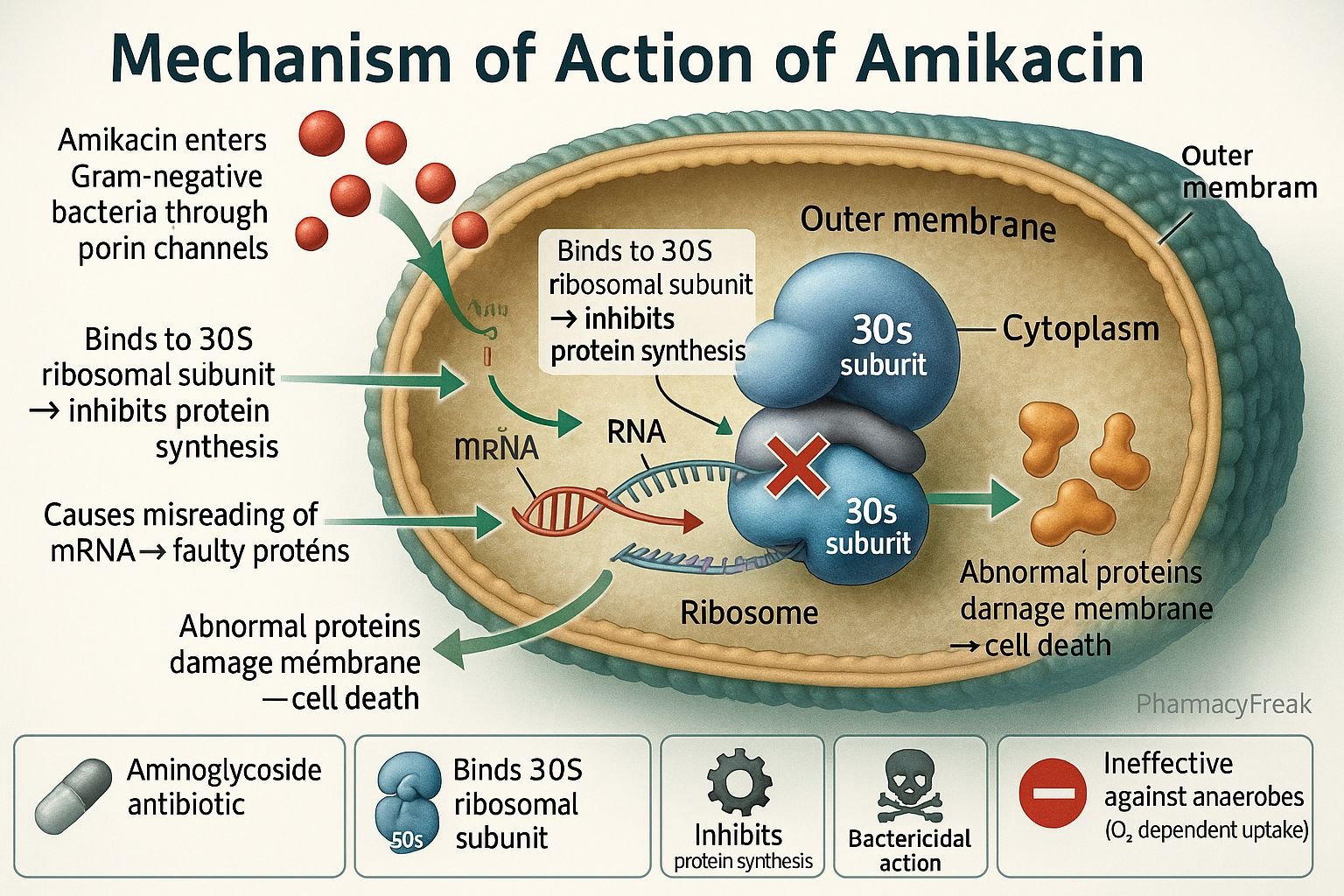
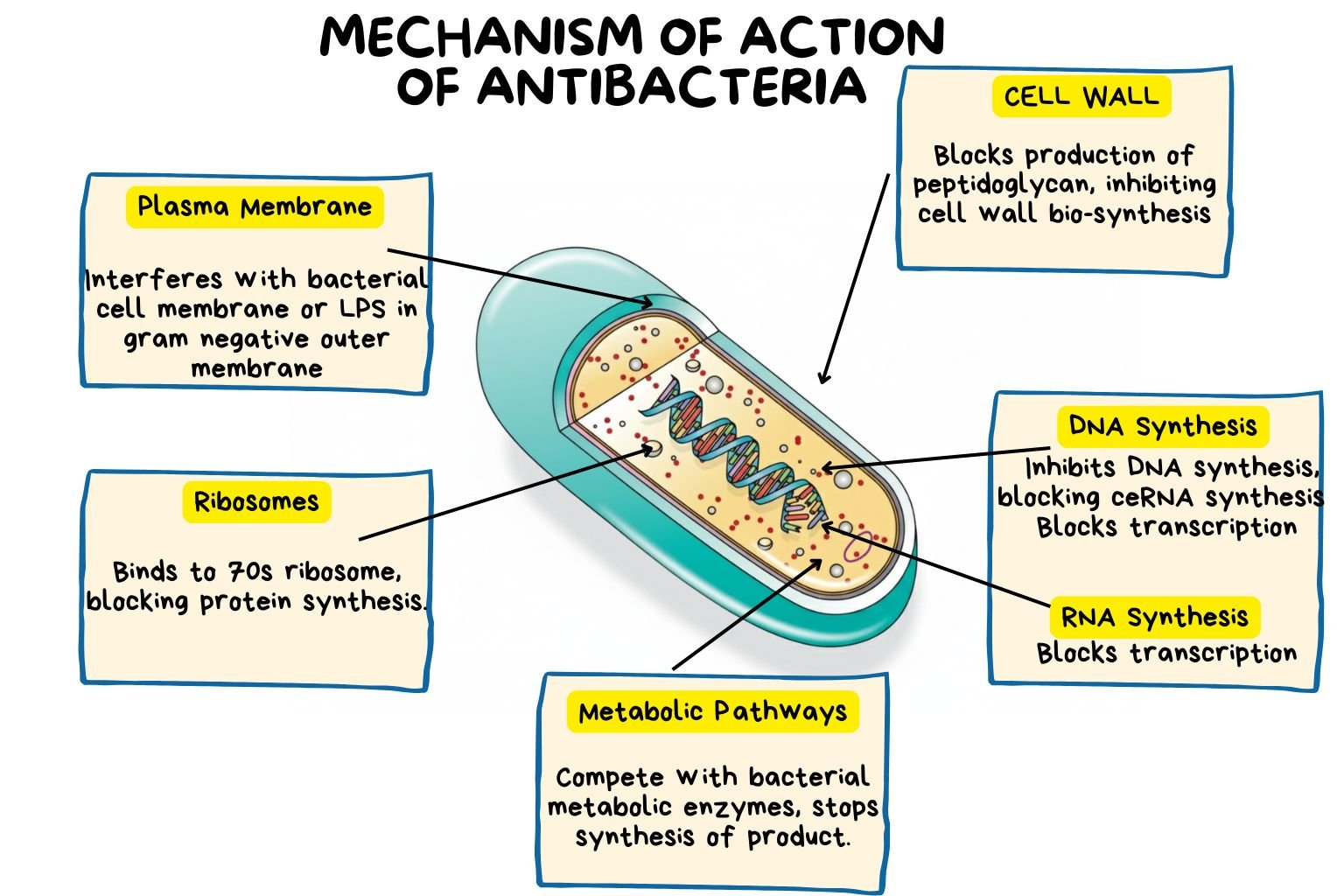
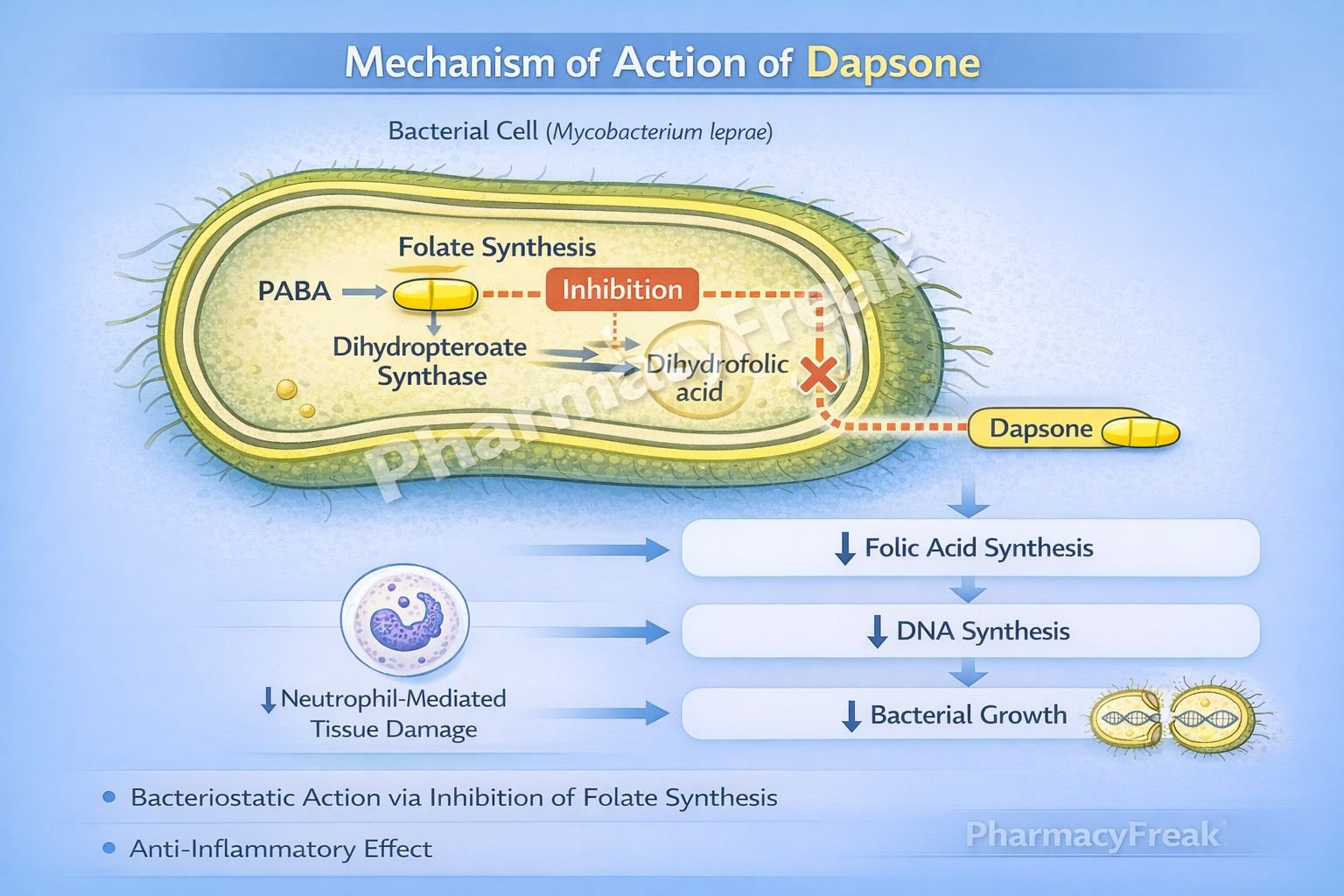
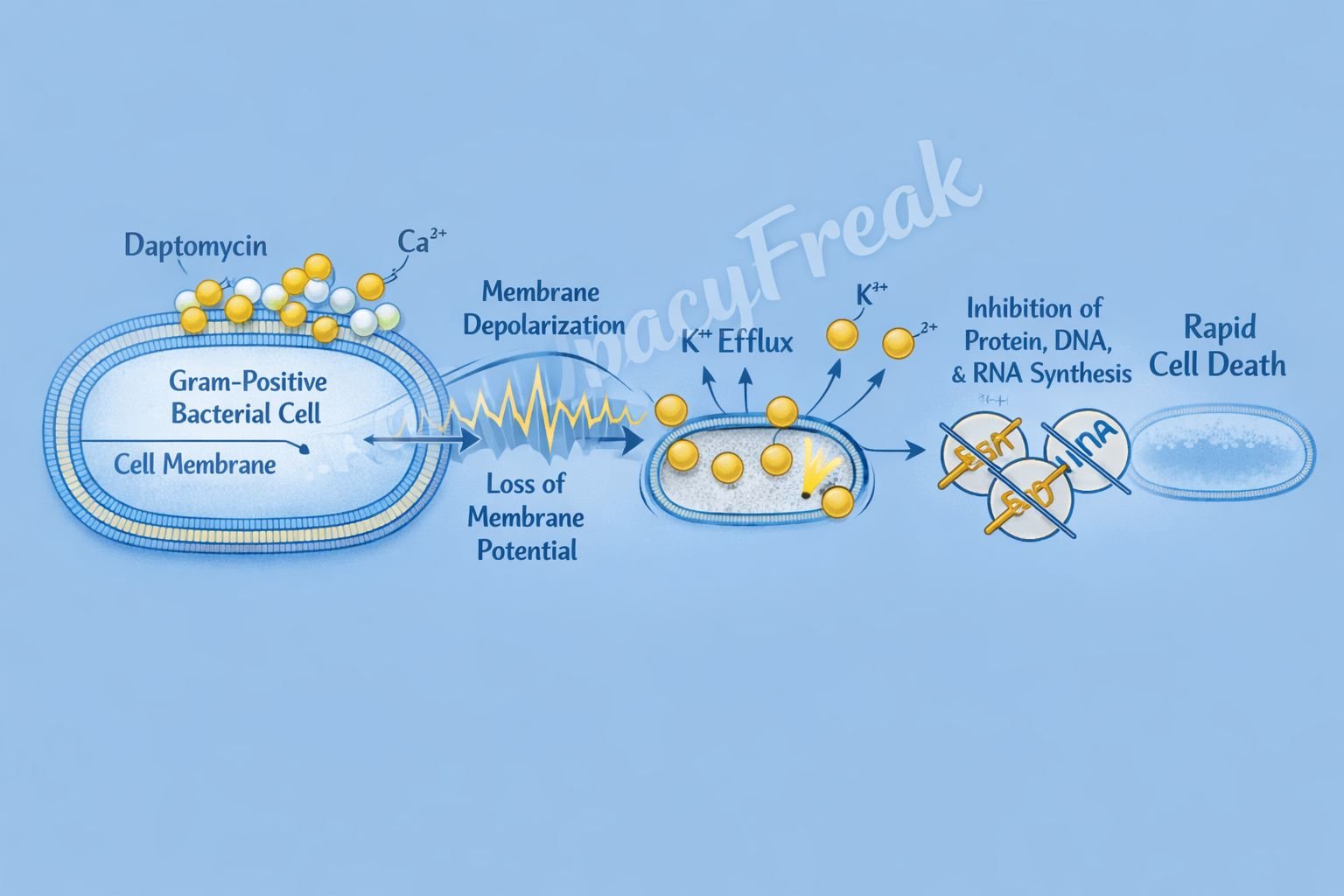
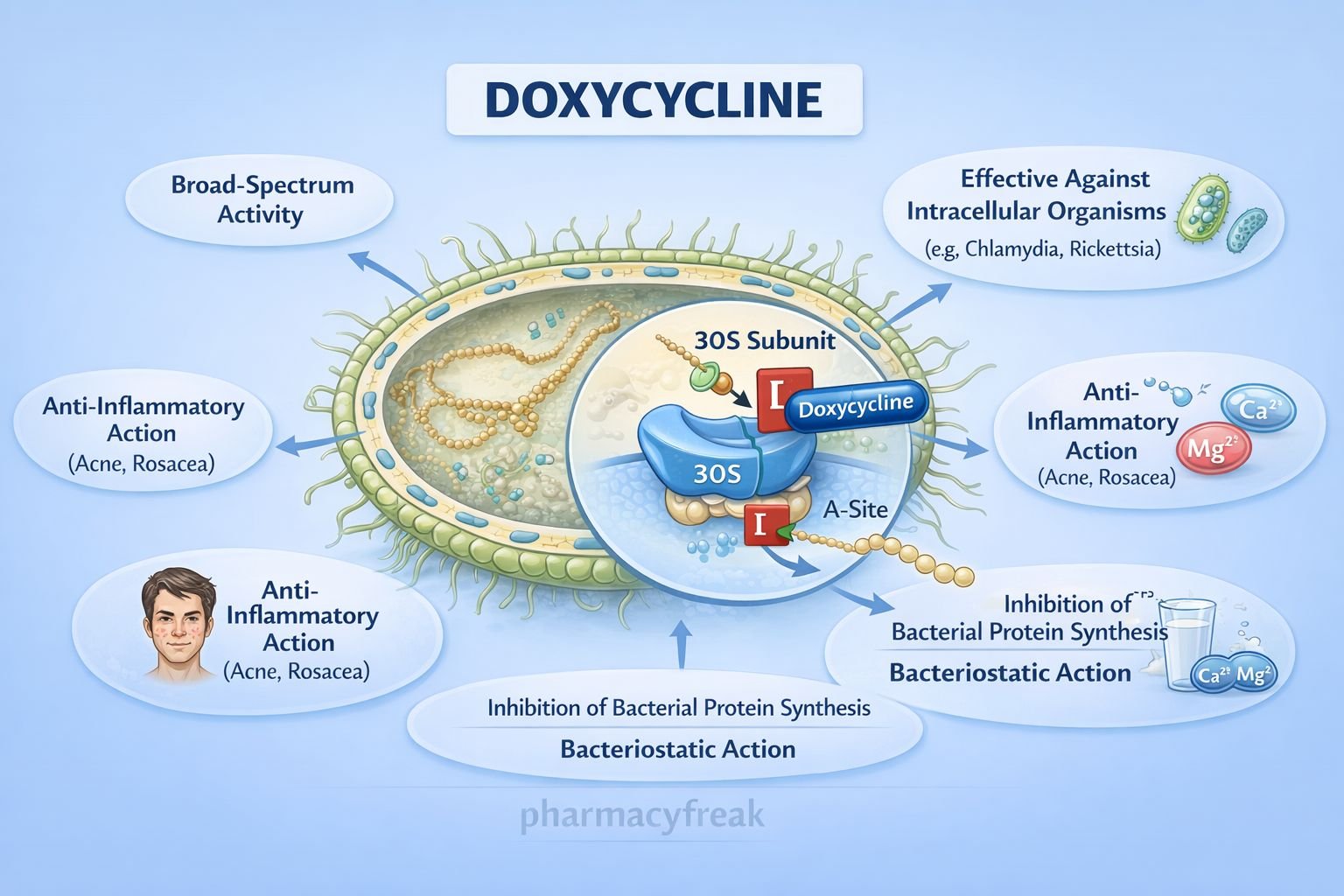
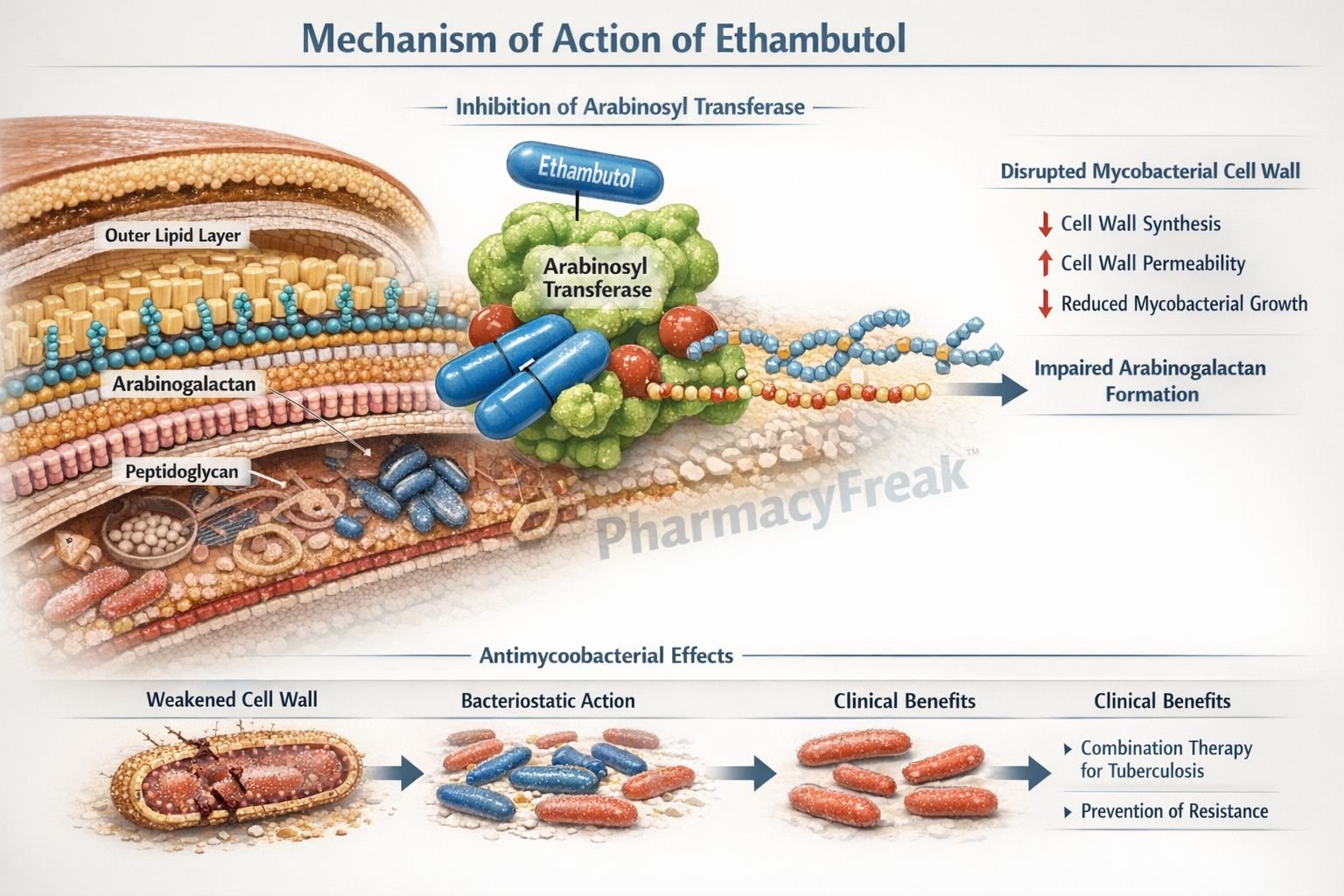
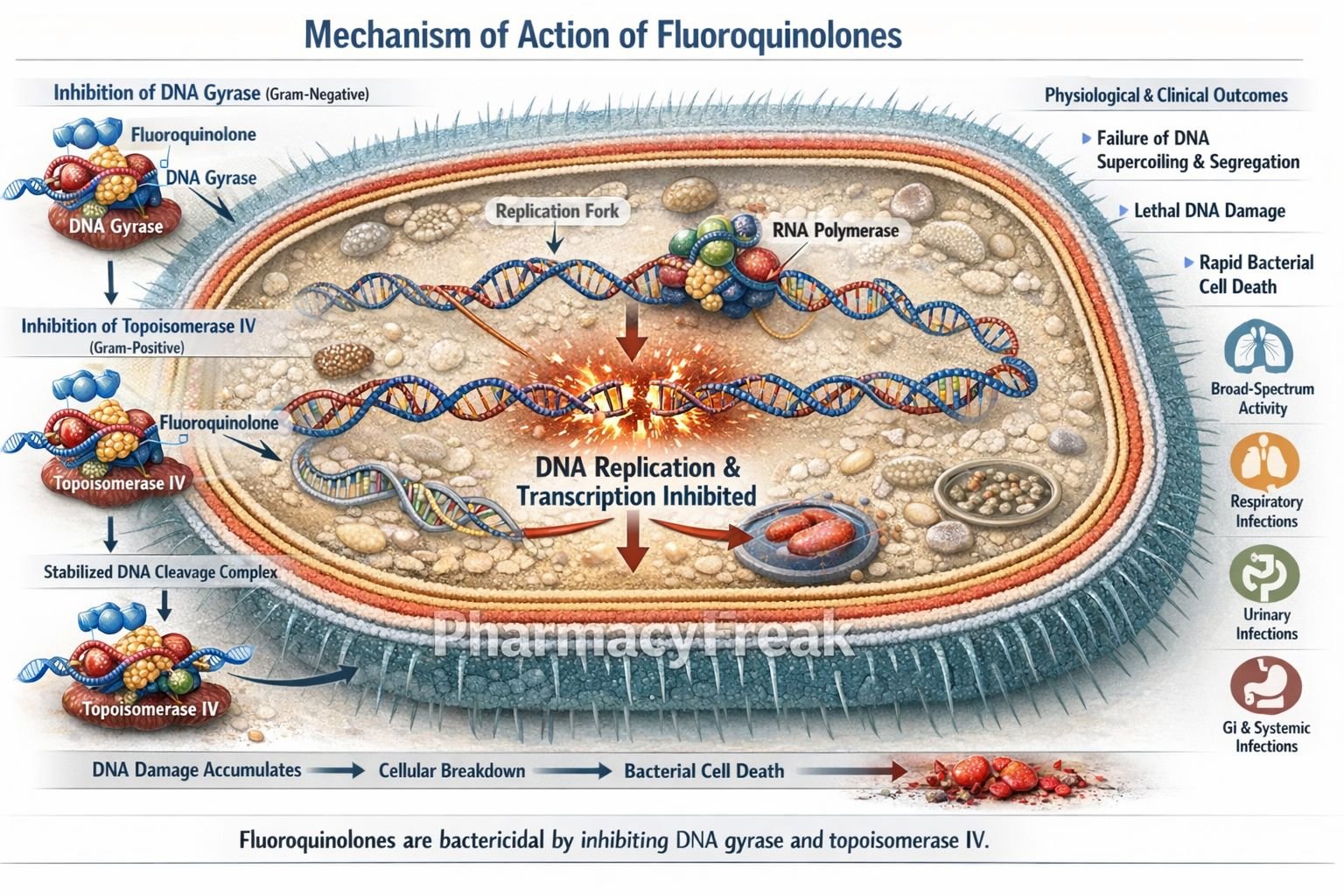
Antibiotics
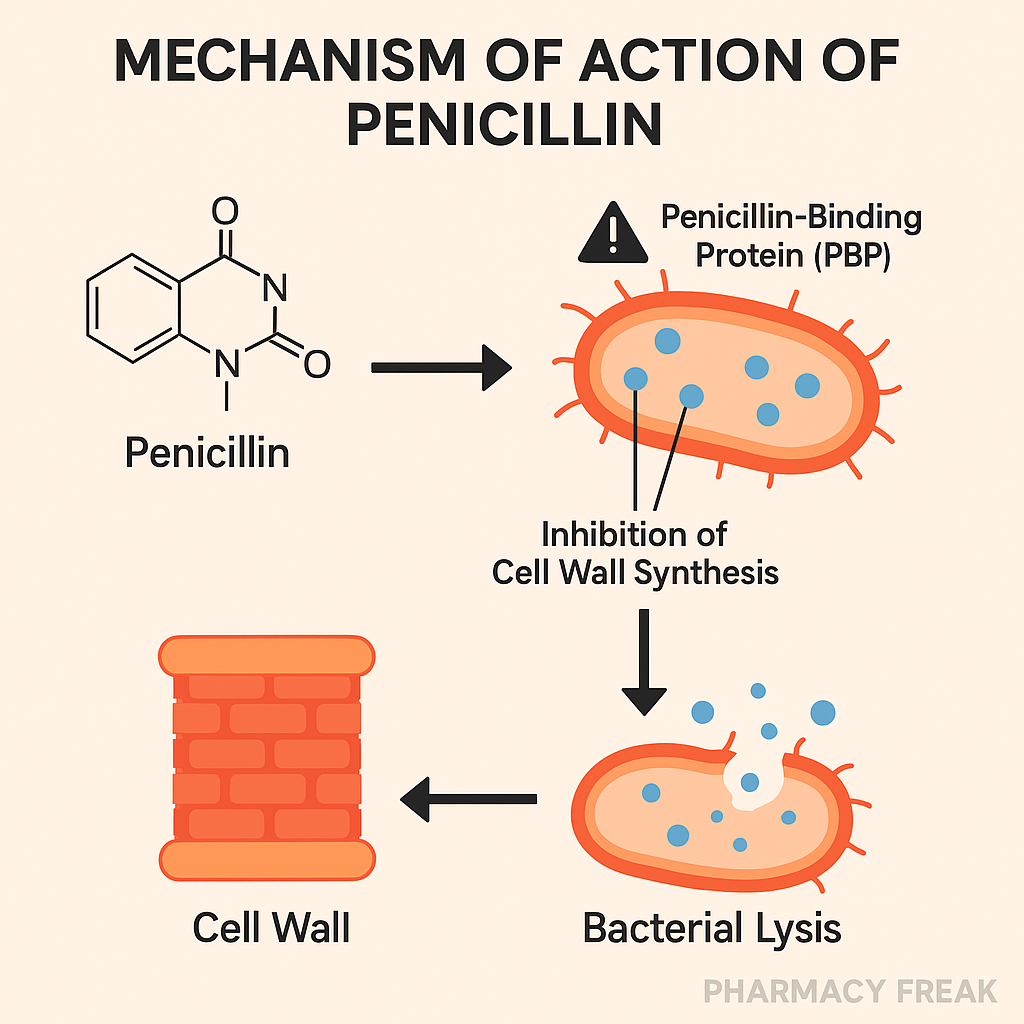
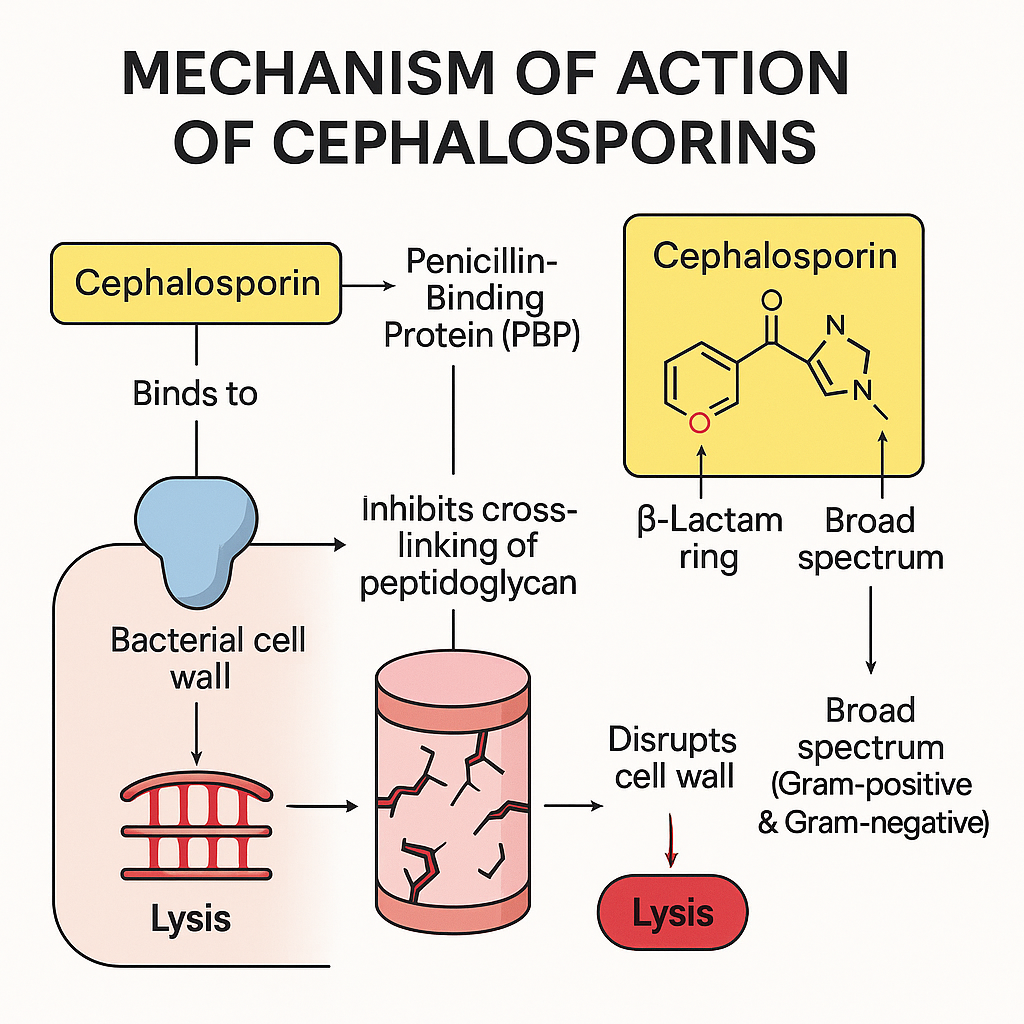
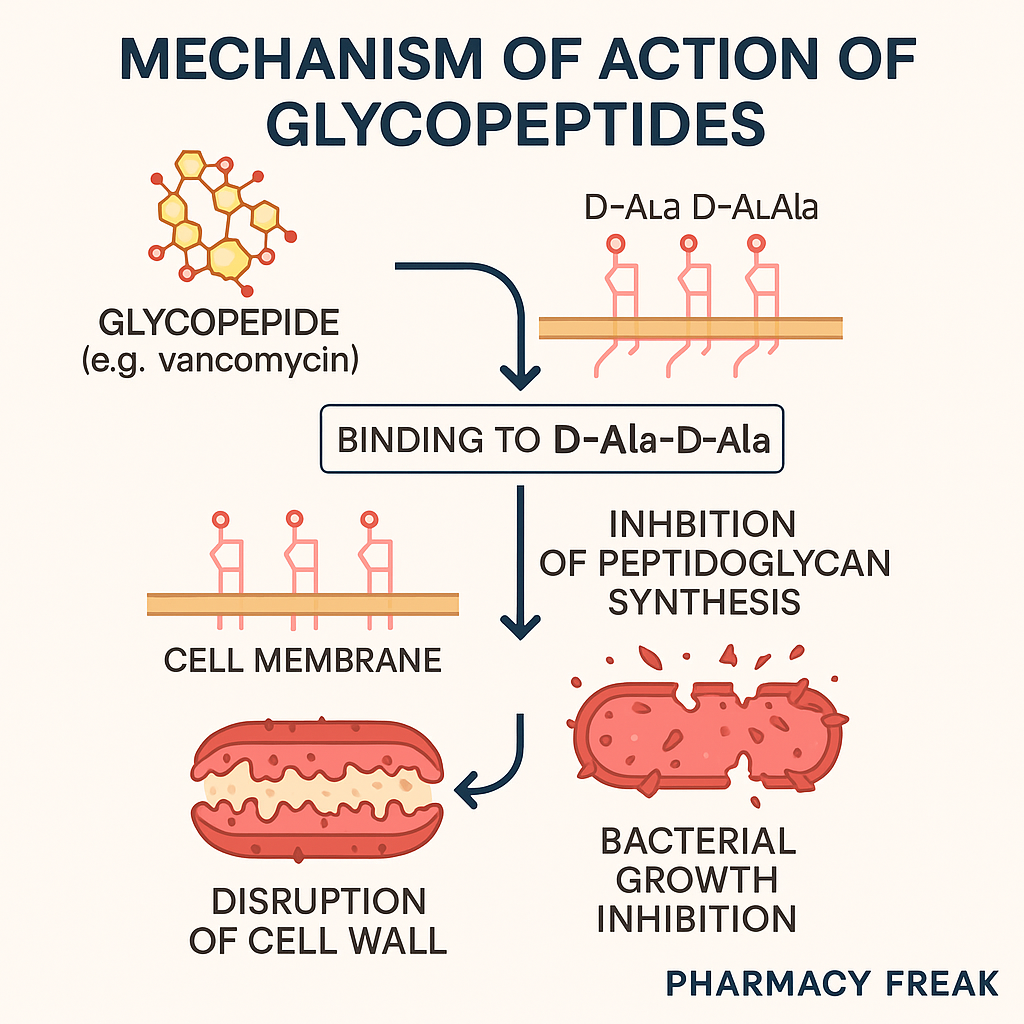
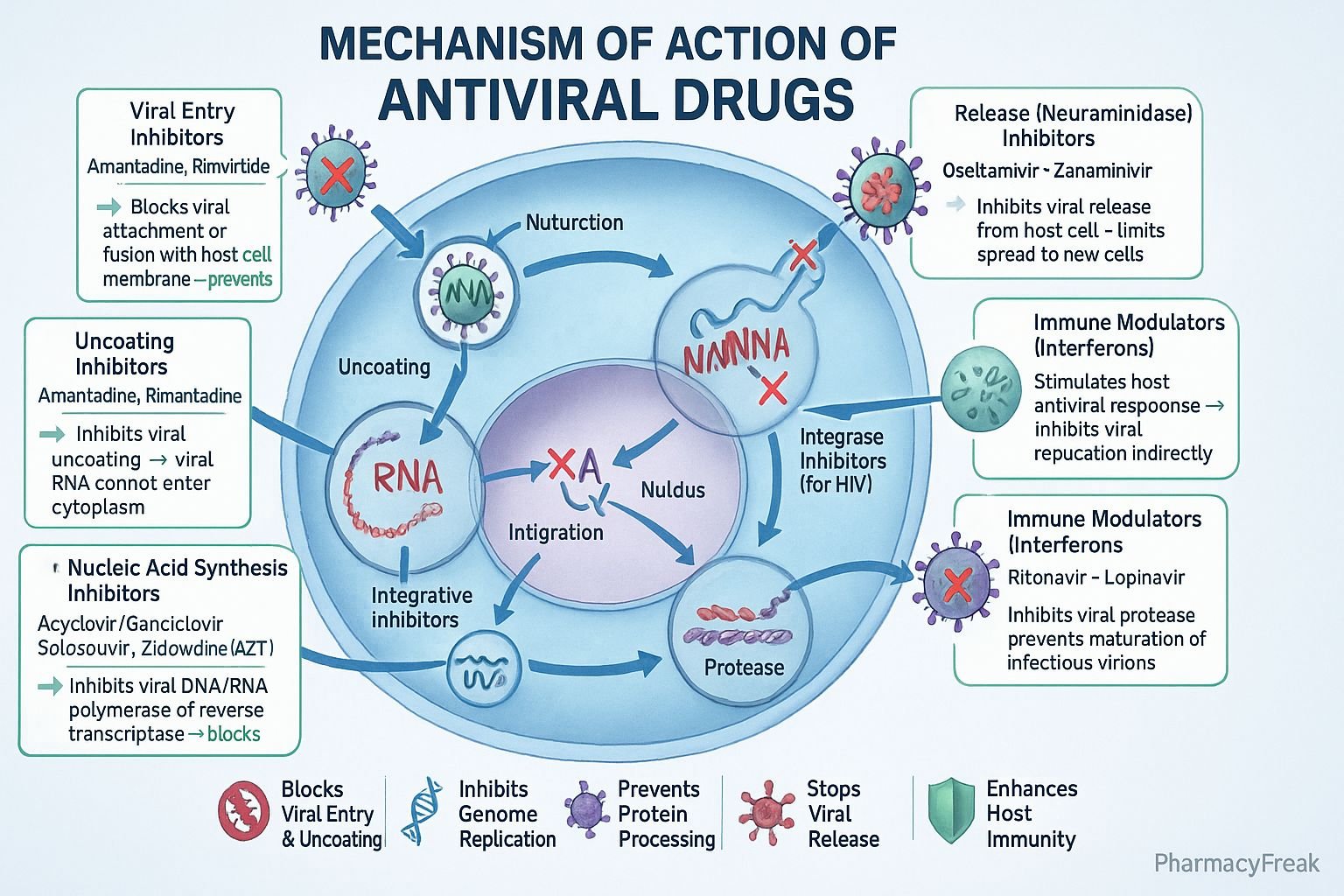
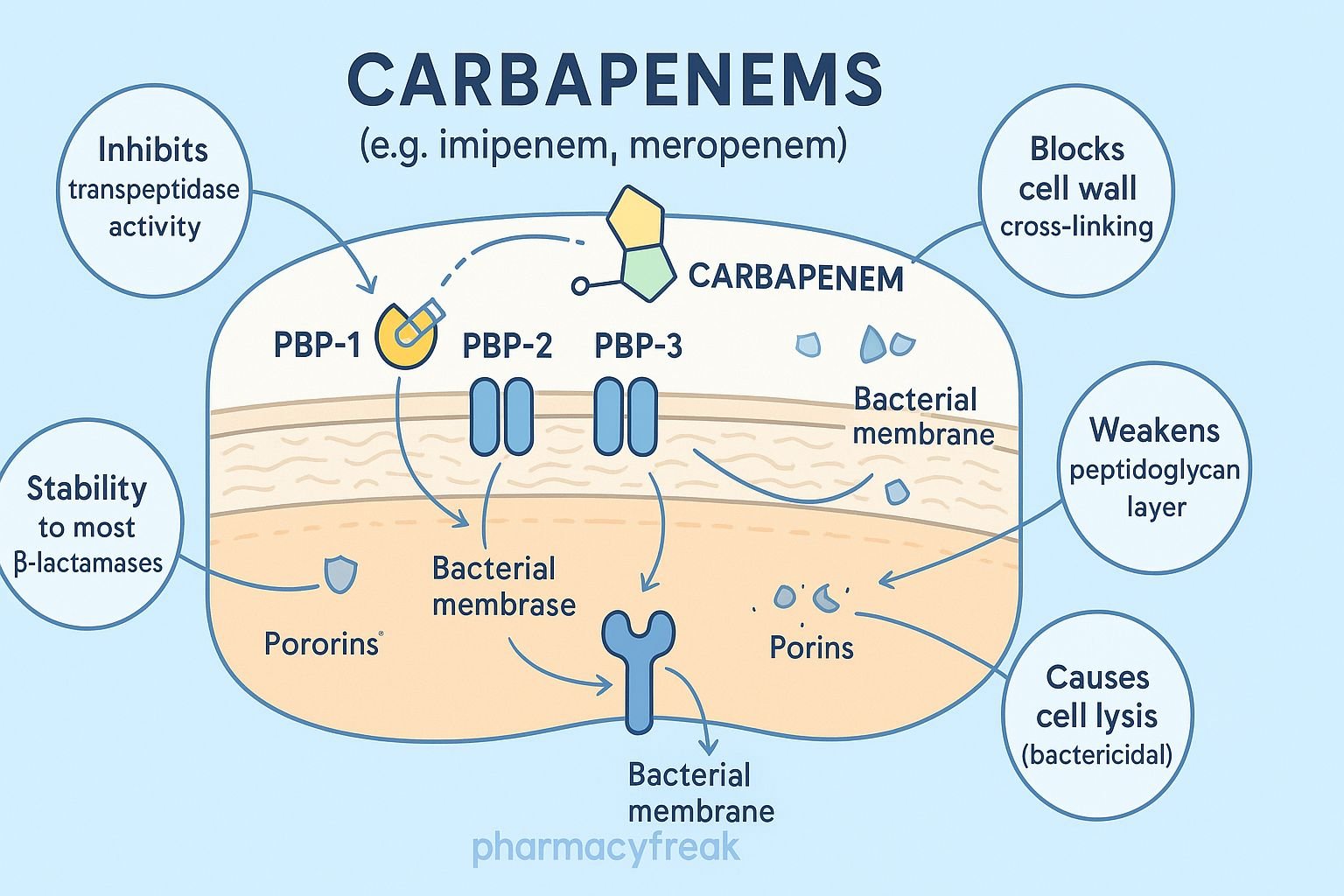
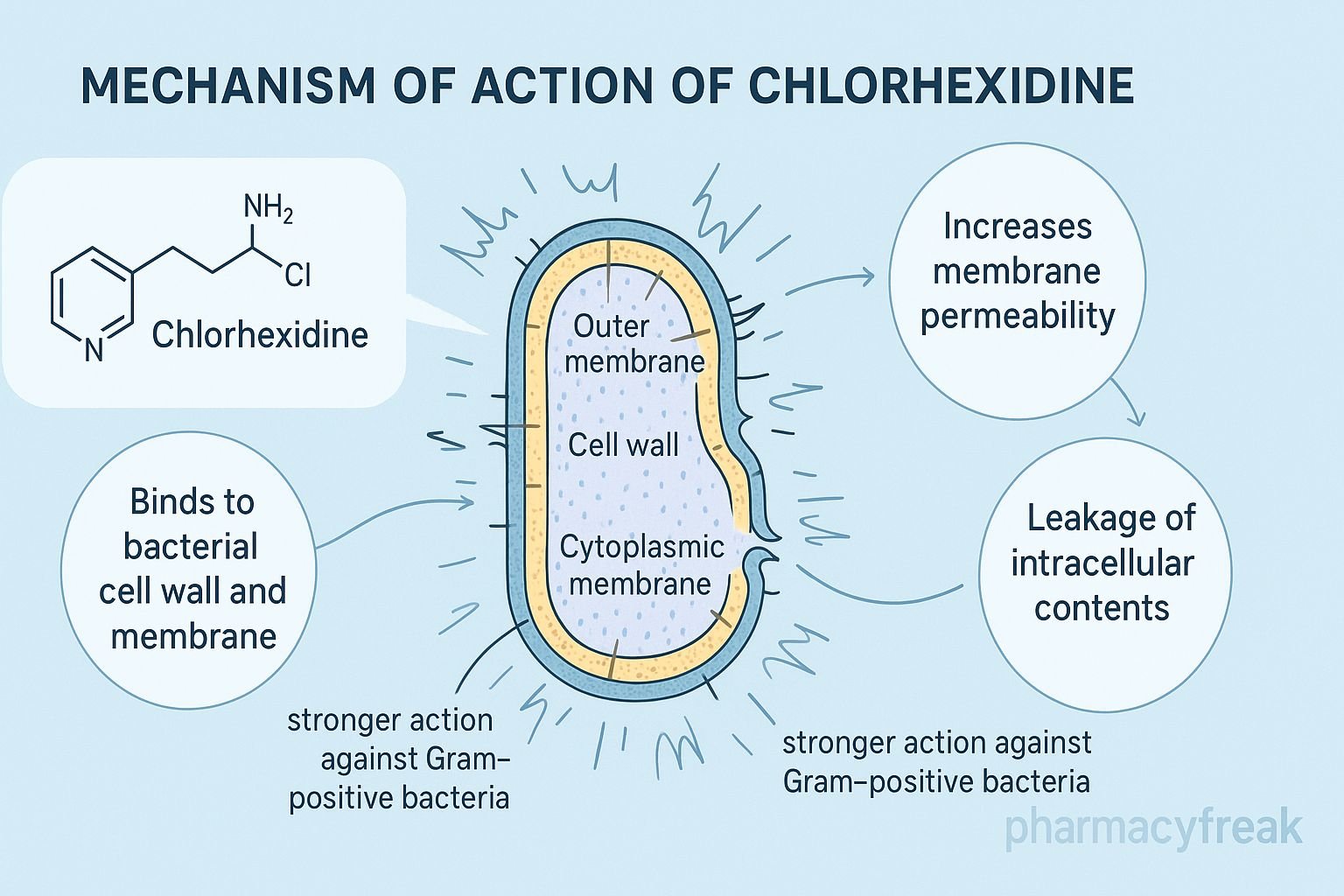
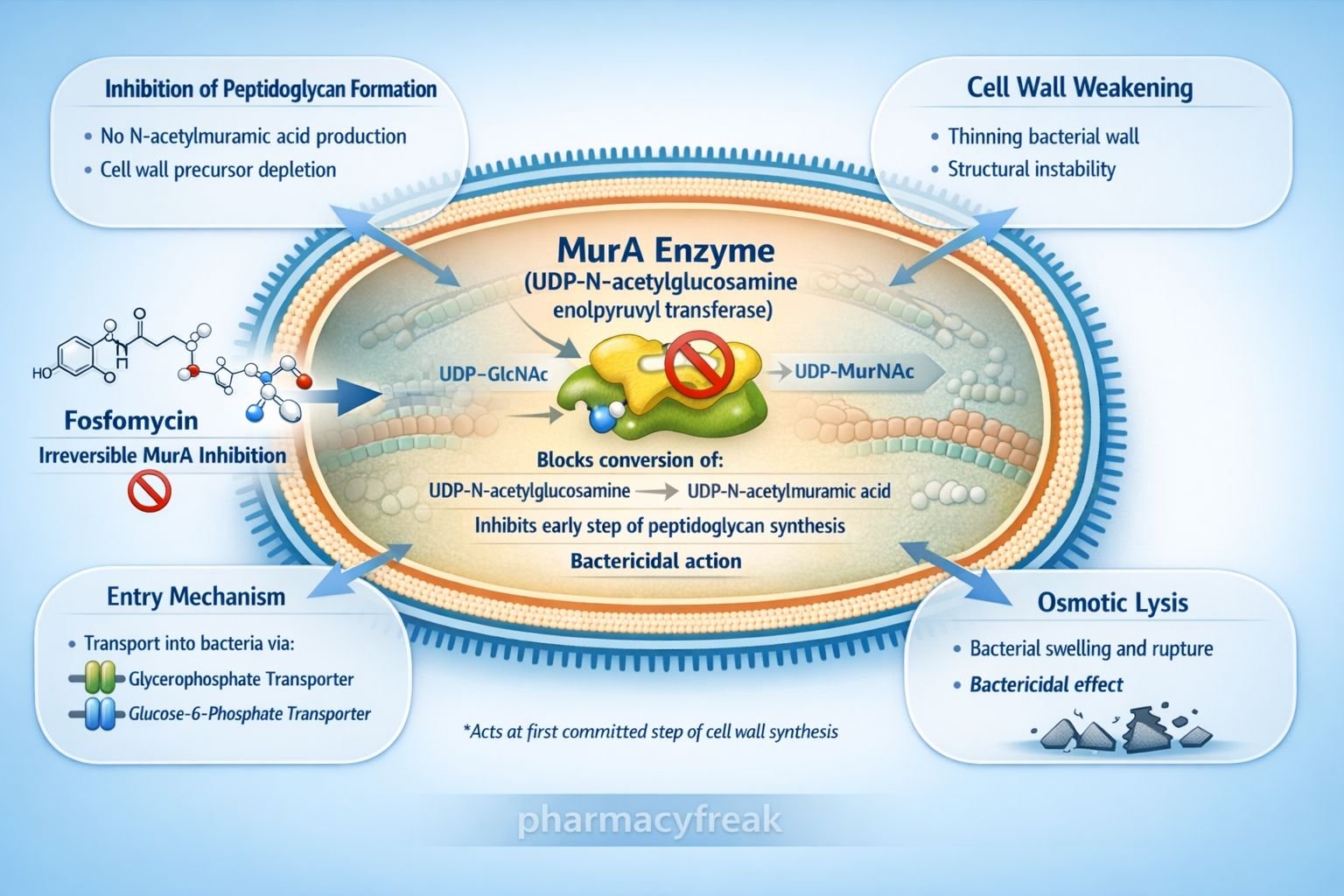
Penicillins: Inhibit bacterial cell wall synthesis by binding to penicillin-binding proteins, leading to cell lysis.
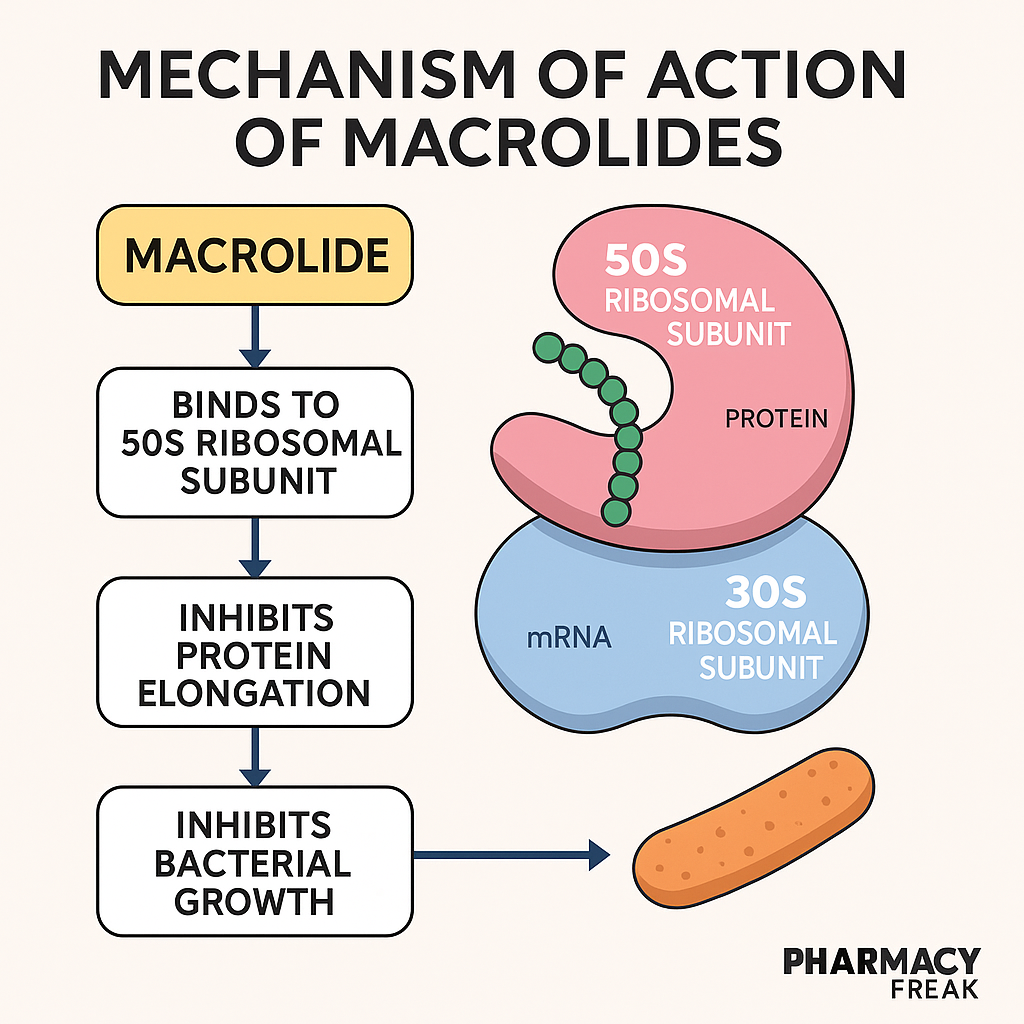
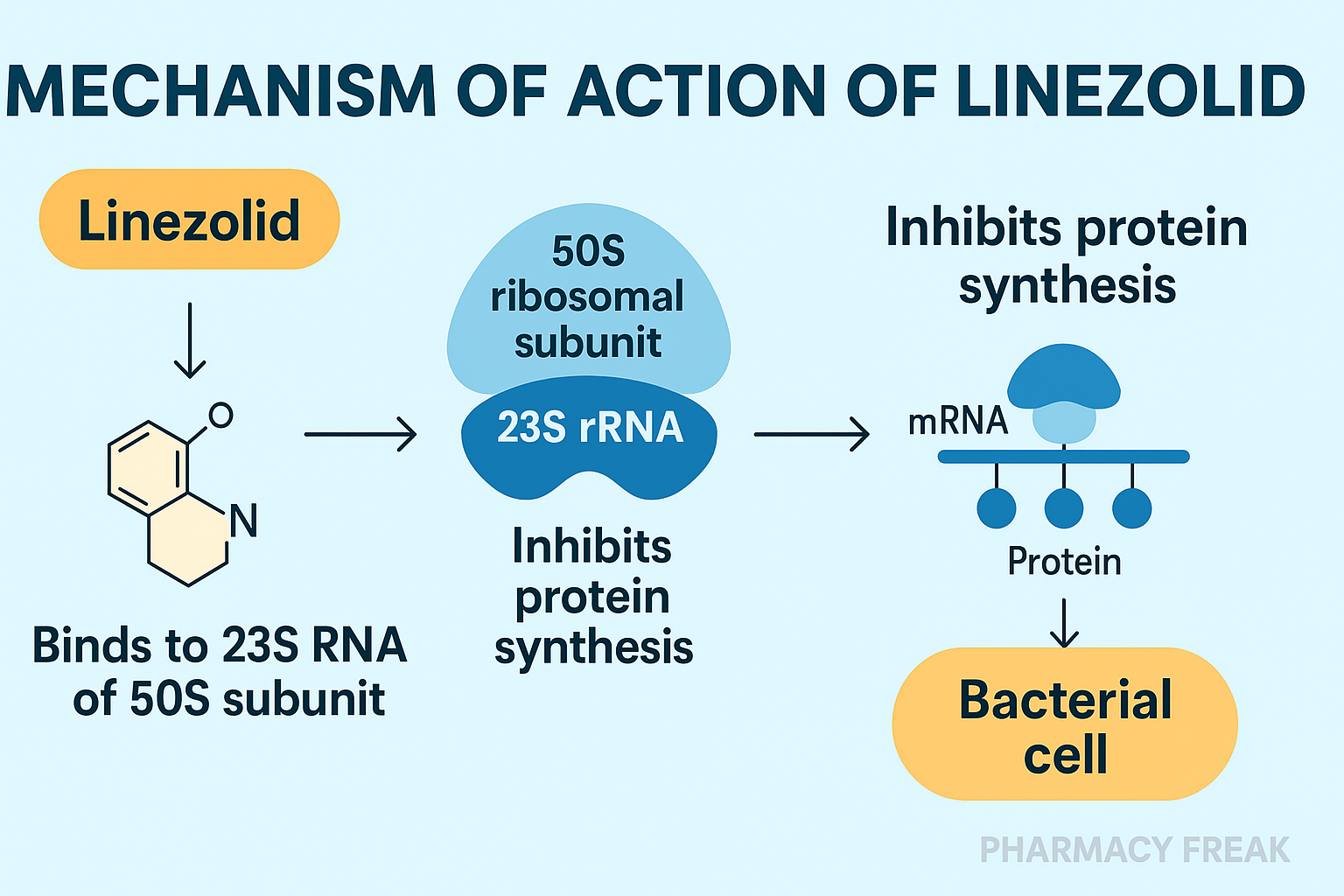
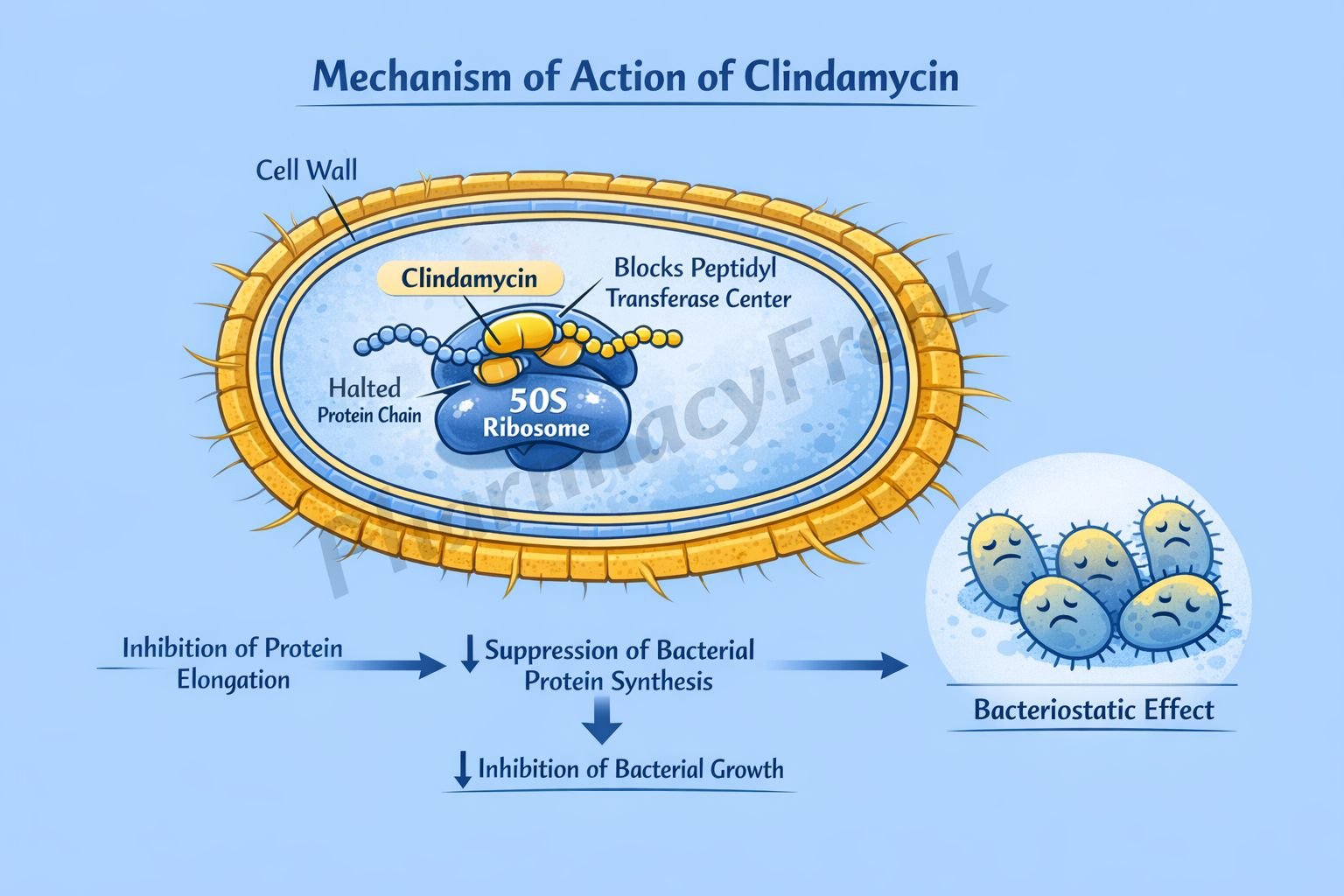
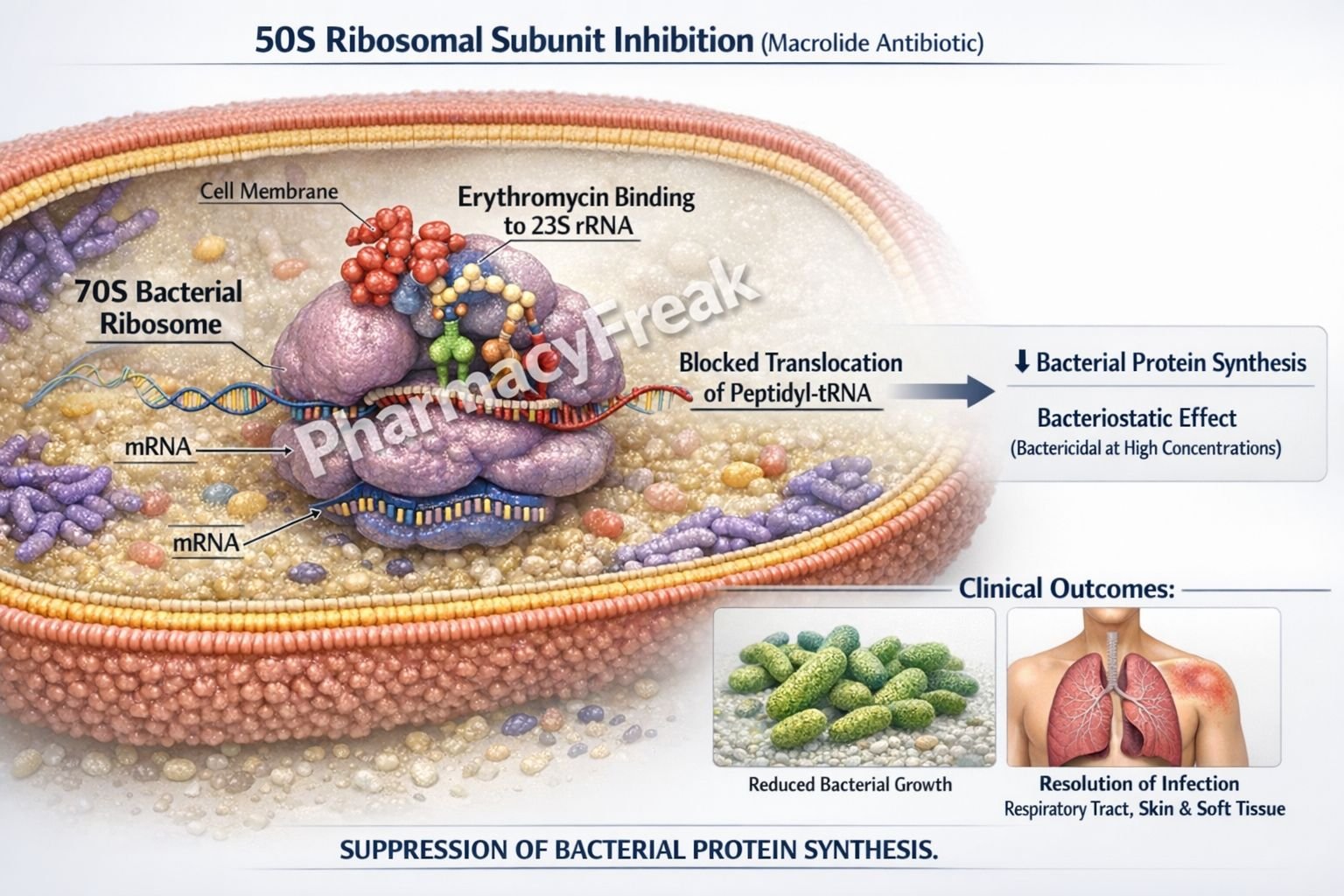
Macrolides (e.g., erythromycin): Inhibit bacterial protein synthesis by binding to the 50S ribosomal subunit.
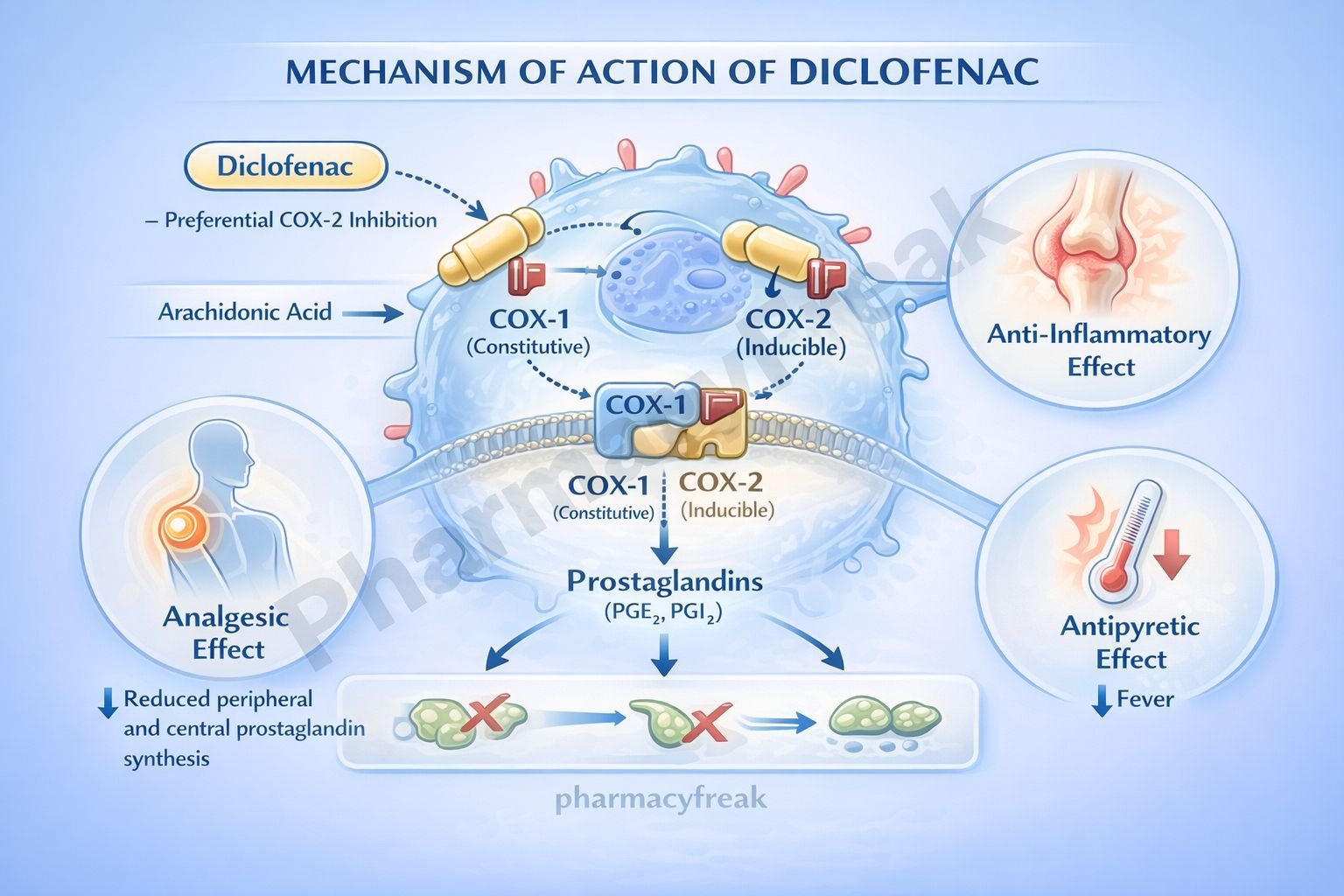
Analgesics
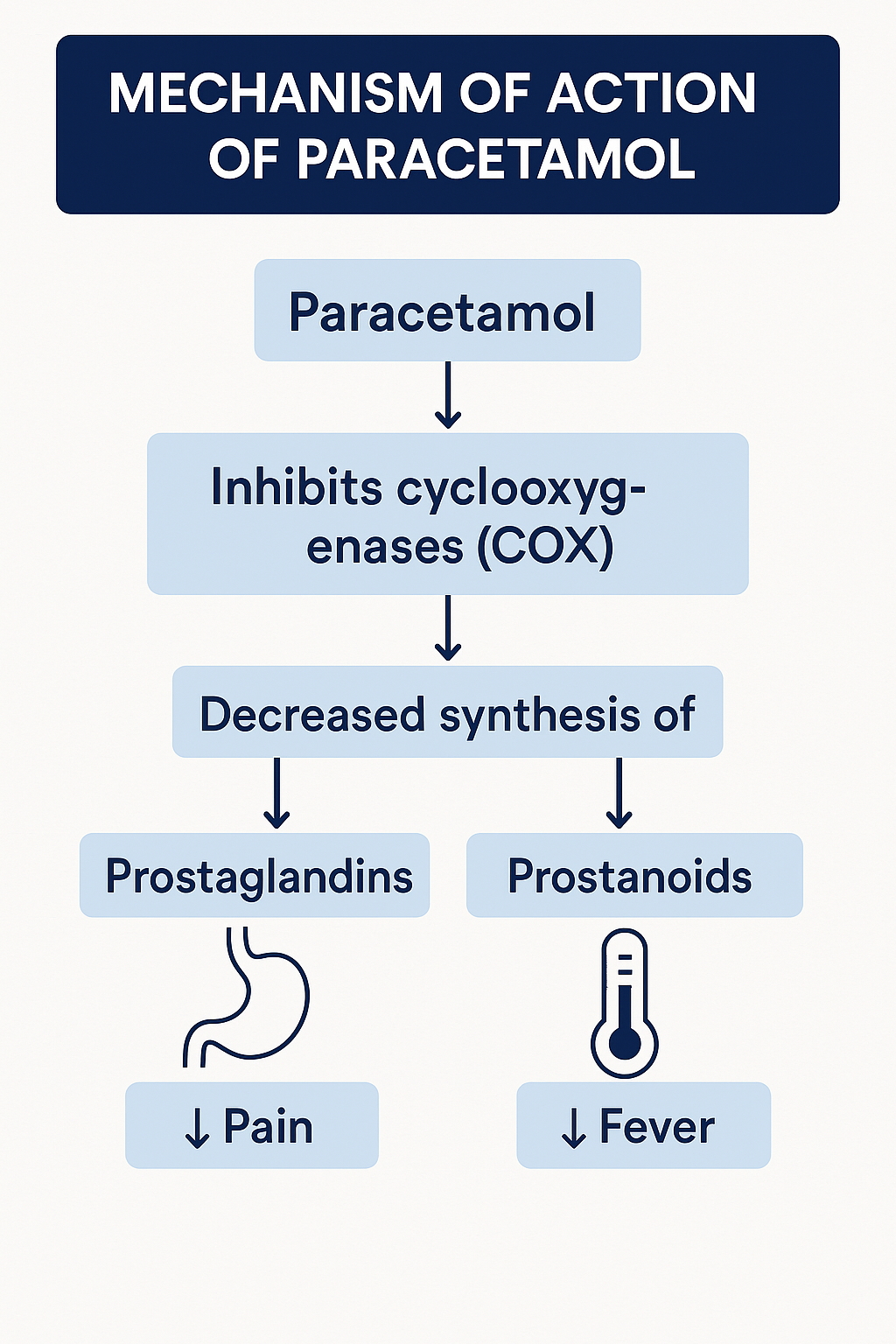
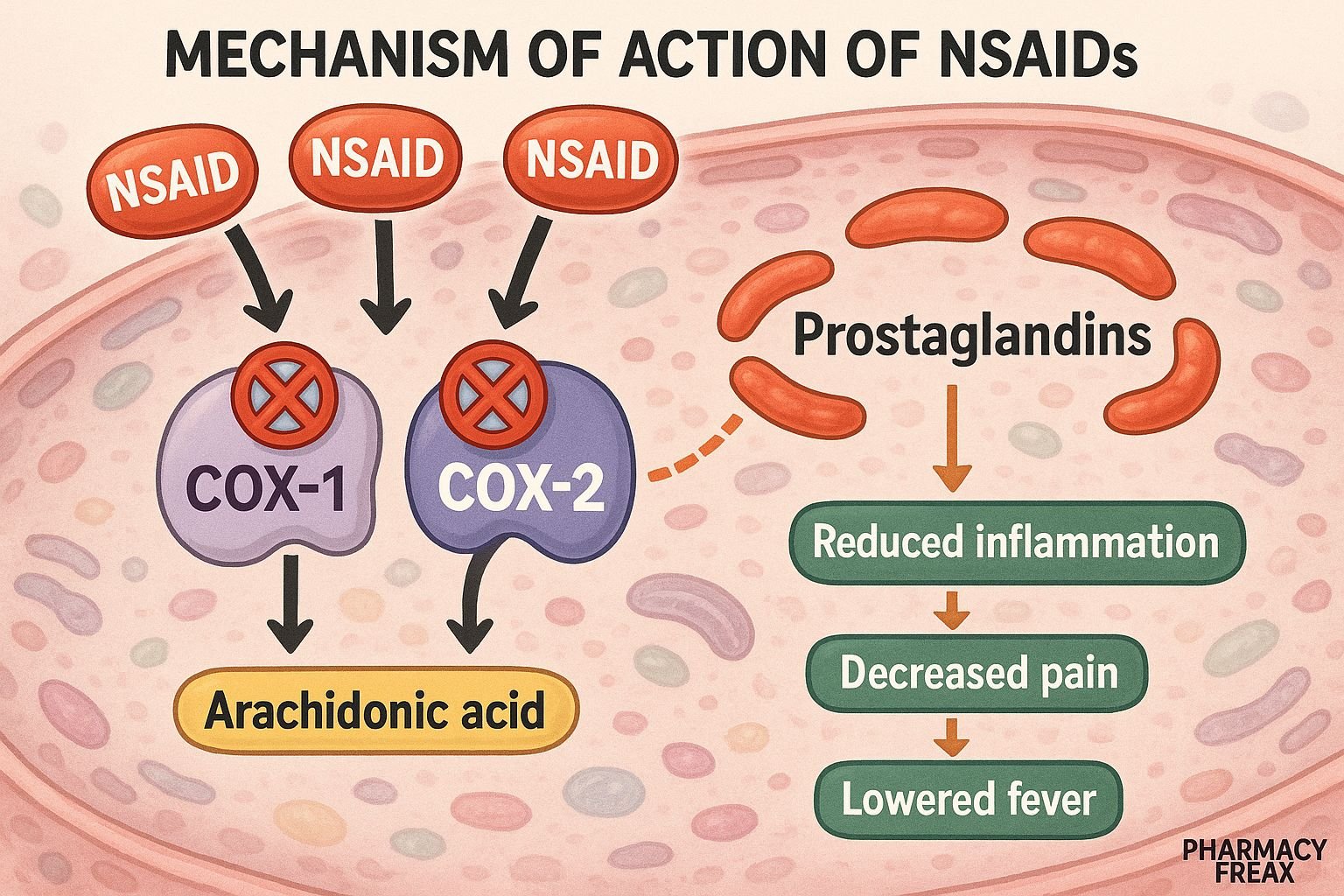
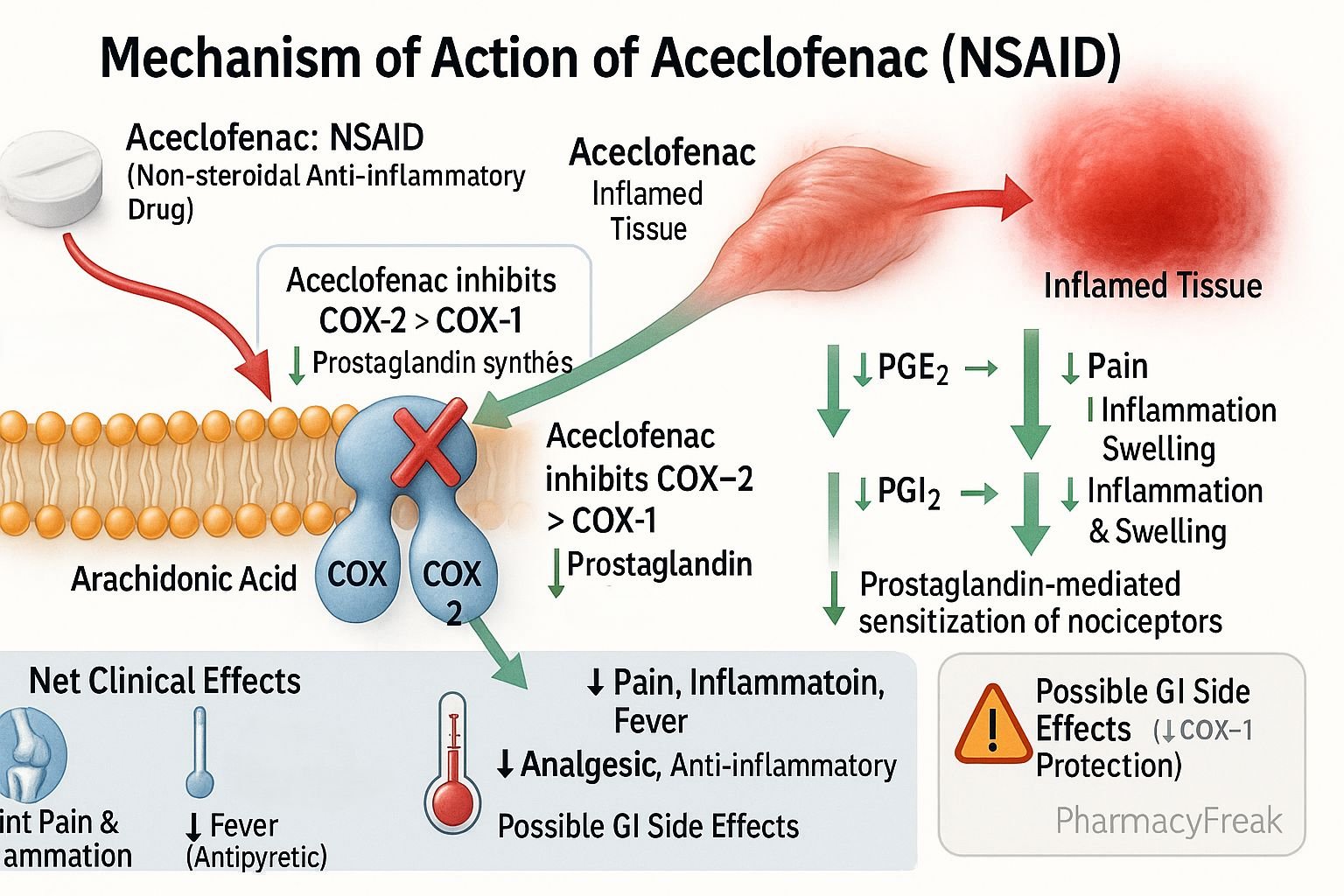
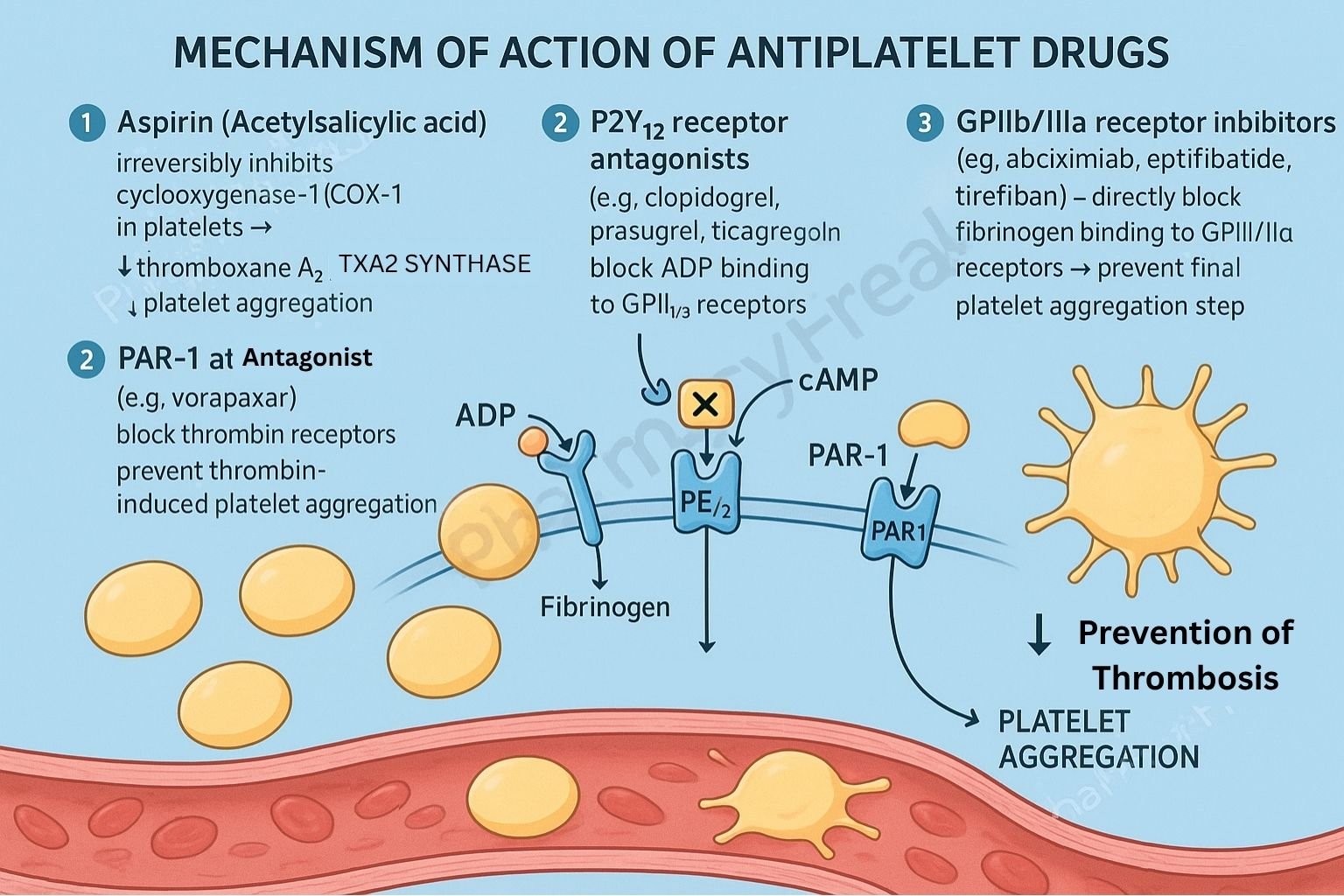
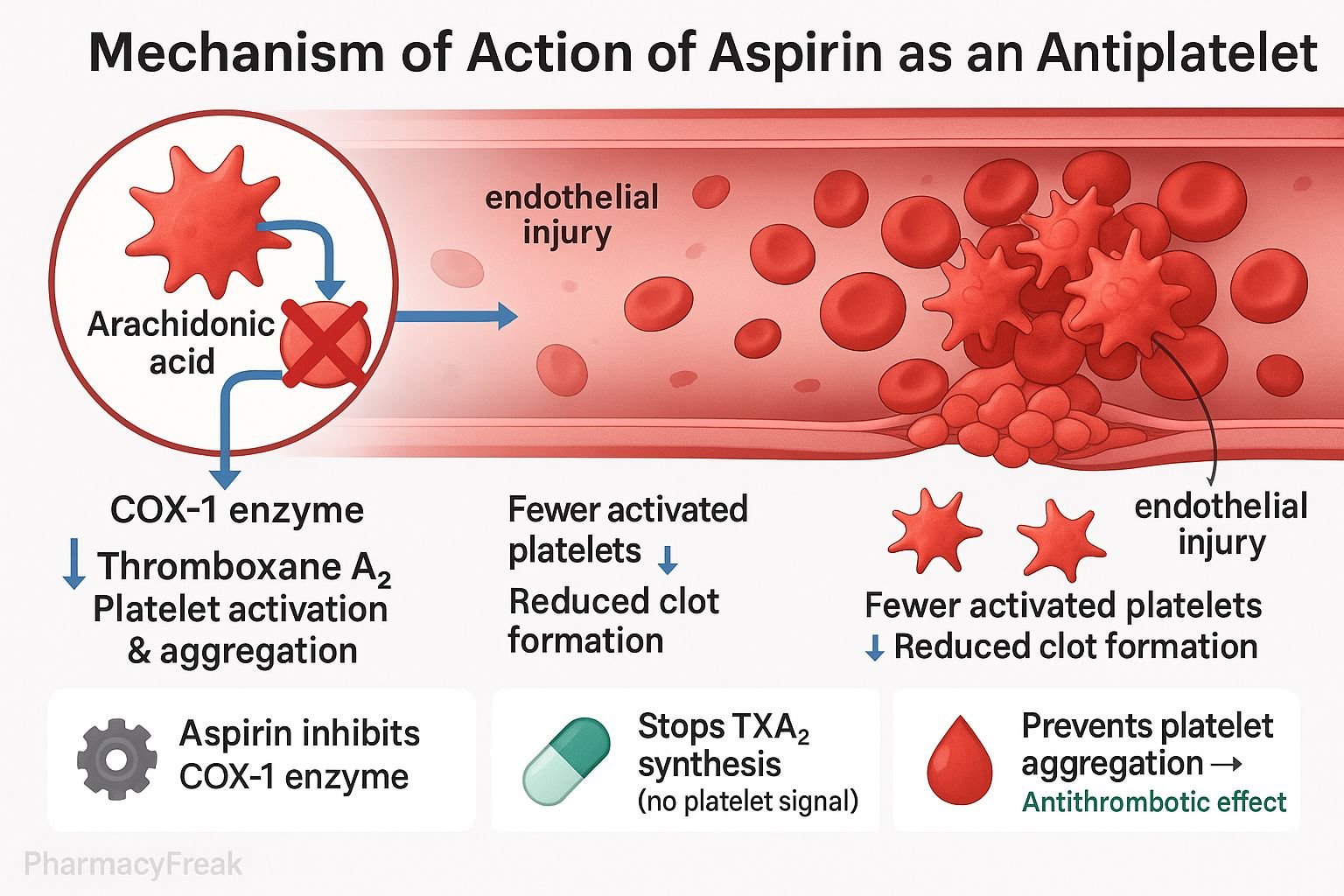
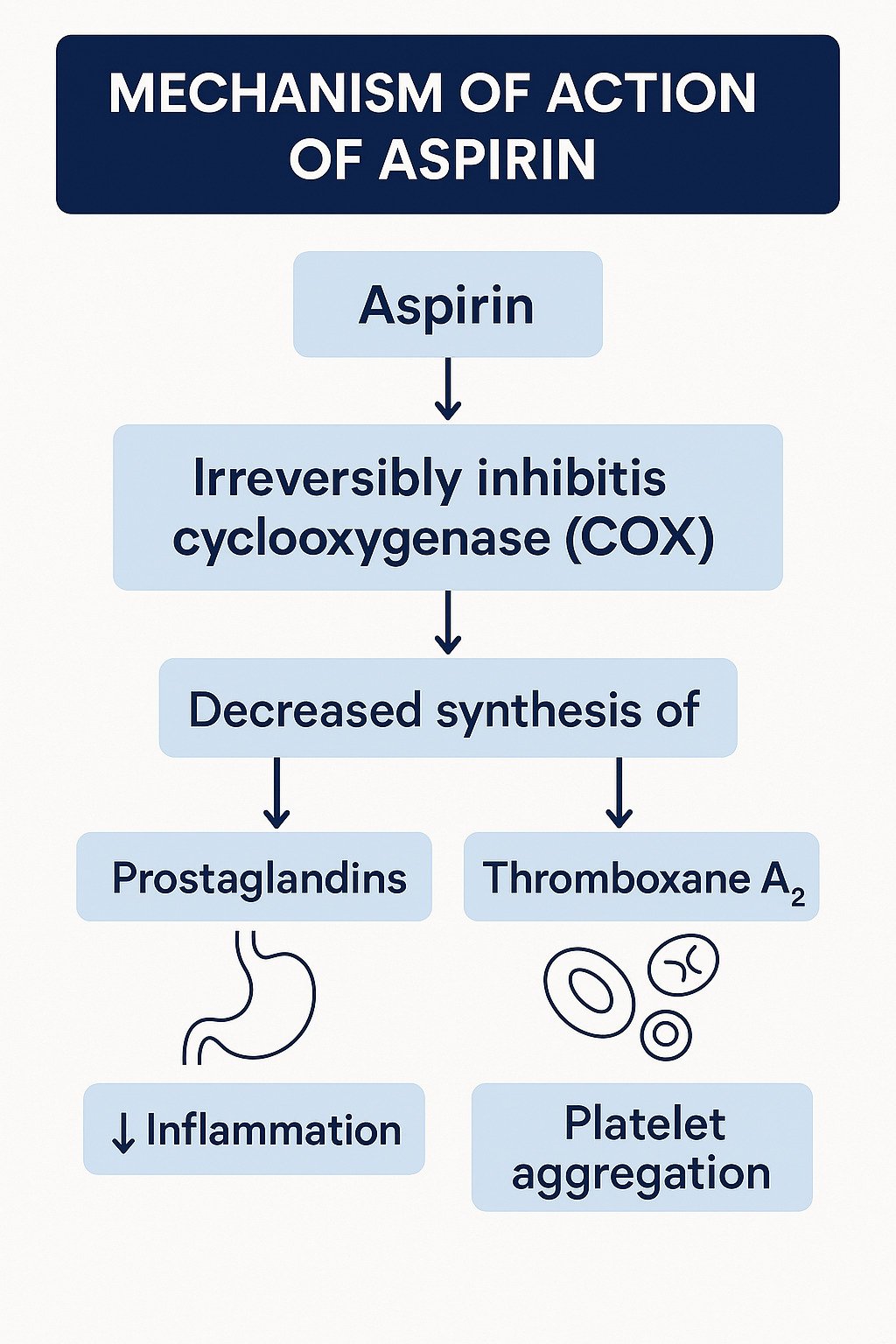
Non-steroidal anti-inflammatory drugs (NSAIDs, e.g., ibuprofen): Inhibit cyclooxygenase enzymes (COX-1 and COX-2), reducing prostaglandin synthesis and inflammation.
Opioids (e.g., morphine): Bind to mu-opioid receptors in the CNS, inhibiting pain pathways.
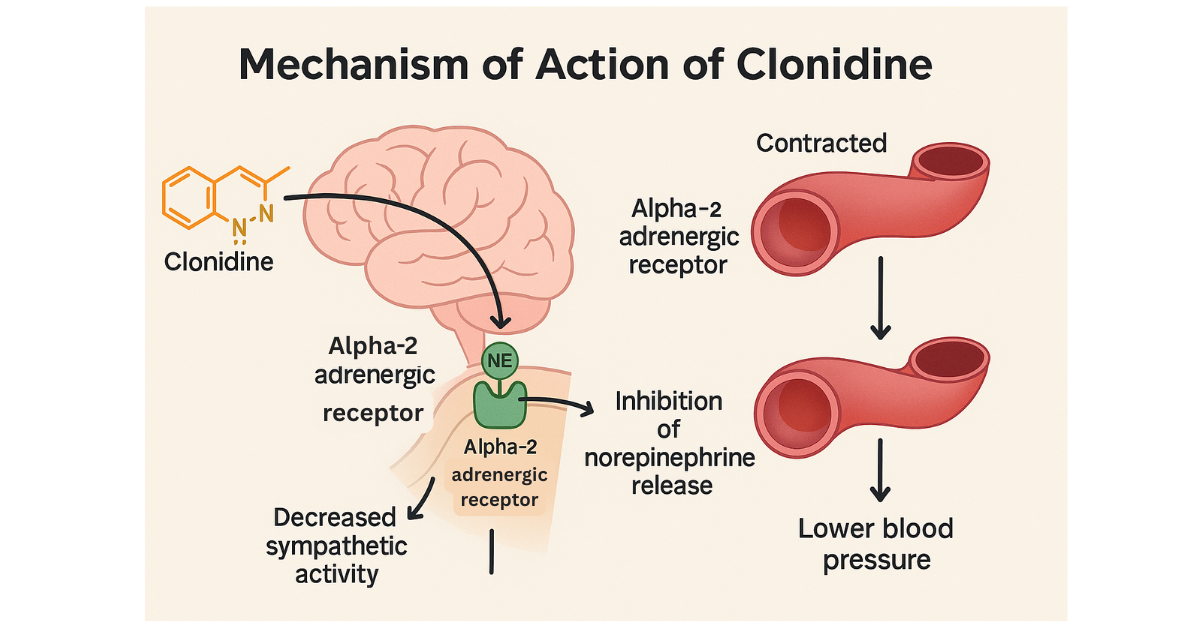
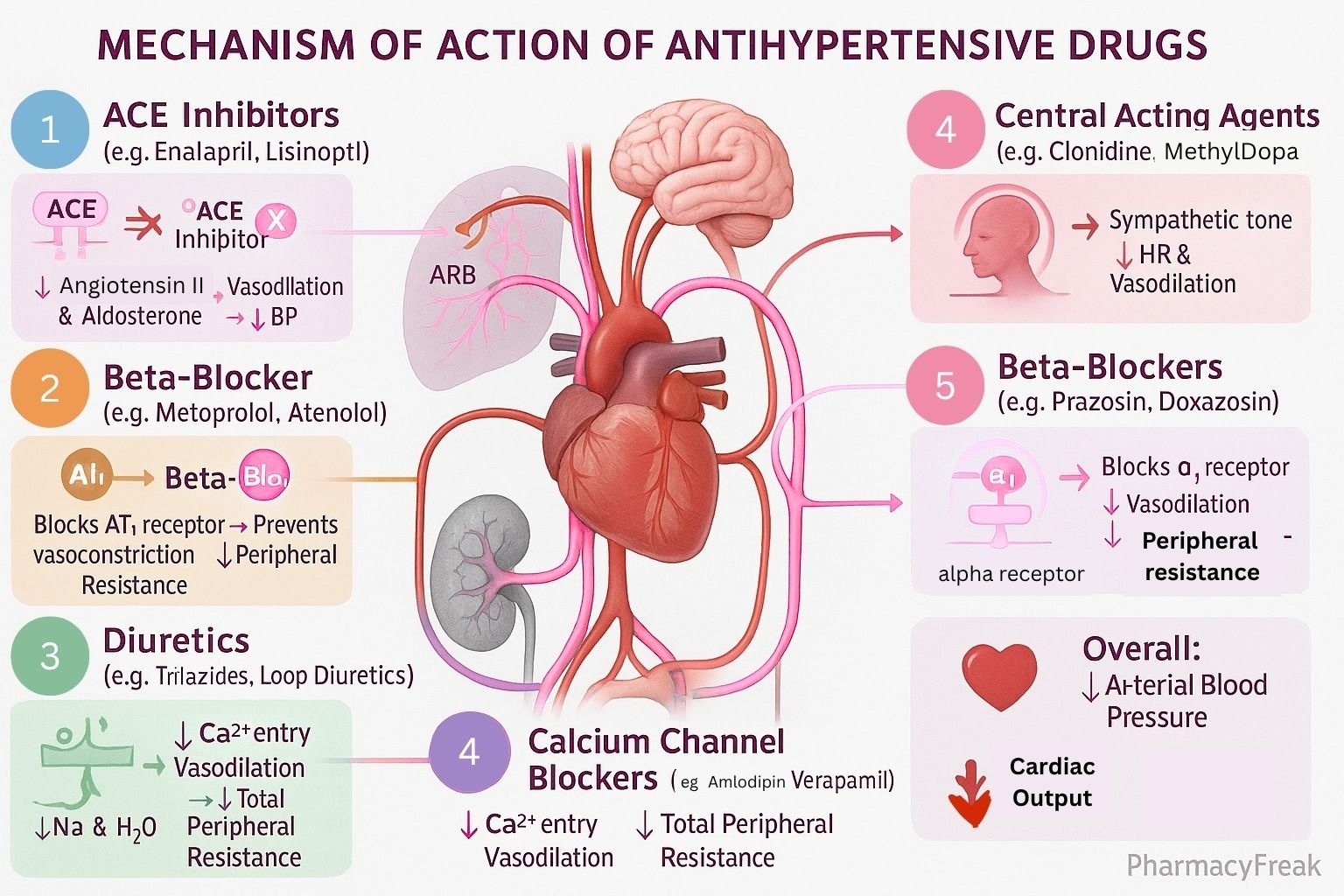
Antihypertensives
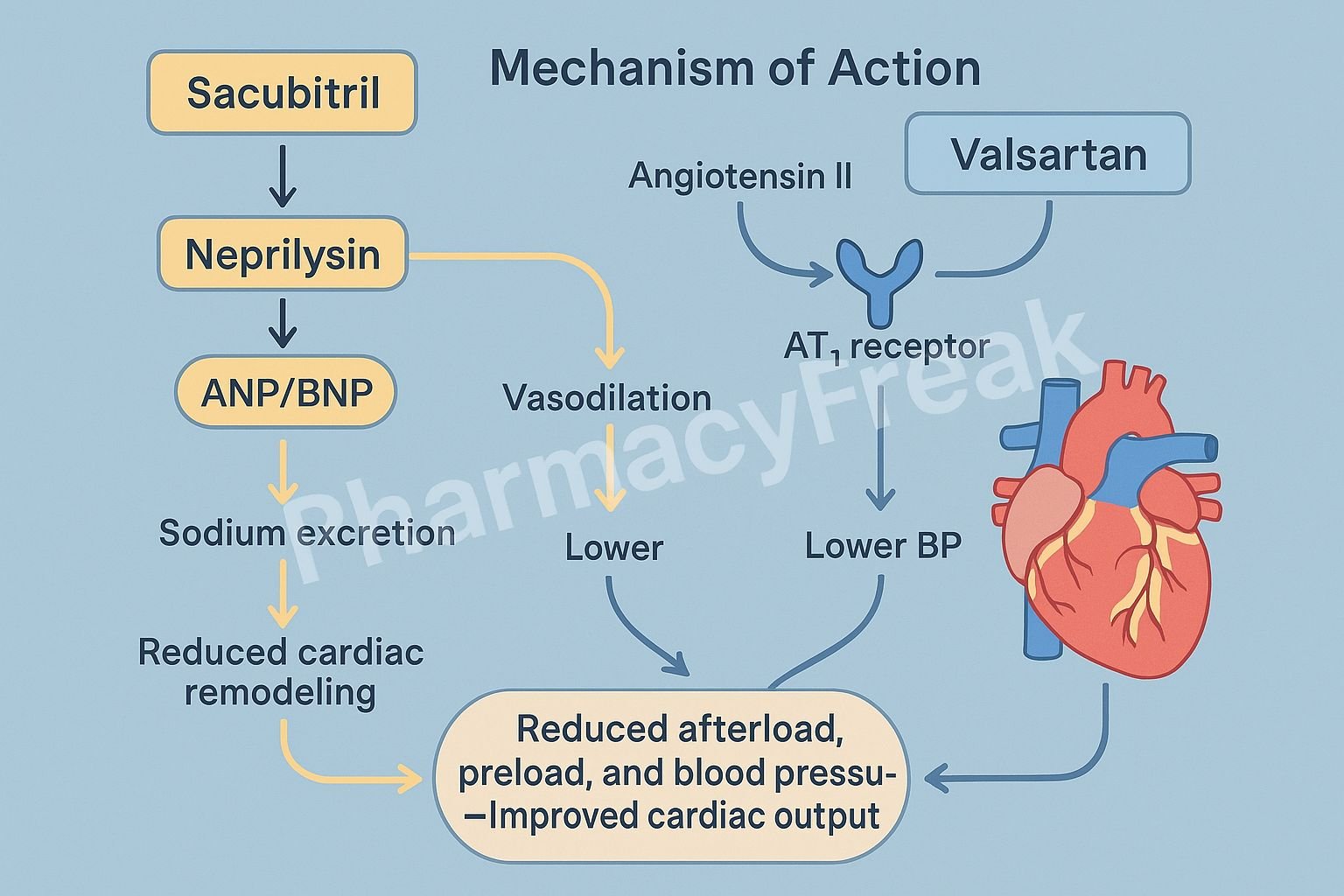
ACE inhibitors (e.g., lisinopril): Inhibit angiotensin-converting enzyme, reducing levels of angiotensin II and causing vasodilation.
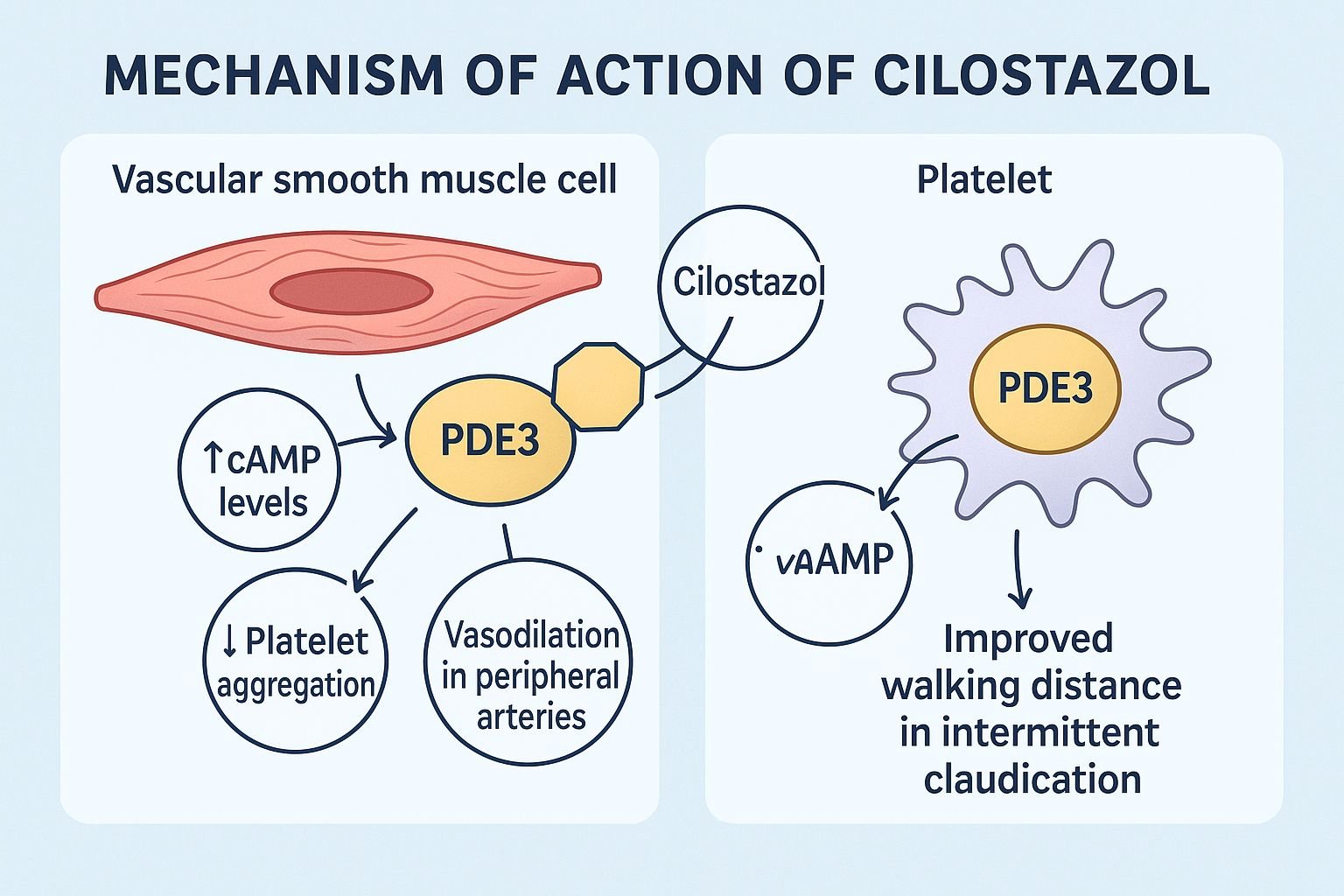
Calcium channel blockers (e.g., diltiazem): Prevent calcium entry into vascular smooth muscle, reducing contractility and blood pressure.
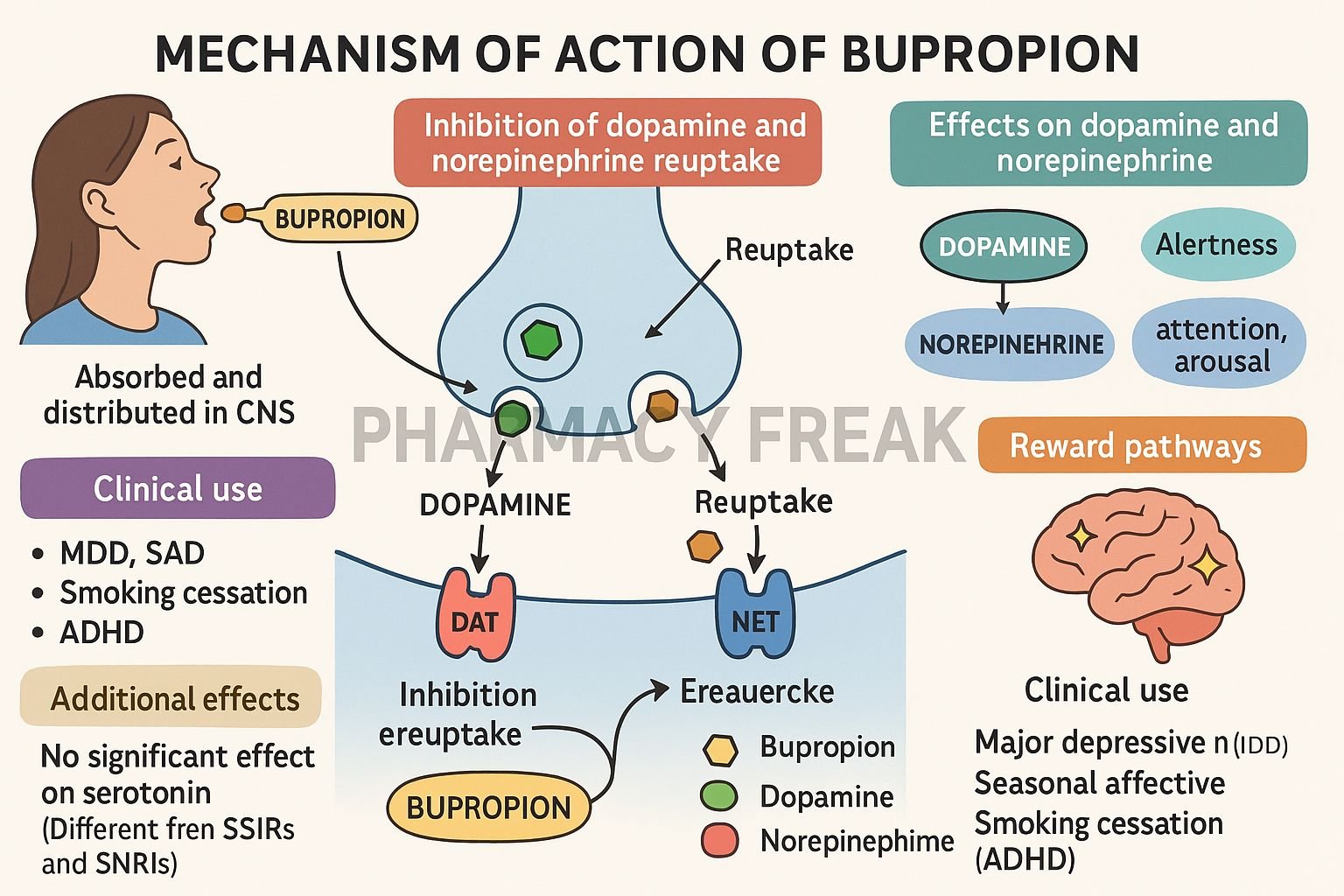
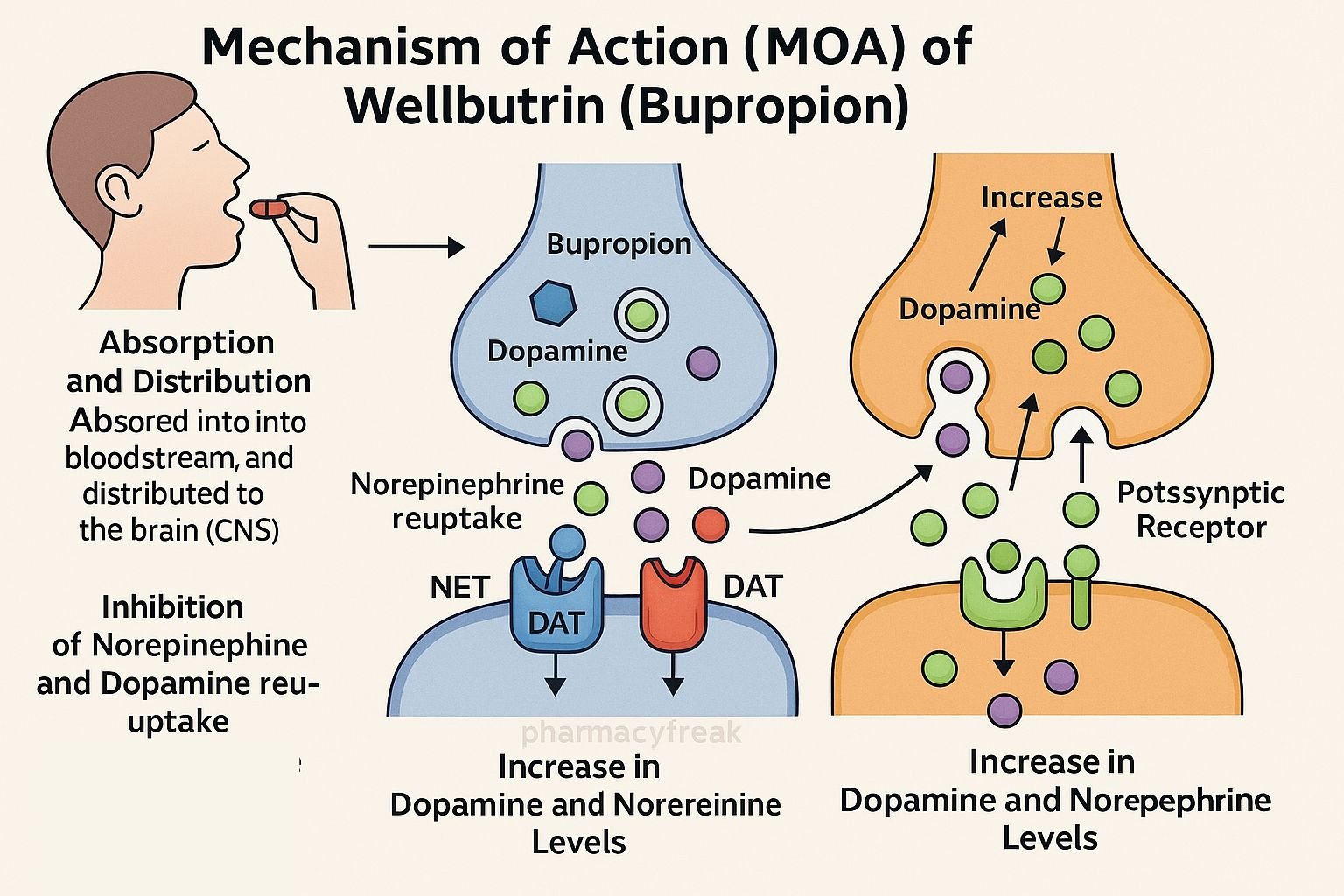
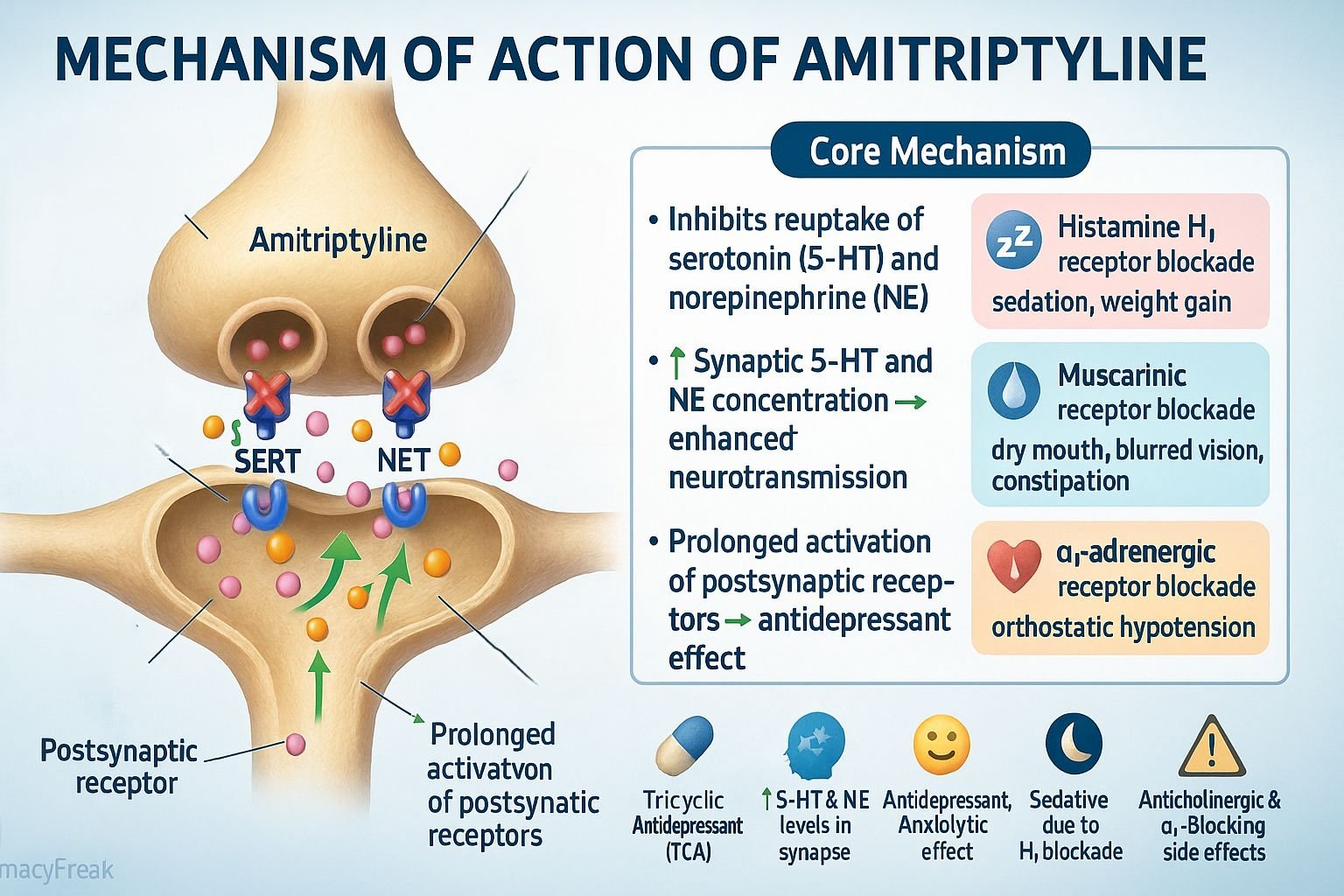
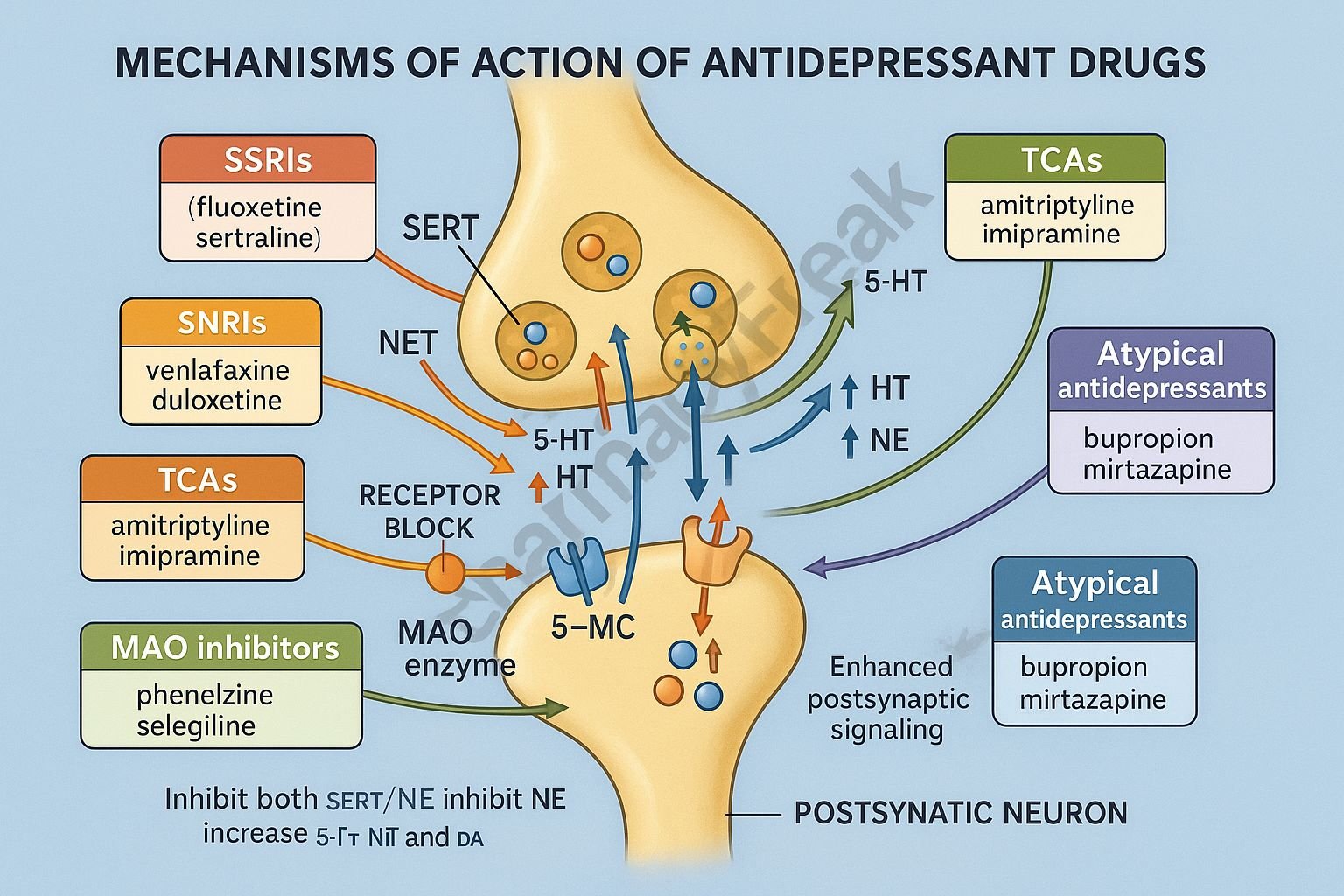
Antidepressants
SSRIs (e.g., sertraline): Block serotonin reuptake, increasing serotonin in synaptic spaces.
Tricyclic antidepressants: Inhibit the reuptake of both norepinephrine and serotonin.
Clinical Applications: Why Mechanism of Action Matters
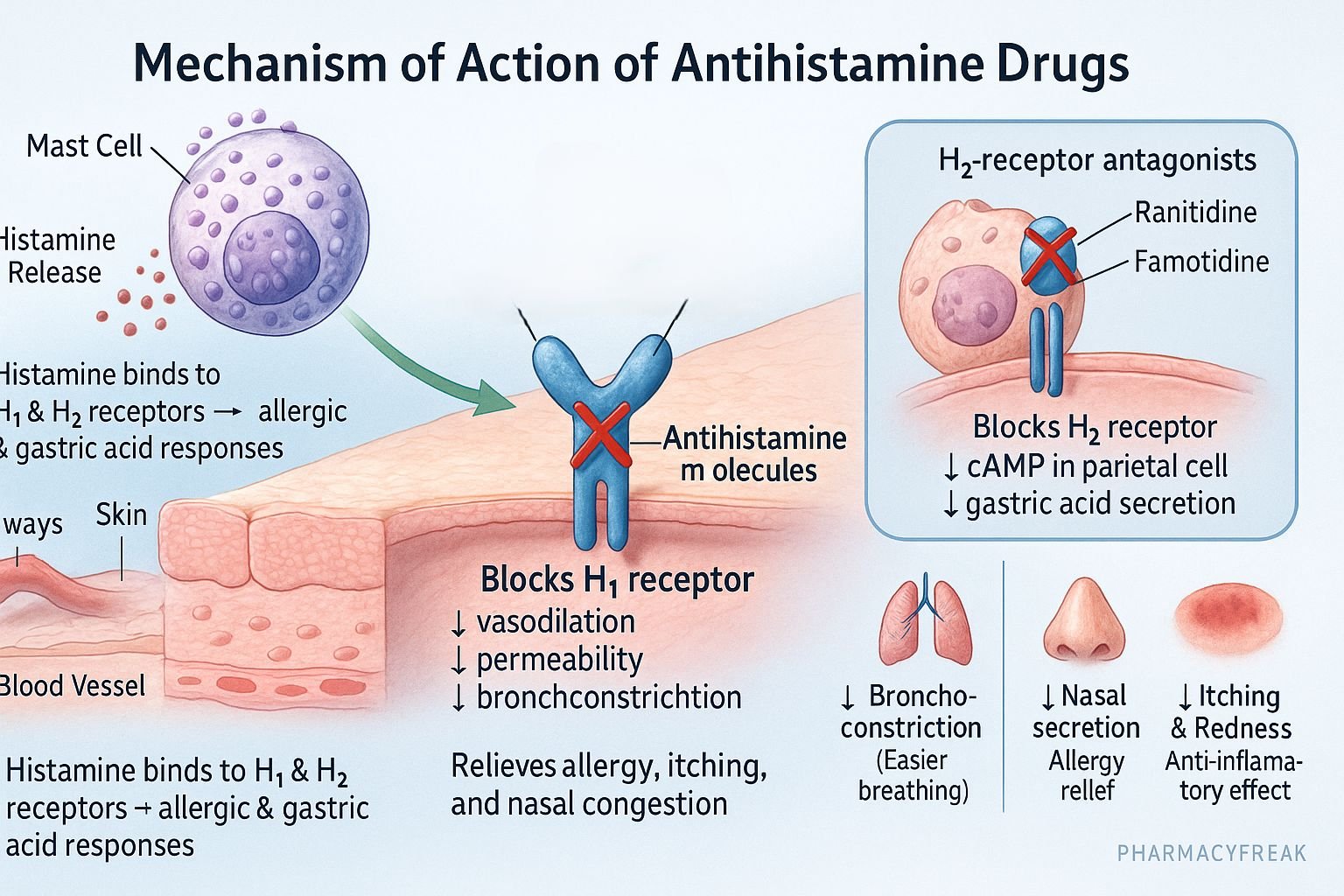
Predicting Side Effects
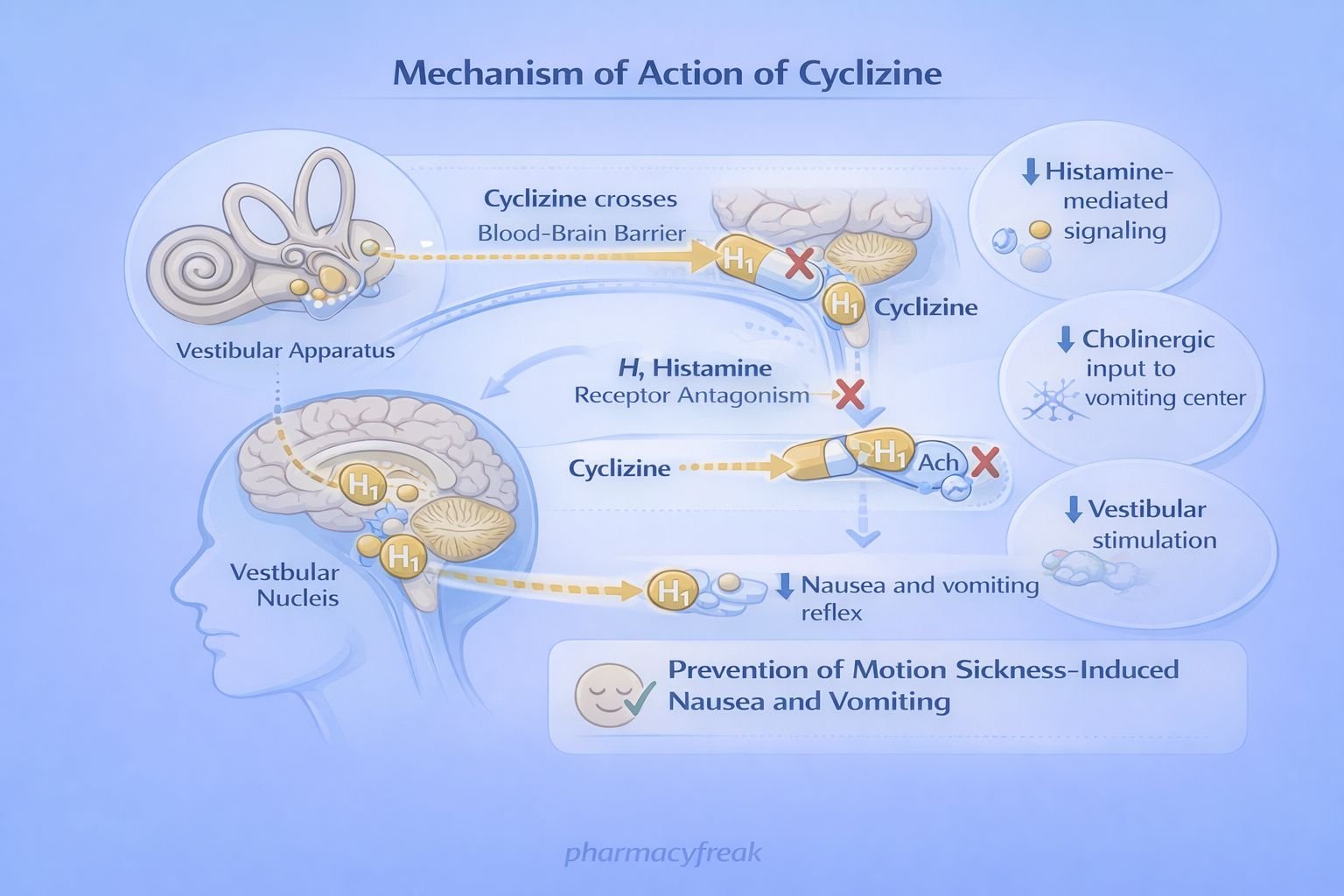
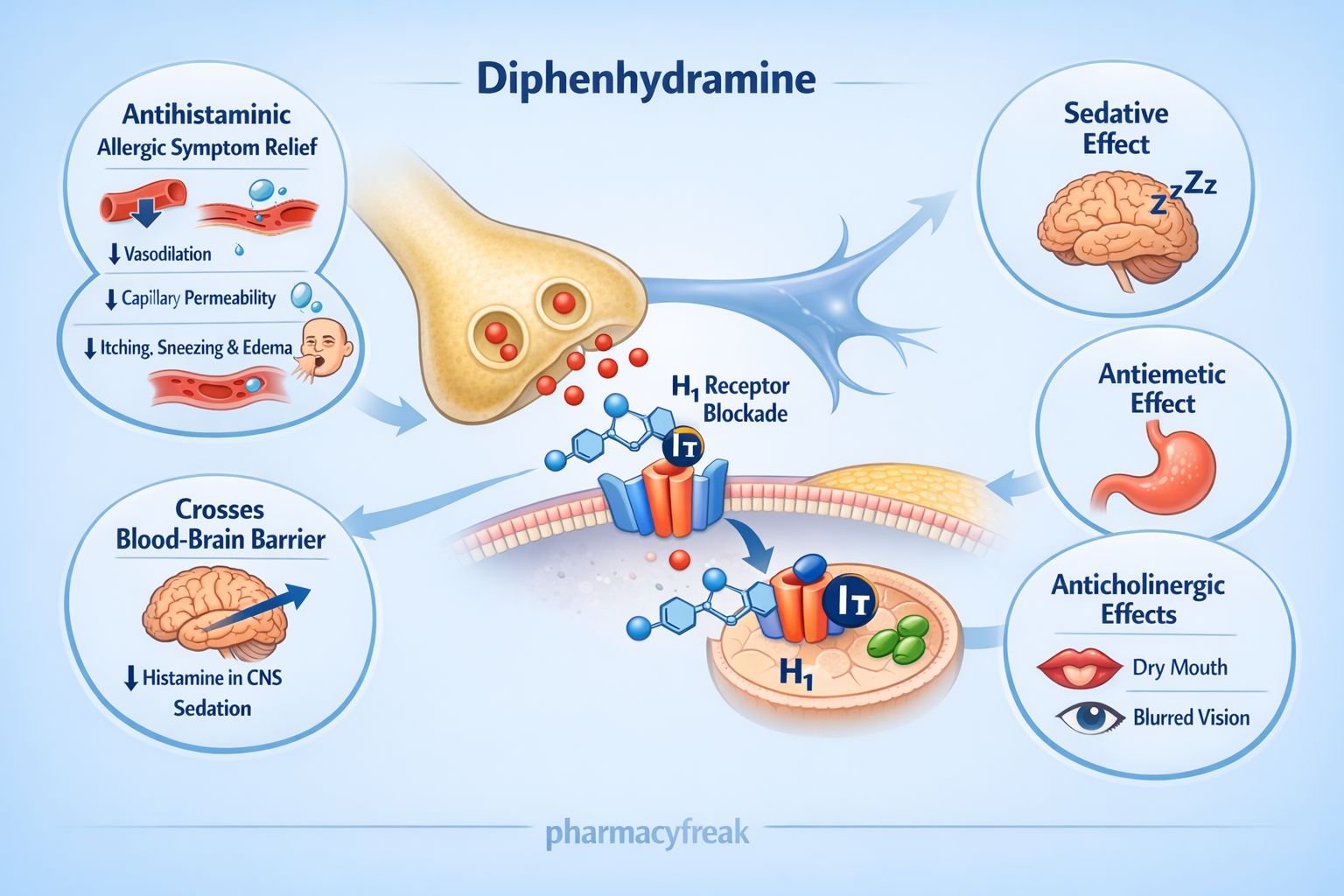
Side effects often result from drug action at unintended sites or receptors. For example, antihistamines that cross the blood-brain barrier can cause sedation because they also block histamine receptors in the brain.
Choosing the Right Drug
If two drugs treat the same condition but have different mechanisms, understanding MOA can help select the best drug based on patient factors and comorbidities.
Managing Drug Resistance
Knowing how antibiotics work helps explain why resistance develops. For example, bacteria may alter target proteins or produce enzymes that destroy the drug.
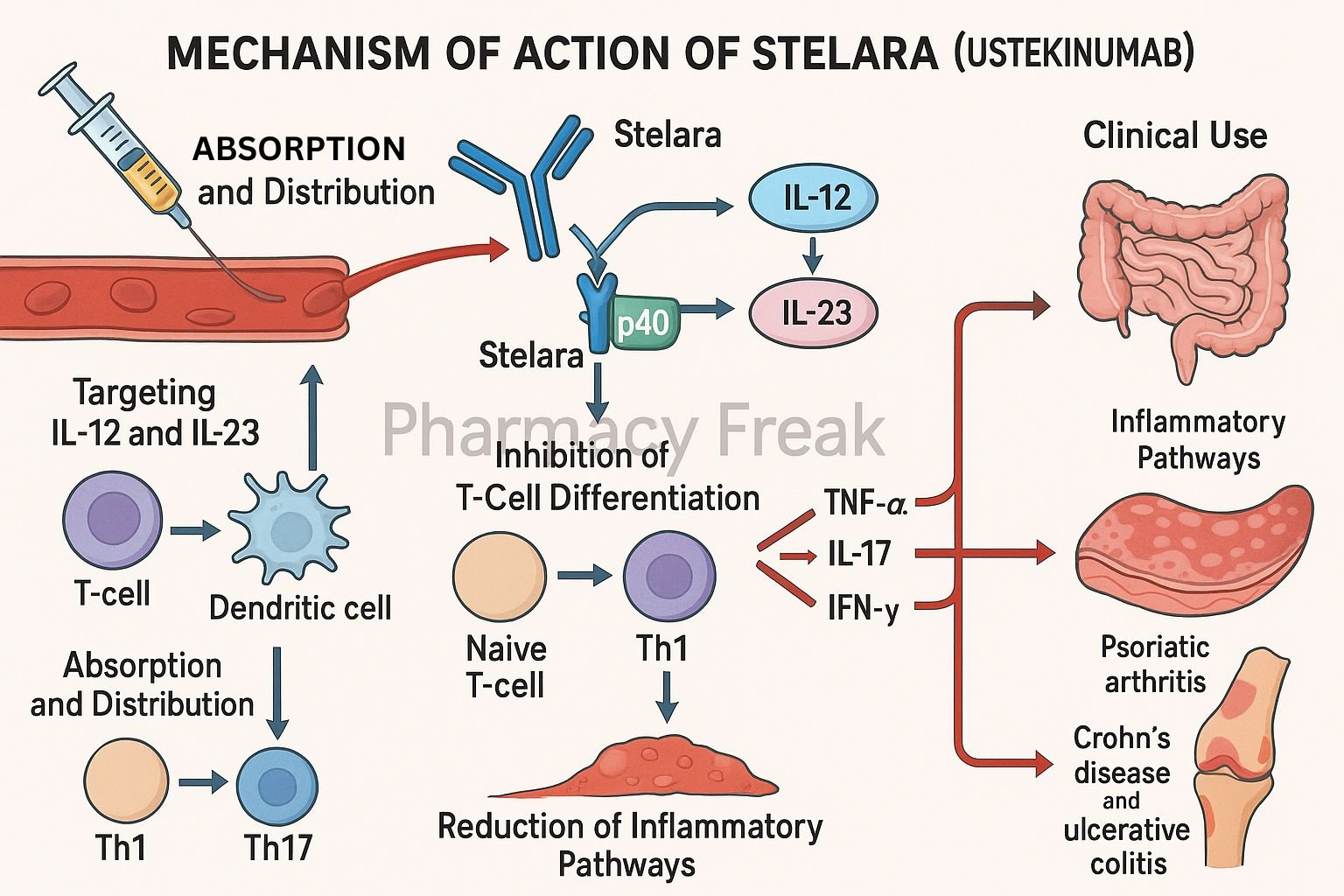
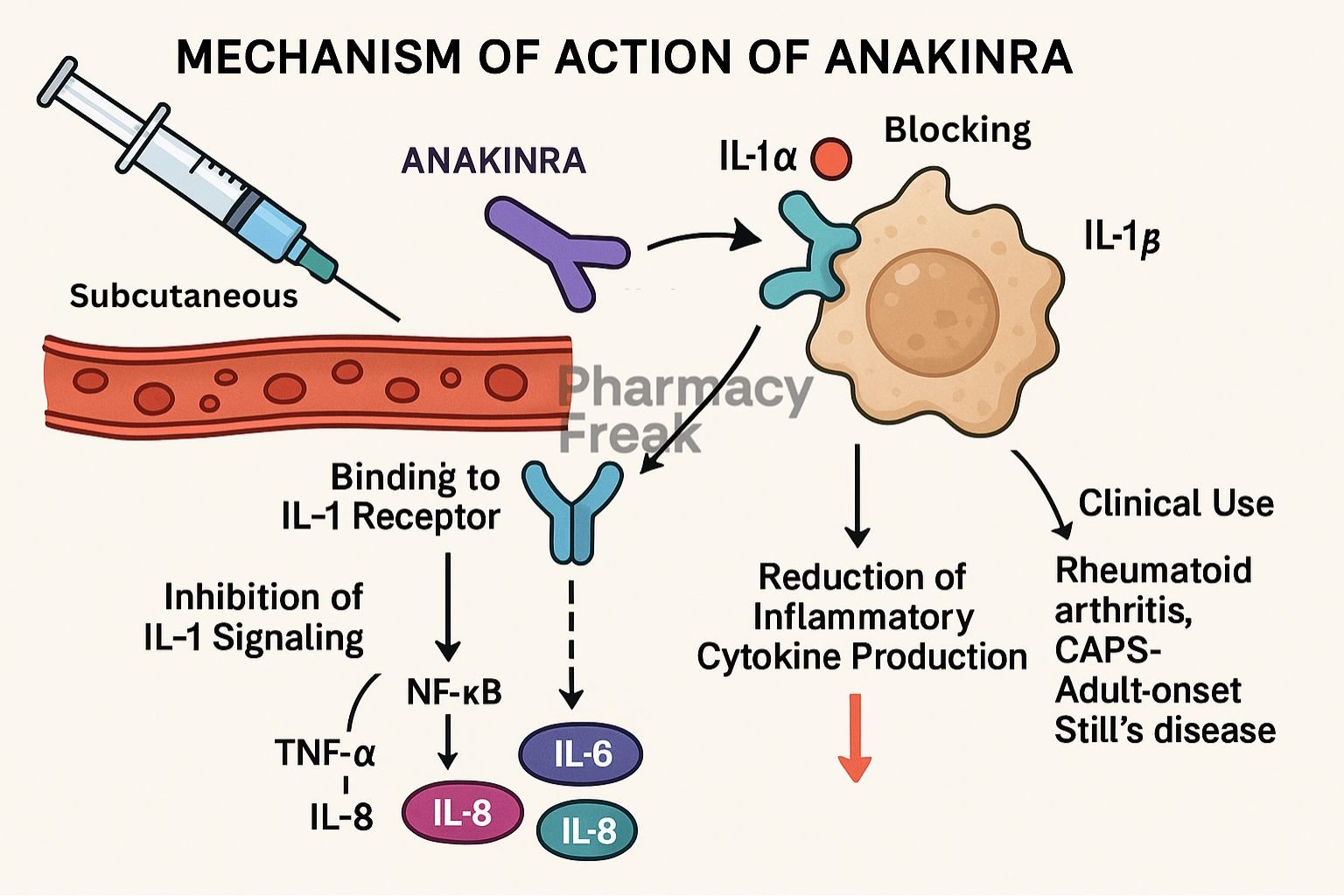
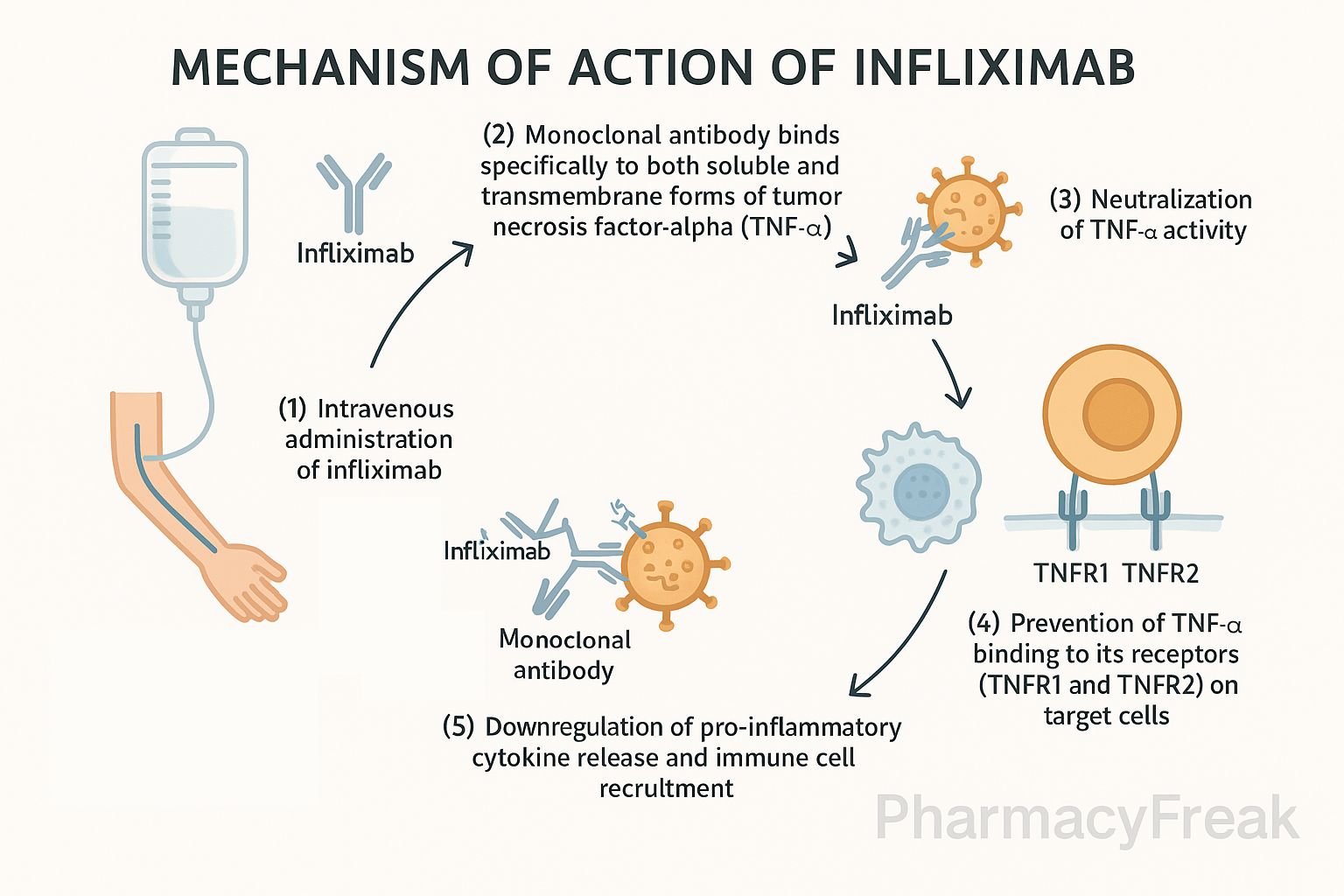
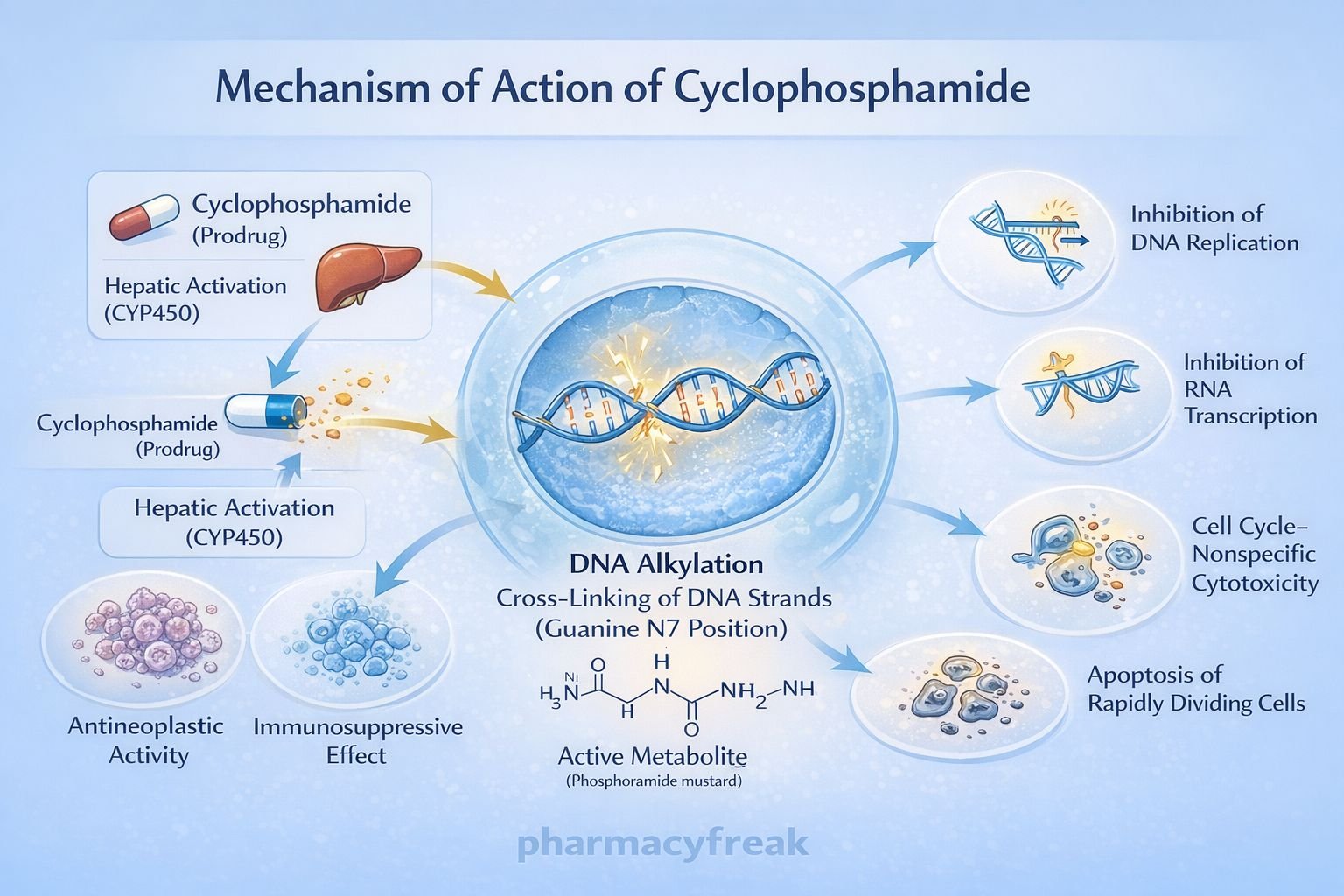
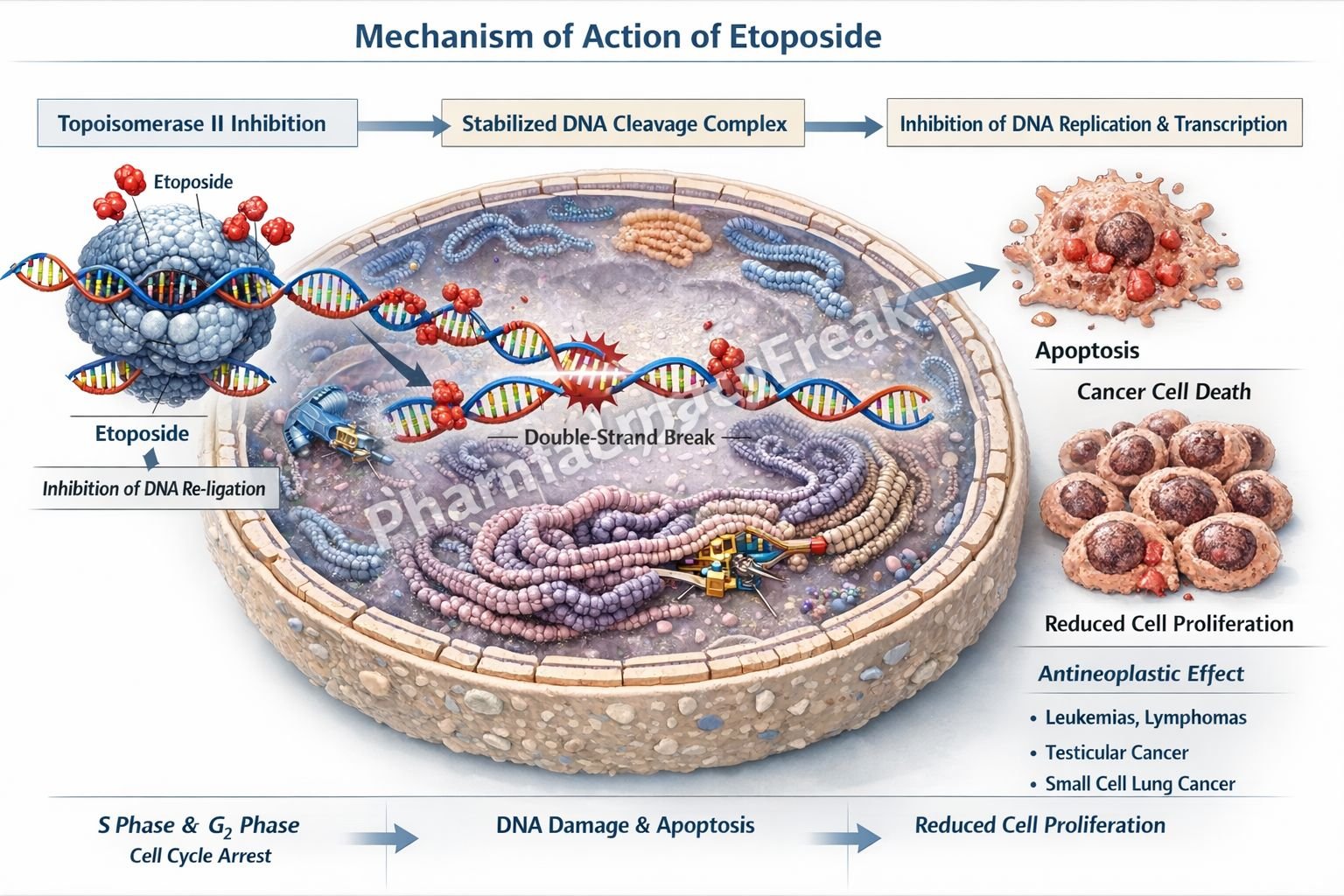
Drug Development
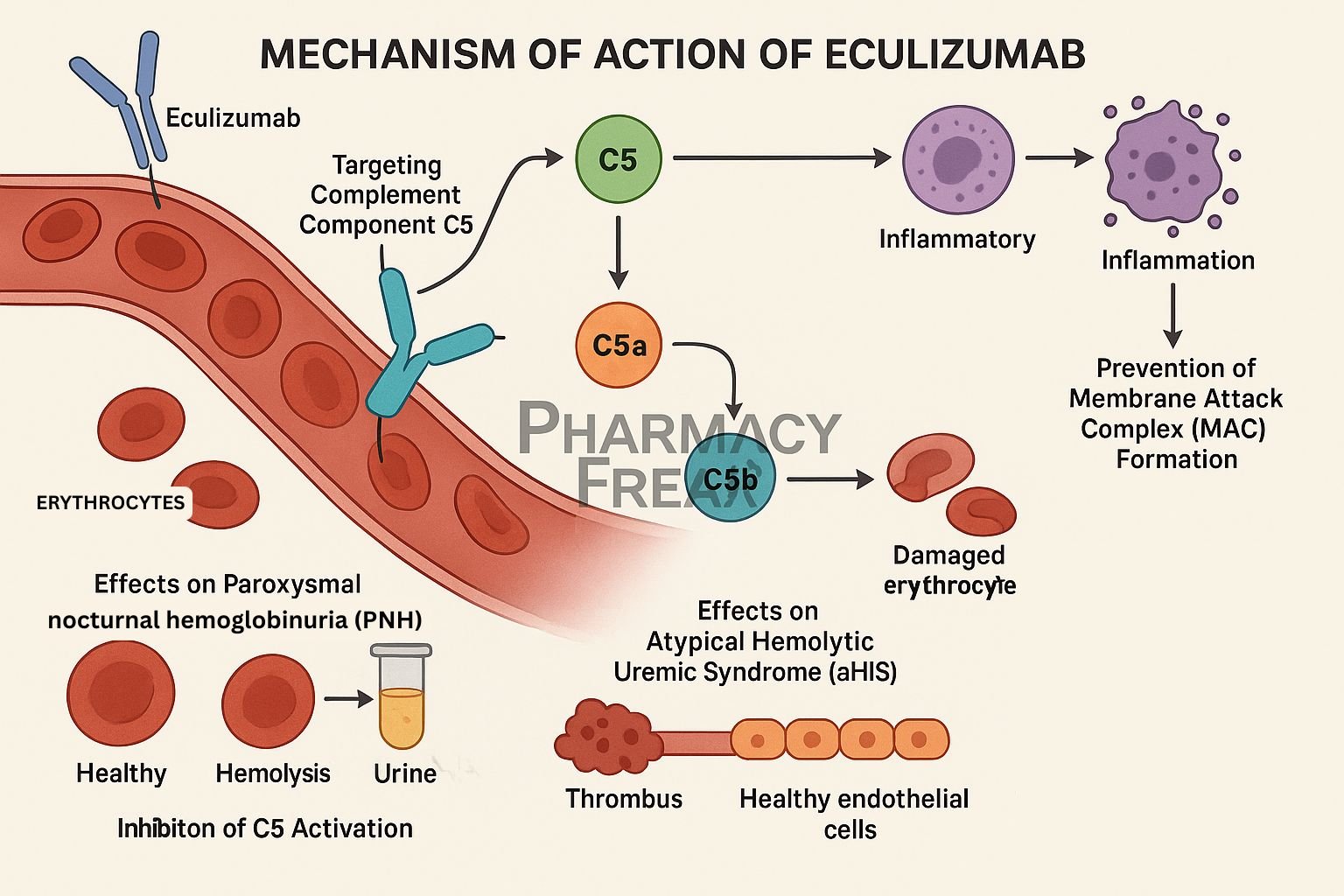
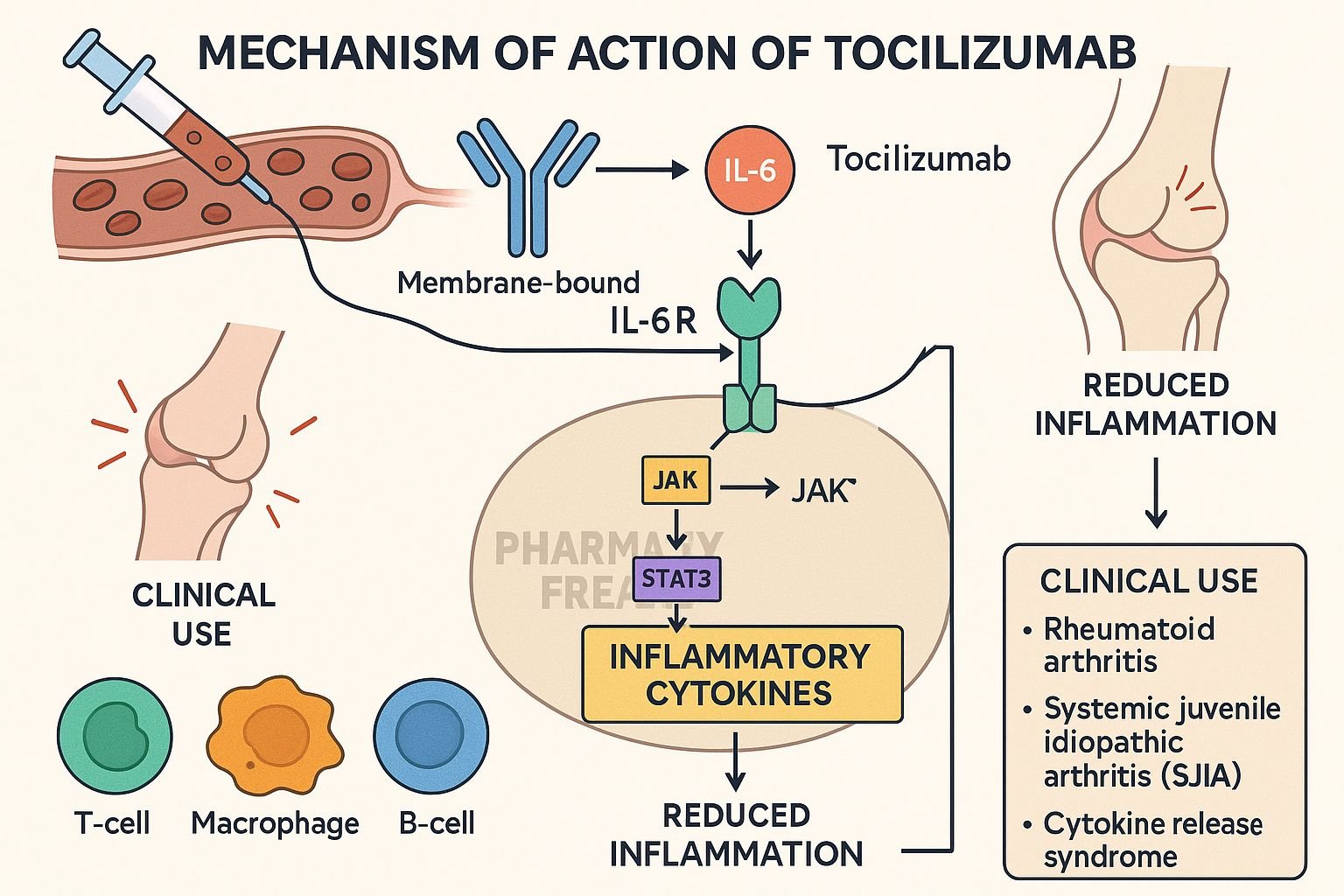
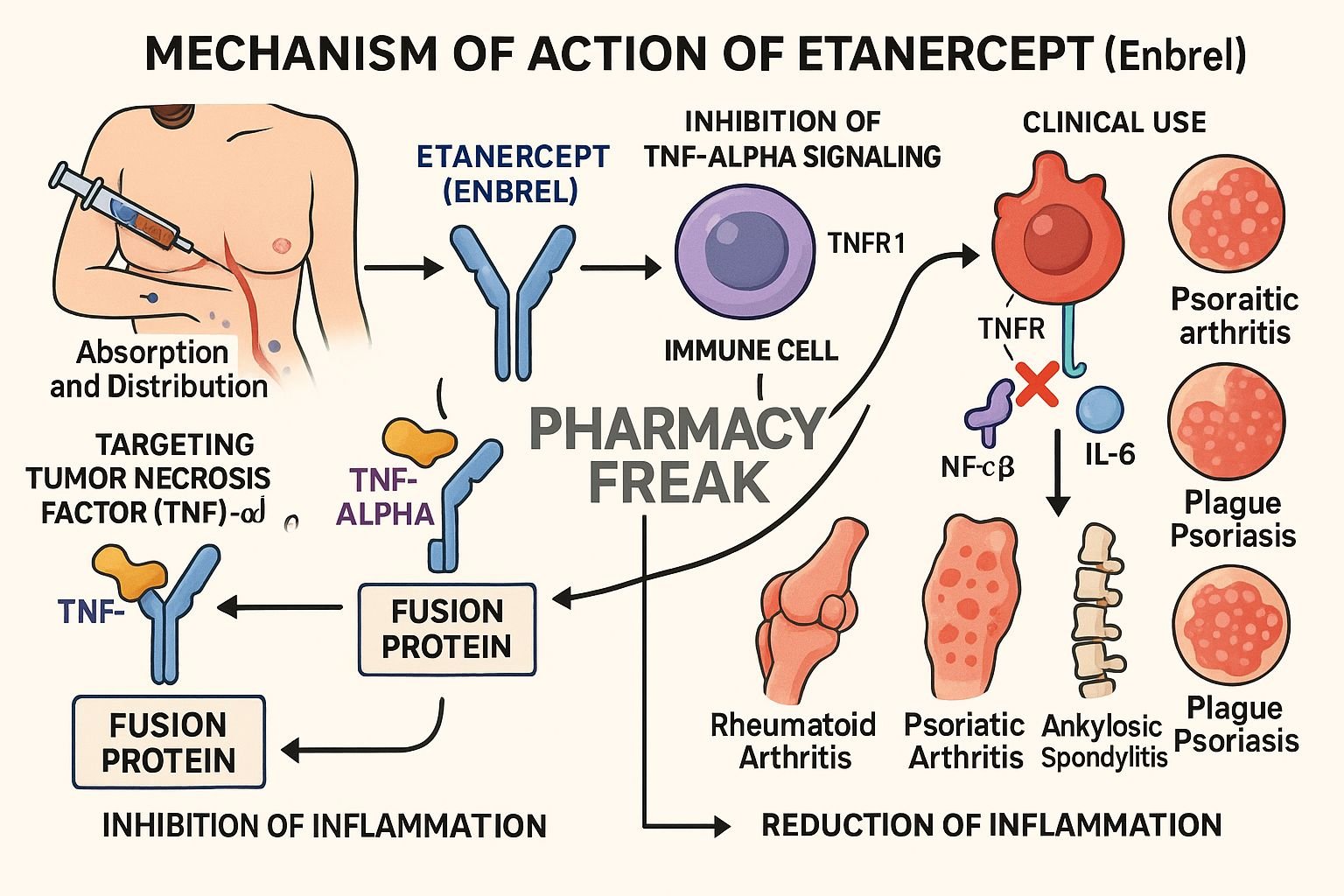
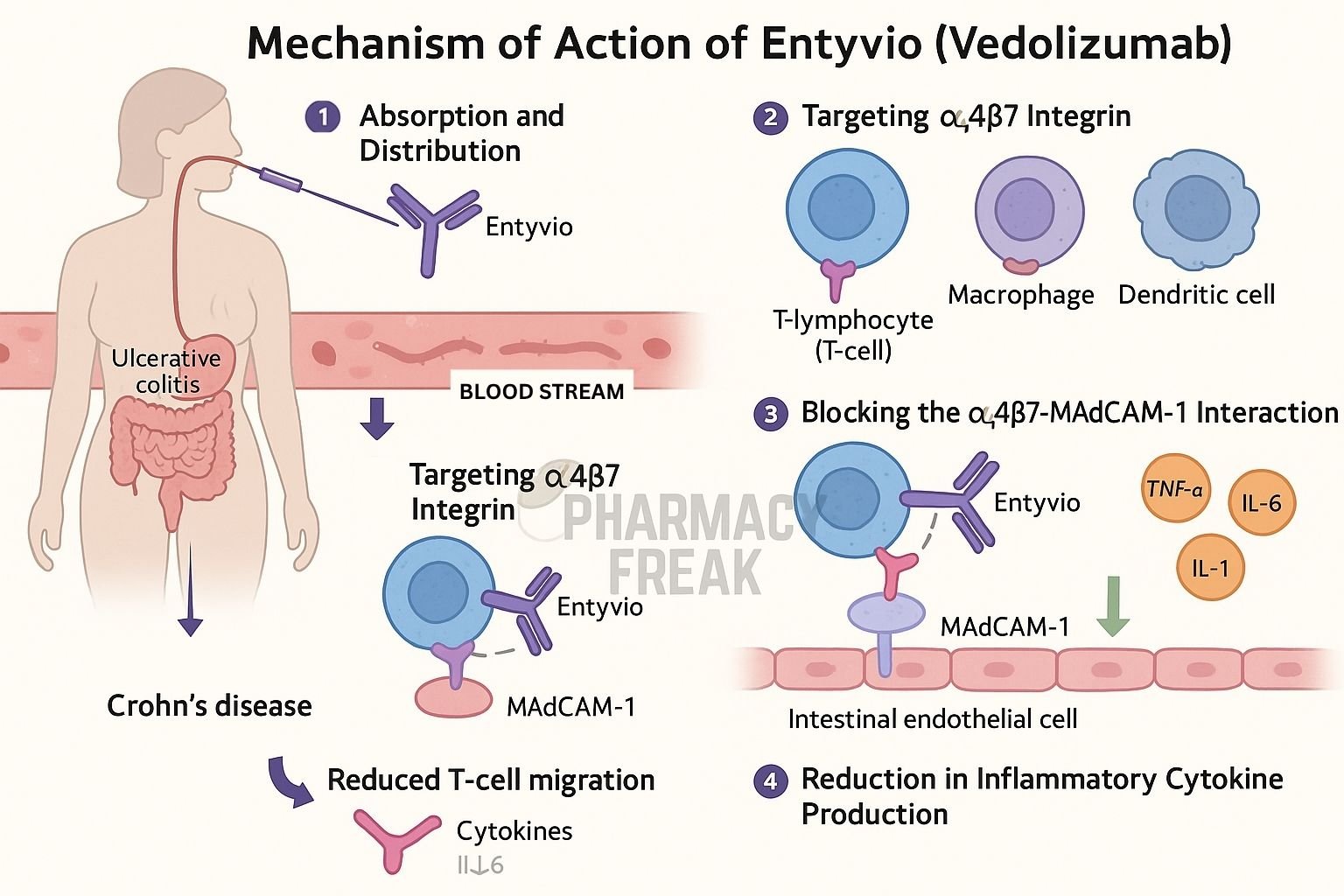
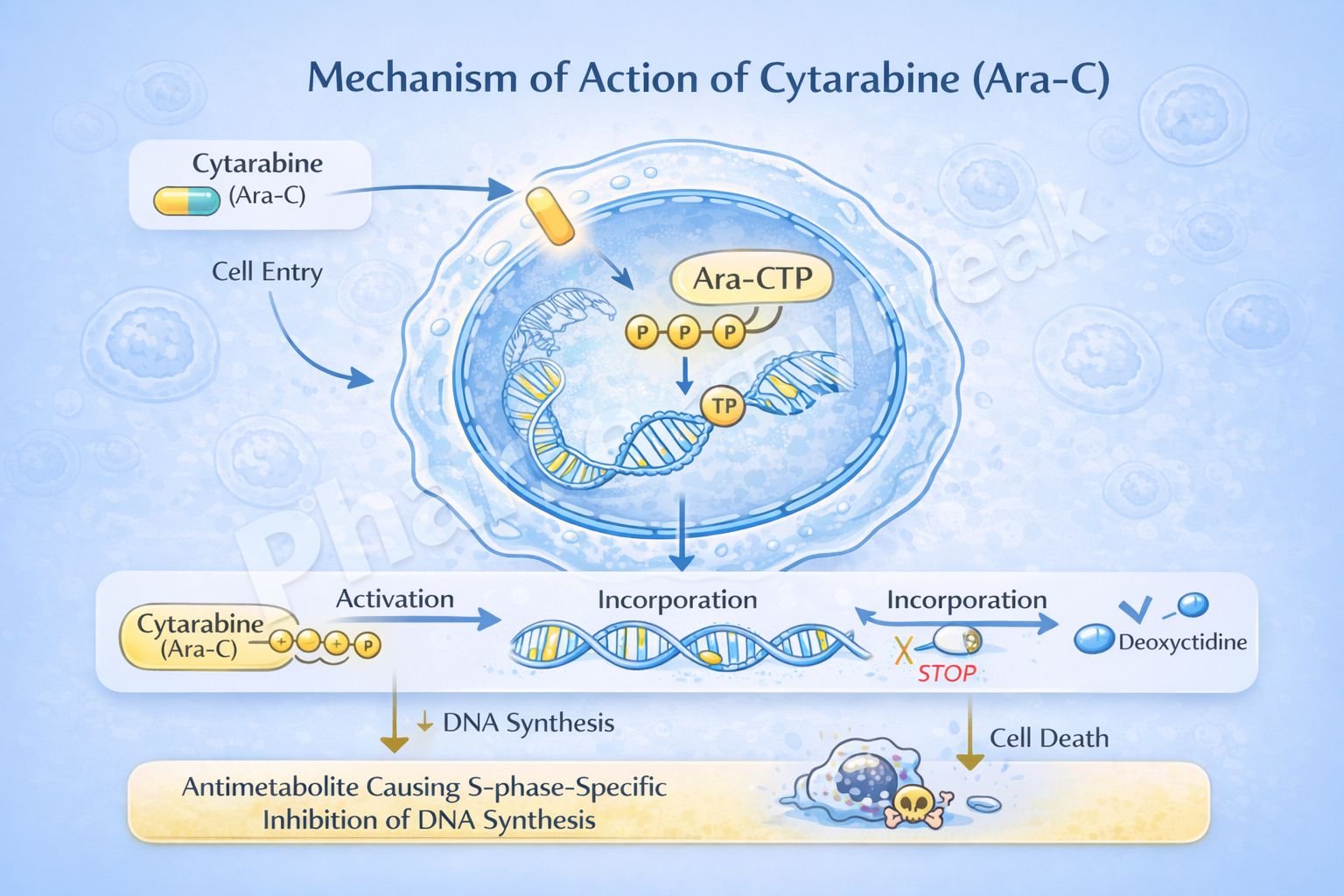
Mechanism-based drug design is used to create more selective drugs with fewer side effects. This has led to the development of monoclonal antibodies and targeted cancer therapies.
Summary Table: Major Drug Targets and Examples
| Drug Target | Example Drugs | Clinical Use | Mechanism |
|---|---|---|---|
| Receptor | Propranolol | Hypertension | Beta-adrenergic receptor blocker |
| Enzyme | Atorvastatin | Hyperlipidemia | HMG-CoA reductase inhibitor |
| Ion Channel | Amlodipine | Hypertension, Angina | Calcium channel blocker |
| Transporter | Fluoxetine | Depression, Anxiety | Serotonin reuptake inhibitor |
| Physical/Chemical | Antacids | Gastric acidity | Neutralizes stomach acid |
Conclusion
The mechanism of action of drugs is a central concept in medicine and pharmacology. It explains not only how drugs treat diseases but also why they can cause side effects or fail to work in some cases. By studying drug mechanisms, medical students build a strong foundation for clinical reasoning, patient care, and lifelong learning.
Remember, every drug you encounter in your medical career will have a specific way it works. Mastering these principles now will help you throughout your studies and into your practice.