Table of Contents
Introduction
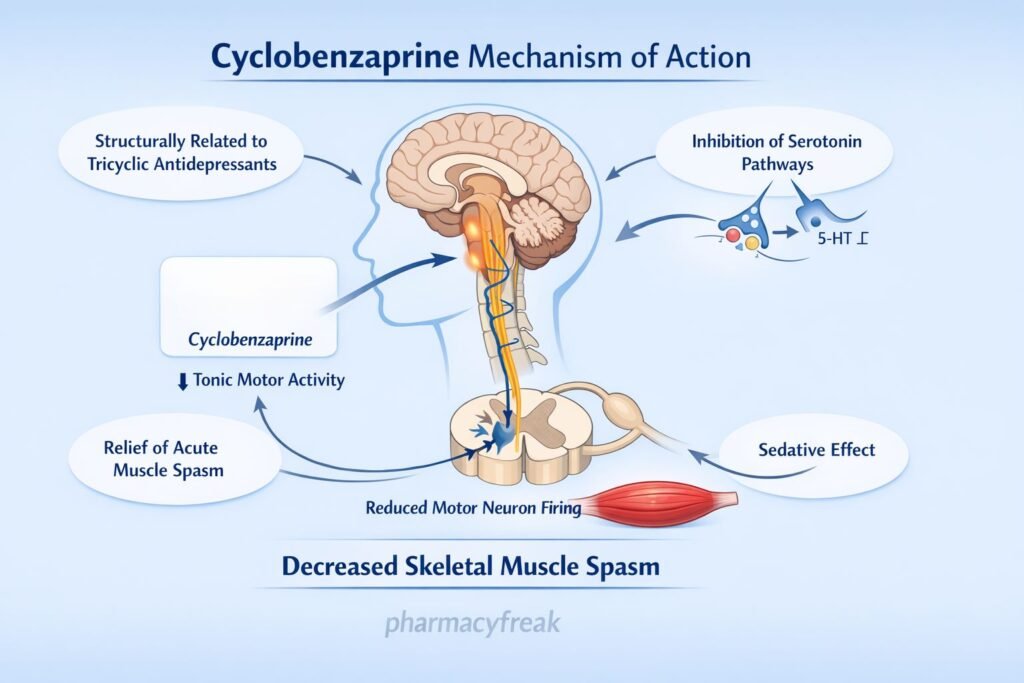
Cyclobenzaprine is a centrally acting skeletal muscle relaxant commonly prescribed for the short-term management of acute musculoskeletal conditions associated with muscle spasm. Structurally and pharmacologically related to tricyclic antidepressants, cyclobenzaprine does not act directly on skeletal muscle or neuromuscular junctions. Instead, it exerts its effects at the central nervous system level. Its distinctive central mechanism and tricyclic-like properties make it a frequently tested drug in pharmacology, orthopedics, anesthesia, and clinical examinations.
Mechanism of Action (Step-wise)
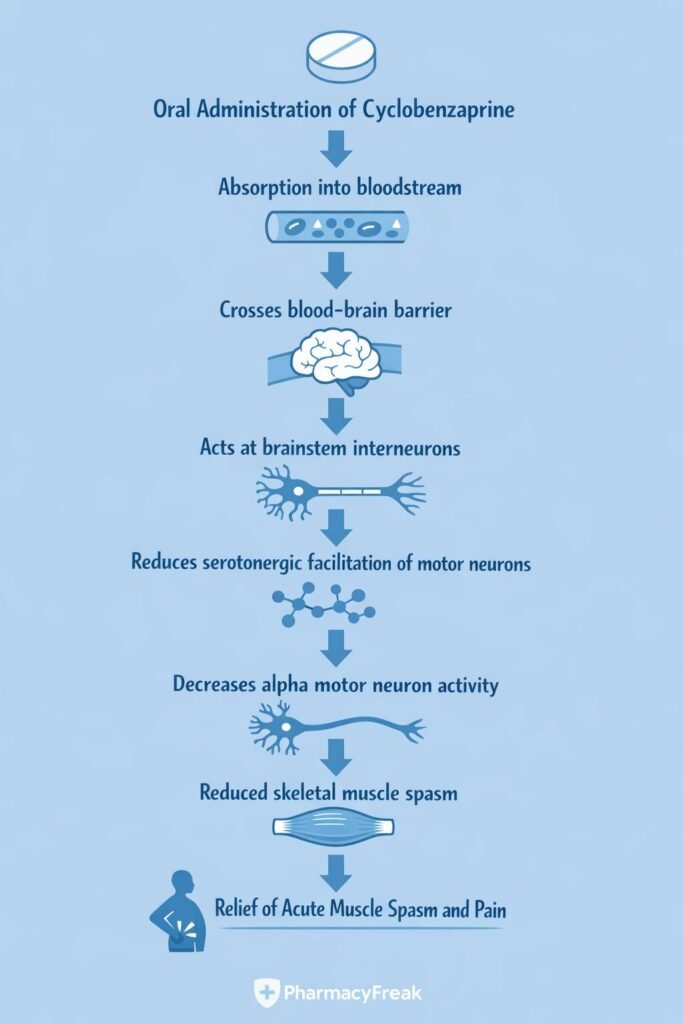
Cyclobenzaprine reduces muscle spasm by modulating central nervous system pathways involved in muscle tone regulation.
Step-wise mechanism:
- Central Site of Action
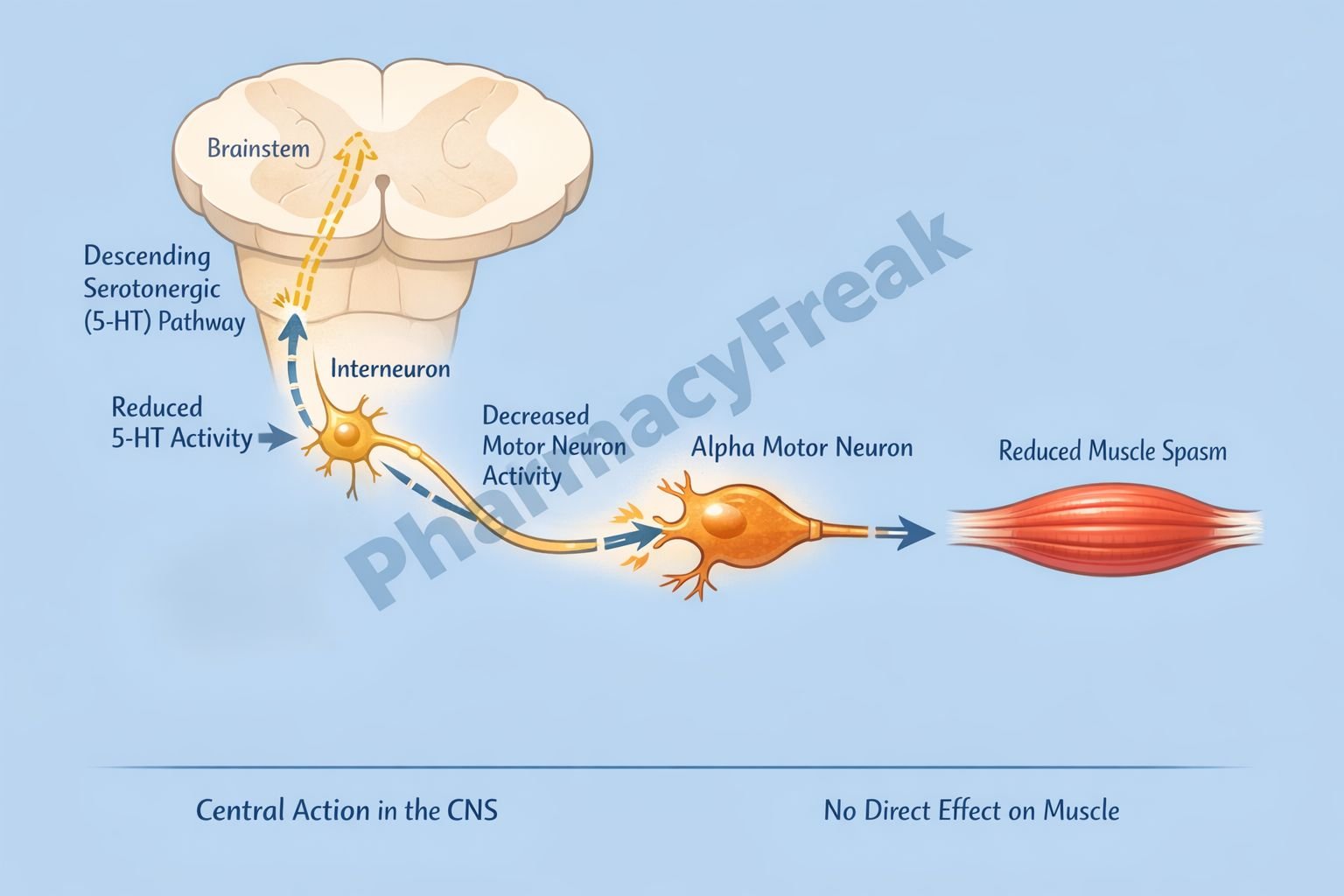
Cyclobenzaprine acts primarily within the brainstem and spinal cord rather than at the neuromuscular junction or muscle fibers. - Reduction of Tonic Somatic Motor Activity
It decreases tonic alpha (α) and gamma (γ) motor neuron activity that maintains muscle tone. - Influence on Descending Pathways
Cyclobenzaprine interferes with descending serotonergic and noradrenergic pathways that facilitate muscle spindle activity. - Brainstem Action
The drug acts at the level of the brainstem, reducing facilitation of spinal motor neurons. - Decreased Muscle Spasm
Reduced motor neuron firing leads to decreased involuntary muscle contractions and relief of muscle spasm. - No Direct Peripheral Effect
Cyclobenzaprine does not act on skeletal muscle fibers, motor end plates, or peripheral nerves.
Pharmacokinetics
- Absorption: Well absorbed orally
- Bioavailability: High, with extensive first-pass metabolism
- Distribution: Widely distributed; highly protein bound
- Metabolism: Hepatic metabolism primarily via CYP1A2, CYP3A4, and CYP2D6
- Elimination: Renal excretion of metabolites
- Half-life: Approximately 18 hours (can be prolonged in elderly)
Dose adjustment is recommended in elderly patients and those with hepatic impairment.
Clinical Uses
Cyclobenzaprine is indicated for short-term relief of muscle spasm associated with acute musculoskeletal conditions:
- Acute low back pain
- Neck and shoulder muscle spasm
- Muscle spasm following injury or strain
- Adjunct to rest and physical therapy
It is not effective for spasticity due to upper motor neuron disorders such as multiple sclerosis or cerebral palsy.
Adverse Effects
Adverse effects are primarily related to its central and anticholinergic actions:
- Central nervous system:
- Drowsiness
- Dizziness
- Fatigue
- Anticholinergic effects:
- Dry mouth
- Blurred vision
- Constipation
- Urinary retention
- Cardiovascular (rare):
- Tachycardia
- Conduction disturbances
Because of its tricyclic-like structure, cyclobenzaprine should be used cautiously in patients with cardiac disease.
Comparative Analysis (must include a table + explanation)
Comparison of Skeletal Muscle Relaxants
| Feature | Cyclobenzaprine | Baclofen | Tizanidine |
|---|---|---|---|
| Primary site of action | Brainstem | Spinal cord | Central (α₂ agonist) |
| Mechanism | Reduces motor neuron activity | GABA-B agonist | α₂-adrenergic agonist |
| Use in acute spasm | Yes | Limited | Yes |
| Sedation | Moderate | Moderate | High |
| Use in spasticity | No | Yes | Yes |
Explanation:
Cyclobenzaprine is best suited for acute musculoskeletal muscle spasm, whereas baclofen and tizanidine are more effective for chronic spasticity associated with neurological disorders. Cyclobenzaprine’s tricyclic-like profile contributes to anticholinergic side effects not seen with other agents.
MCQs (10–15)
- Cyclobenzaprine relieves muscle spasm primarily by acting on the:
a) Neuromuscular junction
b) Skeletal muscle fibers
c) Central nervous system
d) Peripheral nerves
Answer: c) Central nervous system
- Cyclobenzaprine reduces muscle spasm by decreasing activity of:
a) Beta motor neurons
b) Alpha and gamma motor neurons
c) Sensory neurons
d) Autonomic neurons
Answer: b) Alpha and gamma motor neurons
- Cyclobenzaprine is structurally related to:
a) Benzodiazepines
b) Tricyclic antidepressants
c) Opioids
d) Phenothiazines
Answer: b) Tricyclic antidepressants
- Cyclobenzaprine does NOT act at the:
a) Brainstem
b) Spinal cord
c) Neuromuscular junction
d) Central synapses
Answer: c) Neuromuscular junction
- Which adverse effect is most commonly associated with cyclobenzaprine?
a) Diarrhea
b) Sedation
c) Extrapyramidal symptoms
d) Seizures
Answer: b) Sedation
- Cyclobenzaprine is most appropriate for:
a) Multiple sclerosis spasticity
b) Parkinson disease rigidity
c) Acute muscle spasm
d) Epilepsy
Answer: c) Acute muscle spasm
- Cyclobenzaprine should be used cautiously in patients with:
a) Asthma
b) Cardiac conduction disorders
c) Renal stones
d) Hypothyroidism
Answer: b) Cardiac conduction disorders
- Cyclobenzaprine has anticholinergic effects because it is related to:
a) SSRIs
b) MAO inhibitors
c) Tricyclic antidepressants
d) Benzodiazepines
Answer: c) Tricyclic antidepressants
- Cyclobenzaprine is ineffective in spasticity due to:
a) Muscle injury
b) Low back strain
c) Upper motor neuron lesions
d) Acute trauma
Answer: c) Upper motor neuron lesions
- The primary therapeutic effect of cyclobenzaprine is:
a) Muscle paralysis
b) Muscle relaxation
c) Pain relief via opioid action
d) Sedation only
Answer: b) Muscle relaxation
FAQs (minimum 5)
- What is the primary mechanism of cyclobenzaprine?
It reduces muscle spasm by decreasing central motor neuron activity in the brainstem. - Does cyclobenzaprine act on skeletal muscle directly?
No, it has no direct peripheral muscle action. - Why does cyclobenzaprine cause dry mouth?
Due to its anticholinergic properties. - Is cyclobenzaprine useful for chronic spasticity?
No, it is mainly for acute musculoskeletal conditions. - Why is cyclobenzaprine sedating?
Because of central nervous system depression and antihistaminic effects. - Can cyclobenzaprine affect the heart?
Yes, due to its tricyclic-like structure, it may affect cardiac conduction.
References
- Goodman & Gilman’s The Pharmacological Basis of Therapeutics
https://accessmedicine.mhmedical.com - Katzung BG. Basic and Clinical Pharmacology
https://accessmedicine.mhmedical.com - Tripathi KD. Essentials of Medical Pharmacology
https://www.jaypeebrothers.com - Harrison’s Principles of Internal Medicine
https://accessmedicine.mhmedical.com

I am pursuing MBA in pharmaceutical management from NIPER Hyderabad with a strong academic record and proven success in national-level pharmacy entrance exams. I secured AIR 61 in NIPER 2024 (MS/M.Pharm) and AIR 27 in NIPER MBA, along with AIR 147 in GPAT 2024 and AIR 907 in GPAT 2023. I also achieved AIR 6 in AIIMS CRE-2025 for Drug Store Keeper and was selected as a Pharmacist (AIR 61) for ESIC. Additionally, I was the Runner-Up in Round 2 of the EY Case Study Competition.
At PharmacyFreak.com, I aim to guide future pharmacists through expert content, exam strategies, and insightful resources based on real experience and academic excellence.
Mail- harsh@pharmacyfreak.com