Table of Contents
Introduction
Corticosteroids are a class of steroid hormones that exert potent anti-inflammatory, immunosuppressive, anti-allergic, and metabolic effects. They are synthetic analogs of endogenous glucocorticoids produced by the adrenal cortex, primarily cortisol. Corticosteroids are extensively used across multiple medical specialties, including internal medicine, pulmonology, dermatology, rheumatology, neurology, and critical care. Their broad mechanism of action at the genomic and cellular level makes them a high-yield topic in pharmacology and clinical entrance examinations.


Mechanism of Action (Step-wise)
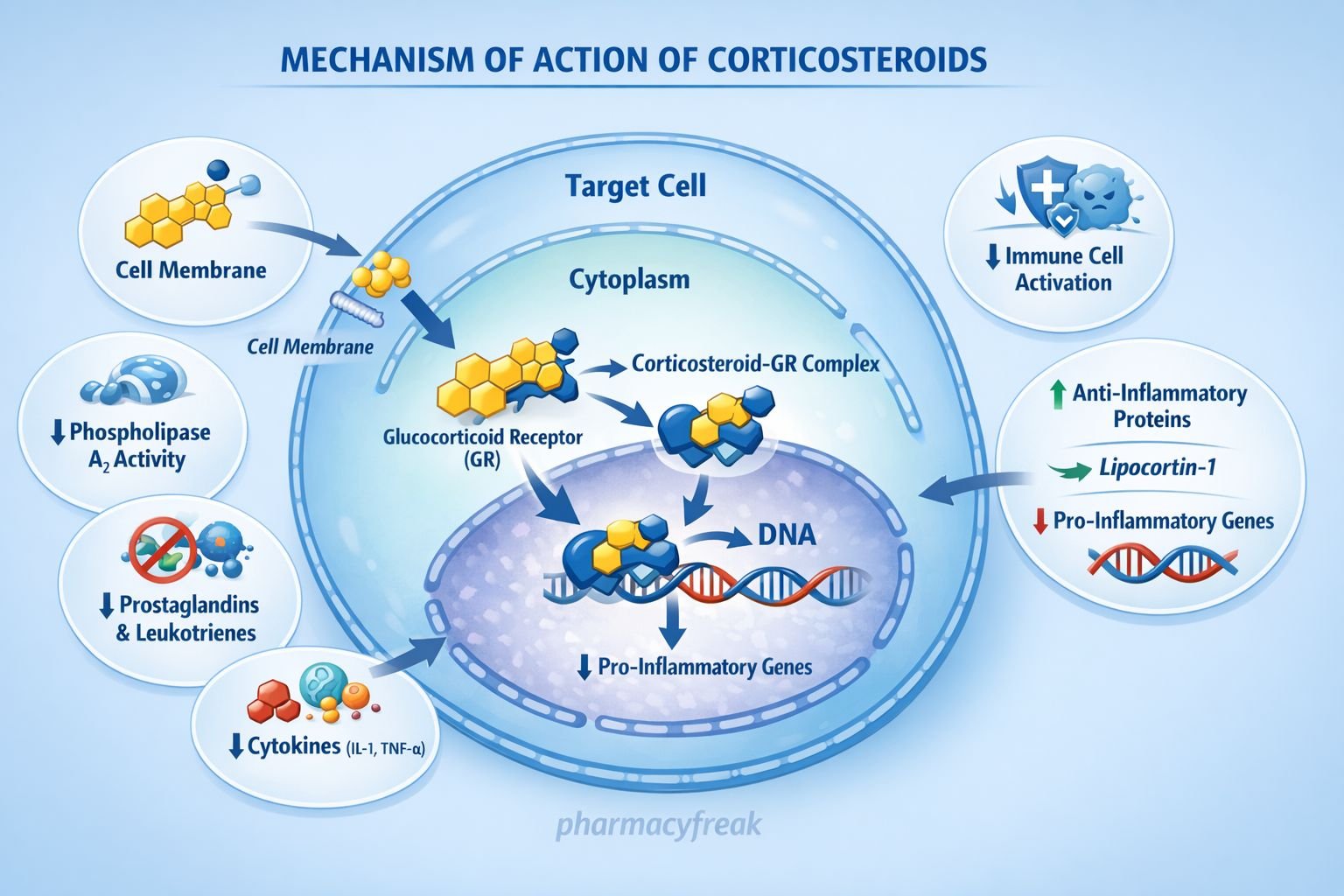
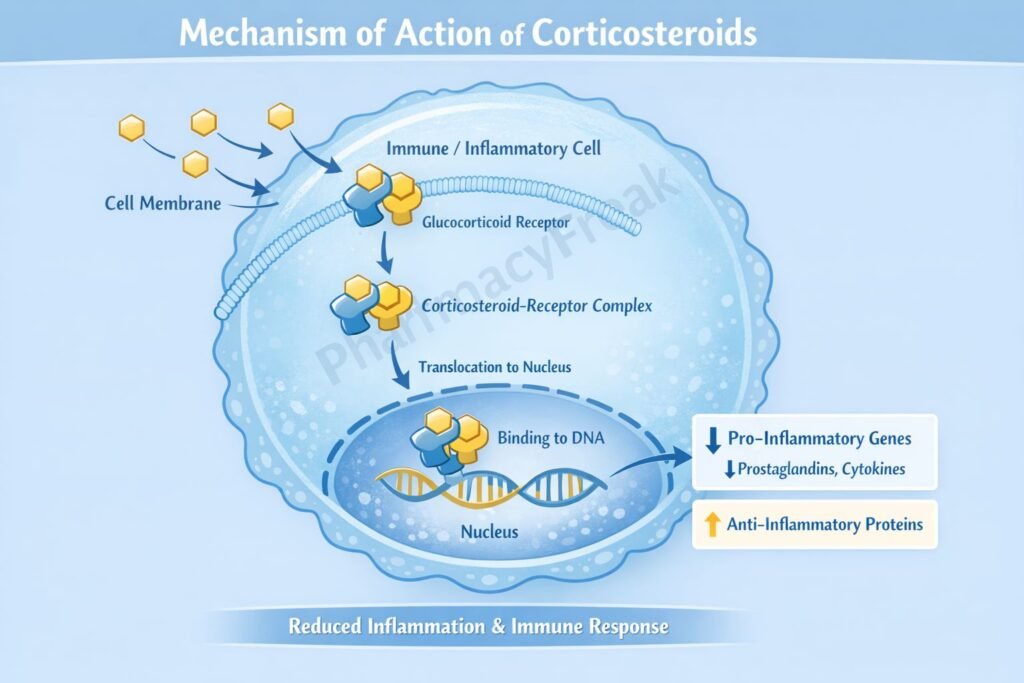
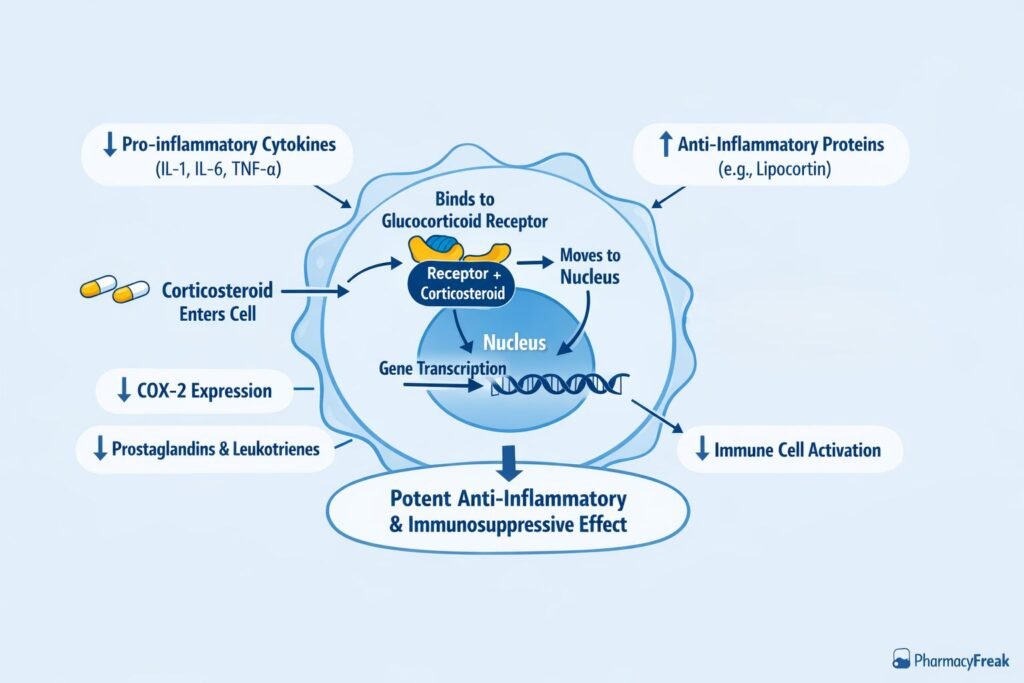
Corticosteroids exert their effects primarily through intracellular glucocorticoid receptor–mediated gene regulation.
Step-wise mechanism:
- Cell Membrane Diffusion
Corticosteroids are lipophilic and freely diffuse across the cell membrane into the cytoplasm. - Binding to Glucocorticoid Receptor (GR)
In the cytoplasm, corticosteroids bind to inactive glucocorticoid receptors complexed with heat shock proteins (HSPs). - Receptor Activation and Translocation
Binding causes dissociation of HSPs, activating the steroid–receptor complex, which then translocates into the nucleus. - Gene Transcription Modulation
The activated complex binds to glucocorticoid response elements (GREs) on DNA. - Upregulation of Anti-inflammatory Proteins
Increased transcription of anti-inflammatory proteins such as:- Lipocortin-1 (annexin A1), which inhibits phospholipase A₂
- IL-10 and other anti-inflammatory mediators
- Downregulation of Pro-inflammatory Genes
Suppression of transcription of:- Cytokines (IL-1, IL-2, IL-6, TNF-α)
- COX-2
- Inducible nitric oxide synthase (iNOS)
- Inhibition of Arachidonic Acid Pathway
Reduced prostaglandin and leukotriene synthesis results in decreased inflammation. - Immunosuppressive and Anti-inflammatory Effects
Net result includes reduced capillary permeability, decreased leukocyte migration, and suppression of immune responses.
Pharmacokinetics
- Absorption: Well absorbed orally; also effective via IV, IM, inhaled, topical routes
- Distribution: Widely distributed; high protein binding (albumin, transcortin)
- Metabolism: Hepatic metabolism
- Elimination: Renal excretion of metabolites
- Half-life: Varies by agent (e.g., hydrocortisone short, dexamethasone long)
- Biological effect duration: Longer than plasma half-life due to genomic action
Clinical Uses
Corticosteroids are used in a wide range of inflammatory, autoimmune, allergic, and neoplastic conditions:
- Bronchial asthma and COPD
- Autoimmune diseases (RA, SLE, vasculitis)
- Allergic reactions and anaphylaxis (adjunct)
- Inflammatory bowel disease
- Cerebral edema
- Organ transplantation (immunosuppression)
- Adrenal insufficiency (replacement therapy)
- Certain malignancies (lymphomas, leukemias)
Adverse Effects
Adverse effects are dose- and duration-dependent:
- Metabolic:
- Hyperglycemia
- Weight gain
- Dyslipidemia
- Endocrine:
- Adrenal suppression
- Cushingoid features
- Musculoskeletal:
- Osteoporosis
- Myopathy
- Immune:
- Increased infection risk
- Delayed wound healing
- Gastrointestinal:
- Peptic ulcer disease
- Neuropsychiatric:
- Mood changes
- Psychosis
Abrupt withdrawal after long-term use can cause acute adrenal insufficiency.
Comparative Analysis (must include a table + explanation)
Comparison of Anti-inflammatory Drug Classes
| Feature | Corticosteroids | NSAIDs | Biologic Agents |
|---|---|---|---|
| Site of action | Gene transcription | COX inhibition | Cytokine blockade |
| Potency | Very high | Moderate | High |
| Onset | Slow (hours–days) | Fast | Variable |
| Immunosuppression | Strong | Minimal | Targeted |
| Adverse effects | Systemic | GI, renal | Infection risk |
Explanation:
Corticosteroids act upstream at the genomic level, making them more potent than NSAIDs. Unlike biologics, they are non-selective and suppress multiple inflammatory pathways, accounting for both their efficacy and wide adverse-effect profile.
MCQs (10–15)
- Corticosteroids exert anti-inflammatory effects primarily by:
a) Blocking COX enzymes
b) Inhibiting phospholipase A₂
c) Blocking histamine receptors
d) Neutralizing cytokines
Answer: b) Inhibiting phospholipase A₂
- Corticosteroids act via which receptor type?
a) Membrane ion channel
b) Tyrosine kinase receptor
c) Nuclear intracellular receptor
d) G-protein–coupled receptor
Answer: c) Nuclear intracellular receptor
- Which protein induced by corticosteroids inhibits arachidonic acid release?
a) COX-2
b) Lipocortin-1
c) NF-κB
d) TNF-α
Answer: b) Lipocortin-1
- Corticosteroids reduce inflammation by decreasing:
a) Histamine synthesis
b) Cytokine gene transcription
c) Antibody production only
d) Platelet aggregation
Answer: b) Cytokine gene transcription
- Which pathway is inhibited by corticosteroids?
a) Renin–angiotensin
b) Arachidonic acid
c) Glycolysis
d) Oxidative phosphorylation
Answer: b) Arachidonic acid
- Corticosteroids suppress immunity mainly by:
a) Neutrophil activation
b) T-cell suppression
c) Complement activation
d) Mast cell degranulation
Answer: b) T-cell suppression
- Long-term corticosteroid therapy causes:
a) Hyperkalemia
b) Osteoporosis
c) Hypoglycemia
d) Bradycardia
Answer: b) Osteoporosis
- Abrupt withdrawal of corticosteroids may cause:
a) Hypertension
b) Cushing syndrome
c) Adrenal insufficiency
d) Thyroid storm
Answer: c) Adrenal insufficiency
- Which corticosteroid has the longest duration of action?
a) Hydrocortisone
b) Prednisolone
c) Dexamethasone
d) Cortisone
Answer: c) Dexamethasone
- Corticosteroids reduce prostaglandin synthesis by:
a) COX inhibition only
b) Blocking prostaglandin receptors
c) Reducing arachidonic acid availability
d) Increasing leukotriene synthesis
Answer: c) Reducing arachidonic acid availability
FAQs (minimum 5)
- Do corticosteroids act genomically or non-genomically?
Primarily genomically via nuclear receptor–mediated gene transcription. - Why do corticosteroids take time to act?
Because their effects depend on altered protein synthesis. - Do corticosteroids suppress prostaglandins and leukotrienes?
Yes, by inhibiting phospholipase A₂. - Why must corticosteroids be tapered?
To prevent adrenal insufficiency due to HPA axis suppression. - Are corticosteroids immunosuppressive?
Yes, they suppress both innate and adaptive immune responses. - Do corticosteroids increase infection risk?
Yes, especially with long-term or high-dose therapy.
References
- Goodman & Gilman’s The Pharmacological Basis of Therapeutics
https://accessmedicine.mhmedical.com - Katzung BG. Basic and Clinical Pharmacology
https://accessmedicine.mhmedical.com - Tripathi KD. Essentials of Medical Pharmacology
https://www.jaypeebrothers.com - Harrison’s Principles of Internal Medicine
https://accessmedicine.mhmedical.com

I am pursuing MBA in pharmaceutical management from NIPER Hyderabad with a strong academic record and proven success in national-level pharmacy entrance exams. I secured AIR 61 in NIPER 2024 (MS/M.Pharm) and AIR 27 in NIPER MBA, along with AIR 147 in GPAT 2024 and AIR 907 in GPAT 2023. I also achieved AIR 6 in AIIMS CRE-2025 for Drug Store Keeper and was selected as a Pharmacist (AIR 61) for ESIC. Additionally, I was the Runner-Up in Round 2 of the EY Case Study Competition.
At PharmacyFreak.com, I aim to guide future pharmacists through expert content, exam strategies, and insightful resources based on real experience and academic excellence.
Mail- harsh@pharmacyfreak.com