Table of Contents
Introduction
Chloroquine is a 4-aminoquinoline antimalarial drug historically used for the treatment and prophylaxis of Plasmodium falciparum, P. vivax, P. malariae, and P. ovale infections. Although resistance limits its use in many regions, chloroquine remains essential for sensitive strains and for autoimmune diseases such as rheumatoid arthritis and lupus.
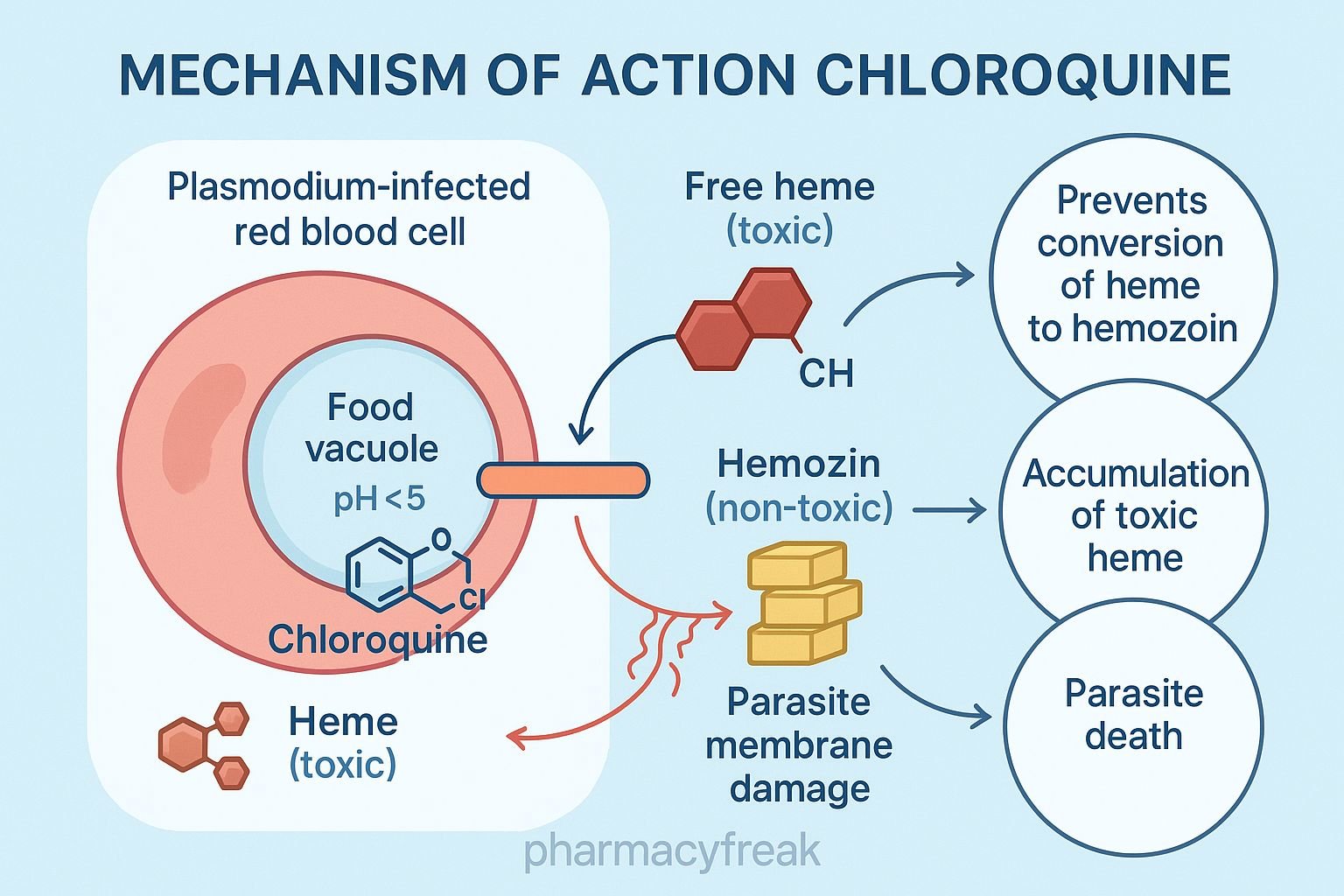
The Mechanism of Action of Chloroquine is primarily based on inhibition of heme detoxification in Plasmodium, leading to parasite death within red blood cells. It also has immunomodulatory effects, explaining its role in autoimmune disorders.



Mechanism of Action (Step-wise)
1. Accumulation in Parasite Food Vacuole – Primary Mechanism
Chloroquine is a weak base that diffuses into the acidic food vacuole of Plasmodium-infected erythrocytes.
Inside the vacuole:
- It becomes protonated and trapped (ion trapping).
- Concentration increases more than 1000-fold.
2. Inhibition of Heme Polymerase
During hemoglobin digestion, Plasmodium releases toxic free heme (ferriprotoporphyrin IX).
Normally:
Heme → polymerized into hemozoin (non-toxic)
Chloroquine blocks heme polymerase, leading to:
- Accumulation of toxic heme
- Membrane damage
- Parasite death
This is the central antimalarial mechanism.
3. Increased Lysosomal pH
By raising pH inside the parasite vacuole, chloroquine disrupts:
- Proteolytic enzymes
- Hemoglobin degradation
- Parasite metabolism
4. Oxidative Stress
Accumulated heme generates:
- Reactive oxygen species
- Lipid peroxidation
- Oxidative damage
This enhances parasite killing.
5. Immunomodulatory Effects (Non-antimalarial)
Chloroquine inhibits:
- Toll-like receptor (TLR) signaling
- Antigen presentation
- Cytokine production (IL-1, TNF-α)
These actions explain its use in SLE and rheumatoid arthritis.
6. Summary of Mechanism
| Mechanism | Effect |
|---|---|
| Accumulates in food vacuole | Ion trapping |
| Inhibits heme polymerase | Toxic heme buildup |
| Raises vacuolar pH | Disrupts parasite digestion |
| Oxidative stress | Parasite death |
| Immunomodulation | Useful in SLE/RA |
Pharmacokinetics
- Absorption: Excellent oral absorption
- Distribution: Very large volume; accumulates in tissues (eye, liver)
- Half-life: 1–2 months (extremely long)
- Metabolism: Hepatic
- Excretion: Renal
Clinical Uses
- Treatment of chloroquine-sensitive malaria
- Prophylaxis in chloroquine-sensitive regions
- Rheumatoid arthritis
- Systemic lupus erythematosus
- Amebic liver abscess (adjunct)
- Porphyria cutanea tarda
Adverse Effects
Common
- Nausea
- Headache
- Pruritus
Serious
- Retinopathy (dose-dependent, irreversible)
- QT prolongation
- Hemolysis in G6PD deficiency
- Hypotension (IV form)
- Neuropsychiatric effects (rare)
Chronic toxicity
- Bull’s-eye maculopathy
- Hearing loss
- Cardiomyopathy
Contraindications
- Pre-existing retinal disease
- Severe hepatic impairment
- G6PD deficiency (relative)
- Concomitant QT-prolonging drugs
Comparative Analysis
| Feature | Chloroquine | Hydroxychloroquine | Quinine |
|---|---|---|---|
| Toxicity | Higher | Lower | High |
| Retinopathy risk | High | Lower | Low |
| Autoimmune role | Limited | Strong | None |
| Resistance | Widespread | Widespread | Minimal |
MCQs
1. Chloroquine kills Plasmodium by inhibiting:
a) Folic acid synthesis
b) DNA polymerase
c) Heme polymerase
d) Mitochondrial respiration
Answer: c) Heme polymerase
2. Accumulation of free heme in malaria causes:
a) Parasite growth
b) Oxidative damage and death
c) Increased hemoglobin digestion
d) Resistance to chloroquine
Answer: b) Oxidative damage and death
3. Chloroquine is concentrated in the parasite because:
a) It binds ribosomes
b) It undergoes ion trapping in acidic vacuoles
c) It inhibits ATPases
d) It binds to DNA
Answer: b) It undergoes ion trapping in acidic vacuoles
4. Long-term chloroquine therapy may cause:
a) Retinopathy
b) Hepatic necrosis
c) Alopecia
d) Nephritis
Answer: a) Retinopathy
5. Chloroquine resistance occurs mainly due to:
a) Enhanced drug metabolism
b) Efflux pumps in Plasmodium
c) Heme polymerase mutation
d) Failure of absorption
Answer: b) Efflux pumps in Plasmodium
FAQs
Q1. Why does chloroquine cause retinopathy?
It accumulates in retinal pigmented epithelium and damages photoreceptors.
Q2. Is chloroquine still used for malaria?
Only in regions where P. falciparum remains chloroquine-sensitive.
Q3. How fast does chloroquine act?
Rapid action—parasitemia decreases within 24–48 hours.
Q4. Why is it effective in autoimmune diseases?
Due to TLR inhibition and suppression of inflammatory cytokines.
Q5. Is chloroquine safe in pregnancy?
Yes—considered safe at therapeutic doses.
References
Goodman & Gilman’s Pharmacological Basis of Therapeutics
https://accesspharmacy.mhmedical.com/book.aspx?bookid=2189
Katzung: Basic and Clinical Pharmacology
https://accessmedicine.mhmedical.com/book.aspx?bookid=2464
Tripathi: Essentials of Medical Pharmacology
https://jaypeebrothers.com/
Harrison’s Principles of Internal Medicine
https://accessmedicine.mhmedical.com/book.aspx?bookid=2129

I am pursuing MBA in pharmaceutical management from NIPER Hyderabad with a strong academic record and proven success in national-level pharmacy entrance exams. I secured AIR 61 in NIPER 2024 (MS/M.Pharm) and AIR 27 in NIPER MBA, along with AIR 147 in GPAT 2024 and AIR 907 in GPAT 2023. I also achieved AIR 6 in AIIMS CRE-2025 for Drug Store Keeper and was selected as a Pharmacist (AIR 61) for ESIC. Additionally, I was the Runner-Up in Round 2 of the EY Case Study Competition.
At PharmacyFreak.com, I aim to guide future pharmacists through expert content, exam strategies, and insightful resources based on real experience and academic excellence.
Mail- harsh@pharmacyfreak.com