Table of Contents
Introduction
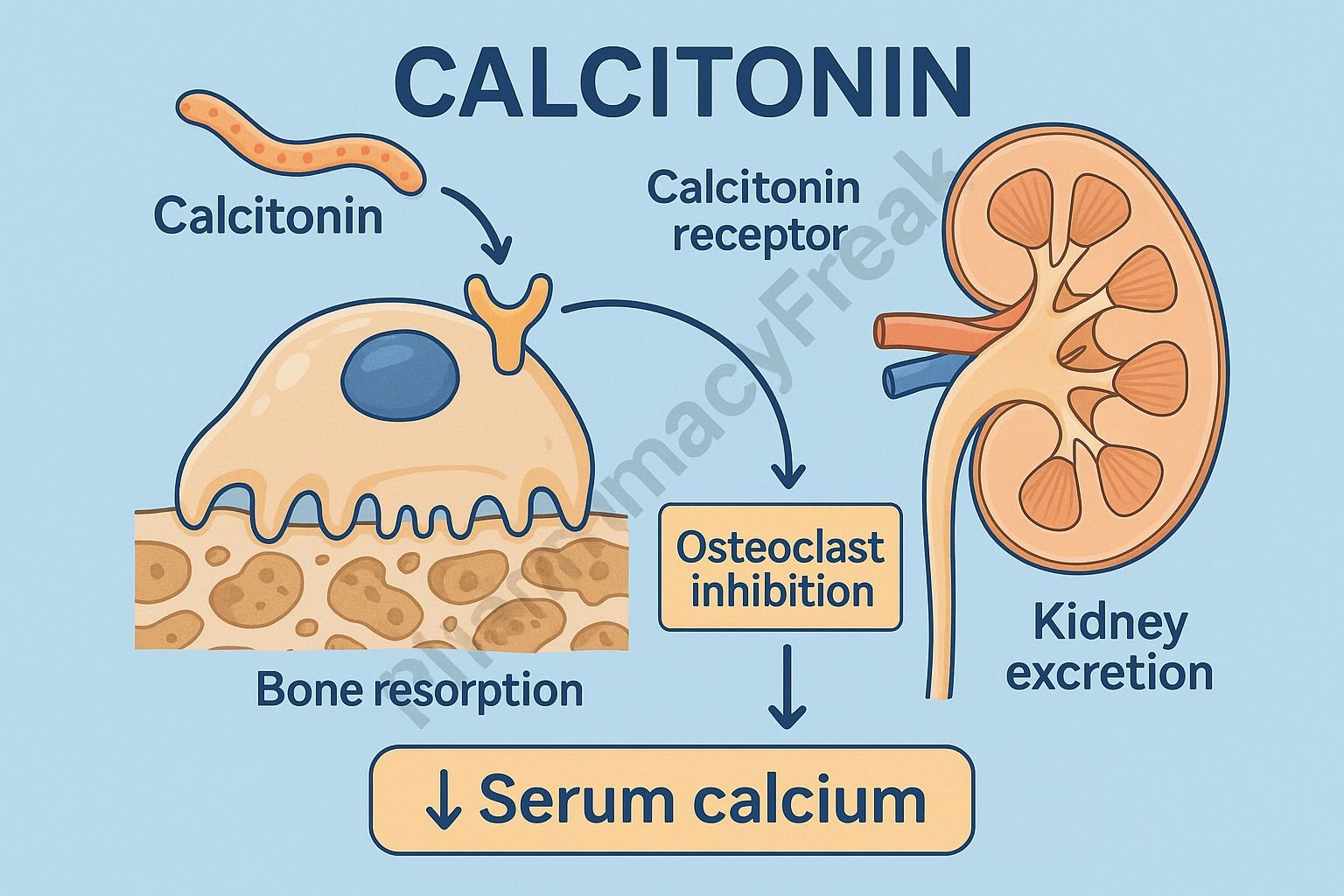
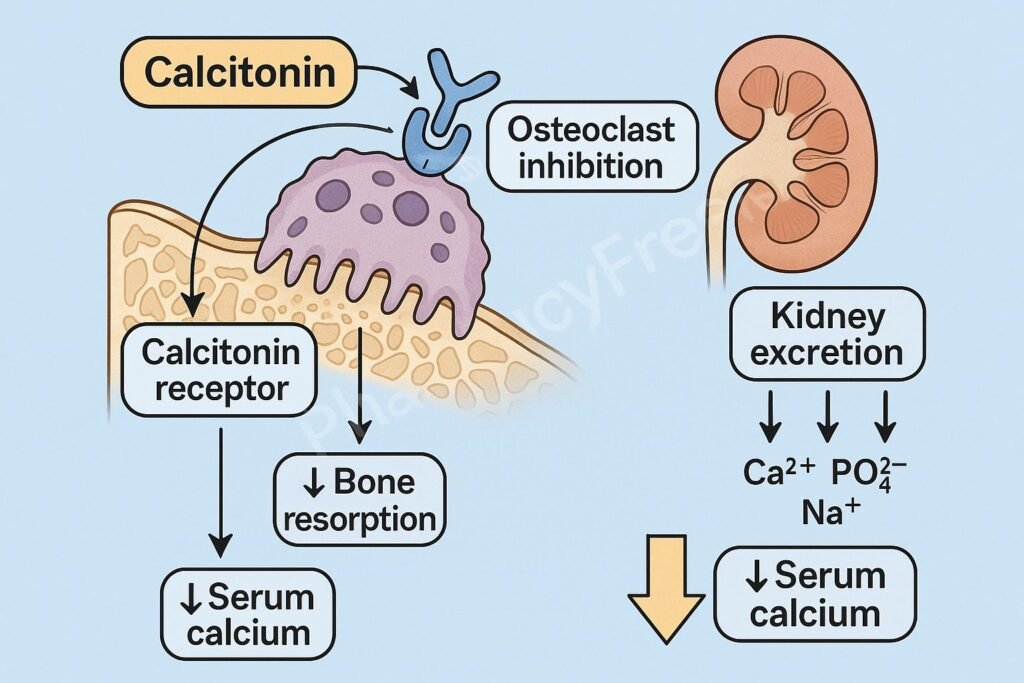
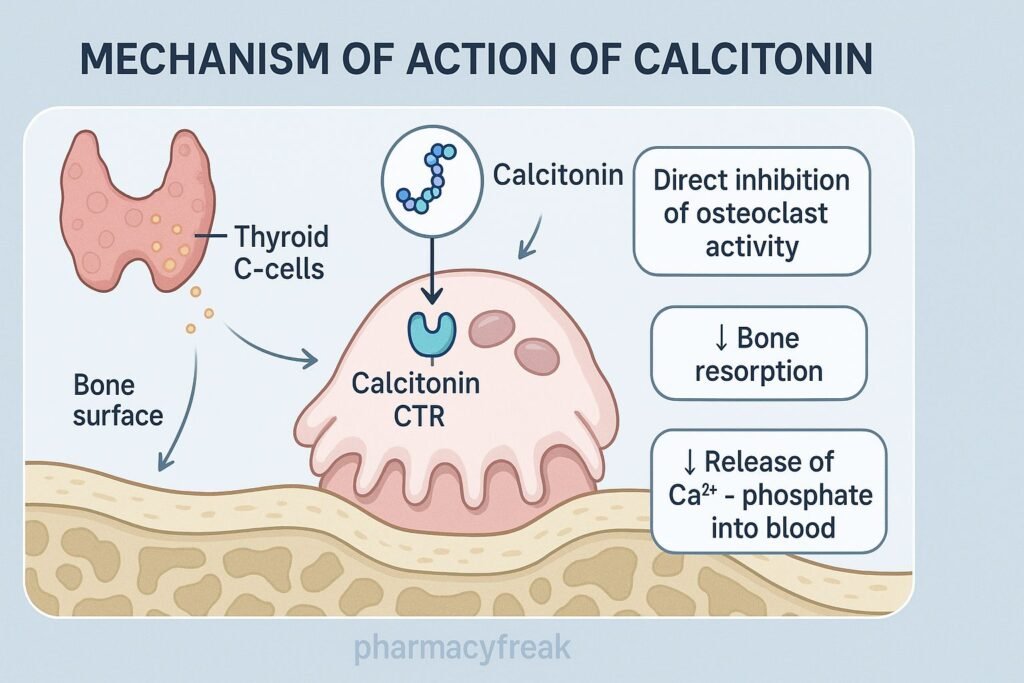
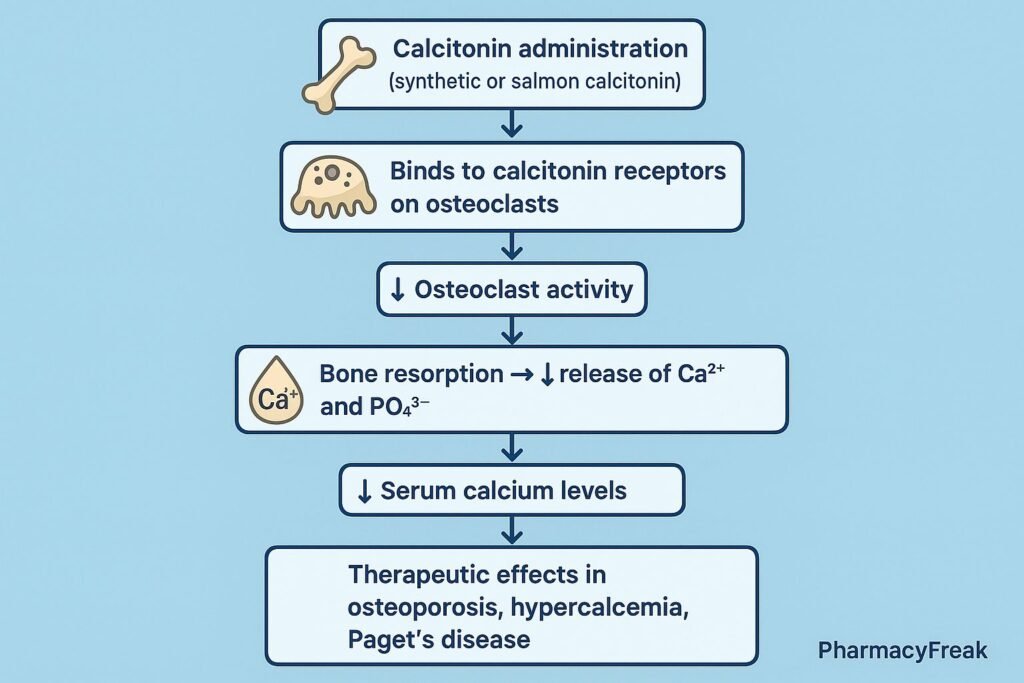
Calcitonin is a peptide hormone produced by the parafollicular (C cells) of the thyroid gland and is also available as a therapeutic agent (salmon calcitonin). It plays an essential role in calcium and bone metabolism, acting as a physiological antagonist to parathyroid hormone (PTH).
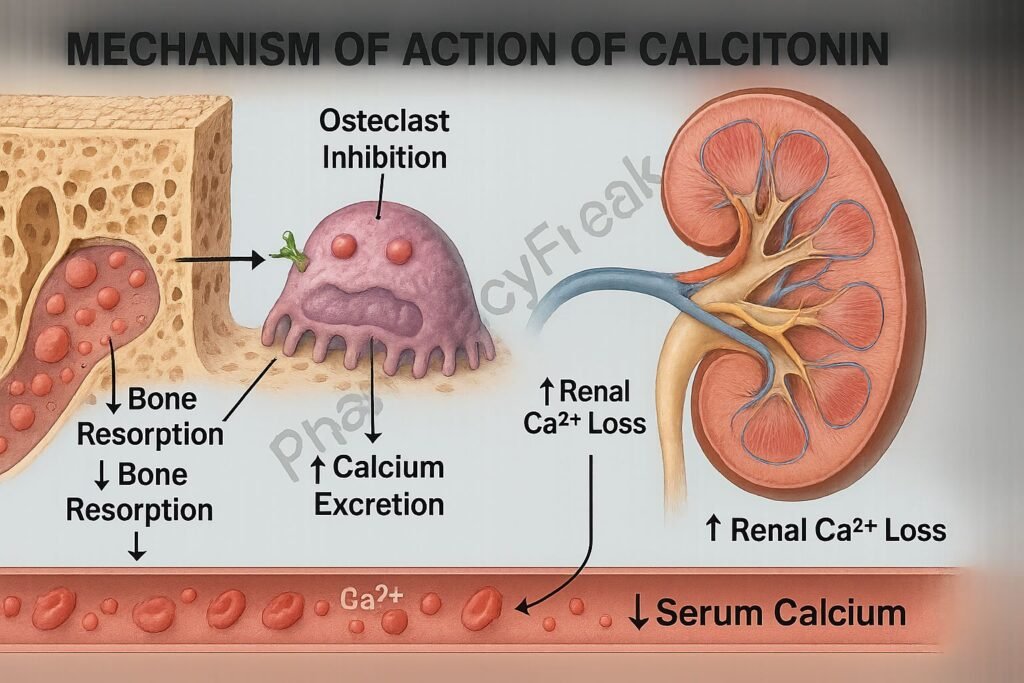
The Mechanism of Action of Calcitonin centers on inhibition of osteoclastic bone resorption and enhanced renal excretion of calcium and phosphate, making it useful in osteoporosis, hypercalcemia, Paget’s disease, and bone pain disorders.
Mechanism of Action (Step-wise)
1. Inhibition of Osteoclast Activity – Primary Mechanism
Calcitonin binds to specific calcitonin receptors on osteoclasts.
Effects:
- ↓ Osteoclast mobility
- ↓ Osteoclast ruffled border formation
- ↓ Bone resorption
- ↓ Calcium release from bone
Result: Reduced serum calcium and slowed bone turnover.
2. Decreased Bone Resorption
By suppressing osteoclasts:
- Bone mineral density is preserved
- Bone turnover rate decreases
- Acute bone pain is relieved (useful in Paget’s disease and vertebral fractures)
3. Increased Renal Excretion of Calcium
Calcitonin acts on the renal tubules to increase calcium excretion.
Mechanisms:
- ↓ Renal tubular reabsorption of Ca²⁺
- ↓ Reabsorption of phosphate (PO₄³⁻)
- ↓ Reabsorption of sodium (Na⁺)
Effect: Reduction in serum calcium levels.
4. Inhibition of Osteoclast-Mediated Proton Pumping
Osteoclasts normally acidify the bone surface to dissolve hydroxyapatite.
Calcitonin blocks:
- Proton pump activation
- Acid secretion into the resorption lacuna
Effect: Inhibition of bone matrix dissolution.
5. Modulation of Gastrointestinal Calcium Handling
Calcitonin mildly reduces:
- Intestinal calcium absorption
This contributes modestly to lowering serum calcium.
6. Summary of Mechanism
| Mechanism | Effect |
|---|---|
| Binds osteoclast receptors | ↓ Bone resorption |
| Inhibits proton pumps | ↓ Hydroxyapatite dissolution |
| ↑ Renal calcium excretion | ↓ Serum calcium |
| ↑ Phosphate excretion | ↓ Serum phosphate |
| Mild ↓ GI absorption | Additional Ca²⁺ lowering |
Pharmacokinetics
- Source: Salmon calcitonin (more potent and longer acting than human)
- Administration: Intranasal, subcutaneous, IM
- Onset: Rapid (within hours)
- Half-life: 1–2 hours (biological effect longer)
- Metabolism: Kidney and peripheral tissues
Clinical Uses
- Hypercalcemia of malignancy
- Paget’s disease of bone
- Postmenopausal osteoporosis
- Bone pain due to fractures or metastases
- Acute vertebral fracture pain relief
Adverse Effects
- Nausea and vomiting
- Flushing
- Hypocalcemia
- Allergic reactions (greater with salmon calcitonin)
- Nasal irritation (intranasal form)
- Tachyphylaxis with long-term use (months)
Contraindications
- Hypocalcemia
- Hypersensitivity to salmon calcitonin
- Pregnancy and breastfeeding (caution)
Comparative Analysis
| Feature | Calcitonin | Bisphosphonates | PTH Analogues |
|---|---|---|---|
| Mechanism | ↓ Osteoclast activity | ↓ Bone resorption (potent) | ↑ Bone formation |
| Hypercalcemia relief | Rapid | Slow | Not useful |
| Osteoporosis benefit | Weak | Strong | Strong |
| Site of action | Osteoclasts | Bone matrix & osteoclasts | Osteoblasts |
MCQs
1. Calcitonin reduces serum calcium primarily by:
a) Increasing PTH secretion
b) Increasing osteoclast activity
c) Inhibiting osteoclasts
d) Increasing intestinal absorption
Answer: c) Inhibiting osteoclasts
2. Calcitonin increases renal excretion of:
a) Calcium and phosphate
b) Glucose
c) Potassium
d) Urea
Answer: a) Calcium and phosphate
3. Calcitonin is most useful for rapid correction of:
a) Hypocalcemia
b) Hypercalcemia
c) Hyperkalemia
d) Hyponatremia
Answer: b) Hypercalcemia
4. Long-term use of calcitonin is limited by:
a) Hepatotoxicity
b) Tachyphylaxis
c) Renal failure
d) Thyroid suppression
Answer: b) Tachyphylaxis
5. Calcitonin has strong analgesic effects in:
a) Migraine
b) Vertebral fractures
c) Osteoarthritis
d) Rheumatoid arthritis
Answer: b) Vertebral fractures
FAQs
Q1. How quickly does calcitonin lower calcium levels?
Within 4–6 hours, making it useful for acute hypercalcemia.
Q2. Is salmon calcitonin stronger than human calcitonin?
Yes—more potent and longer acting.
Q3. Can calcitonin be used long-term for osteoporosis?
Less preferred due to tachyphylaxis and weaker effect compared to bisphosphonates.
Q4. Does calcitonin relieve bone pain?
Yes—especially in vertebral fractures and Paget’s disease.
Q5. Is intranasal calcitonin effective?
Yes, but nasal irritation is common.
References
Goodman & Gilman’s Pharmacological Basis of Therapeutics
https://accesspharmacy.mhmedical.com/book.aspx?bookid=2189
Katzung: Basic and Clinical Pharmacology
https://accessmedicine.mhmedical.com/book.aspx?bookid=2464
Tripathi: Essentials of Medical Pharmacology
https://jaypeebrothers.com/
Harrison’s Principles of Internal Medicine
https://accessmedicine.mhmedical.com/book.aspx?bookid=2129

I am pursuing MBA in pharmaceutical management from NIPER Hyderabad with a strong academic record and proven success in national-level pharmacy entrance exams. I secured AIR 61 in NIPER 2024 (MS/M.Pharm) and AIR 27 in NIPER MBA, along with AIR 147 in GPAT 2024 and AIR 907 in GPAT 2023. I also achieved AIR 6 in AIIMS CRE-2025 for Drug Store Keeper and was selected as a Pharmacist (AIR 61) for ESIC. Additionally, I was the Runner-Up in Round 2 of the EY Case Study Competition.
At PharmacyFreak.com, I aim to guide future pharmacists through expert content, exam strategies, and insightful resources based on real experience and academic excellence.
Mail- harsh@pharmacyfreak.com