Table of Contents
Bumetanide is a potent loop diuretic, structurally related to furosemide but approximately 40 times more potent. It is used in the management of edema associated with heart failure, liver cirrhosis, nephrotic syndrome, and renal impairment, as well as acute pulmonary edema.
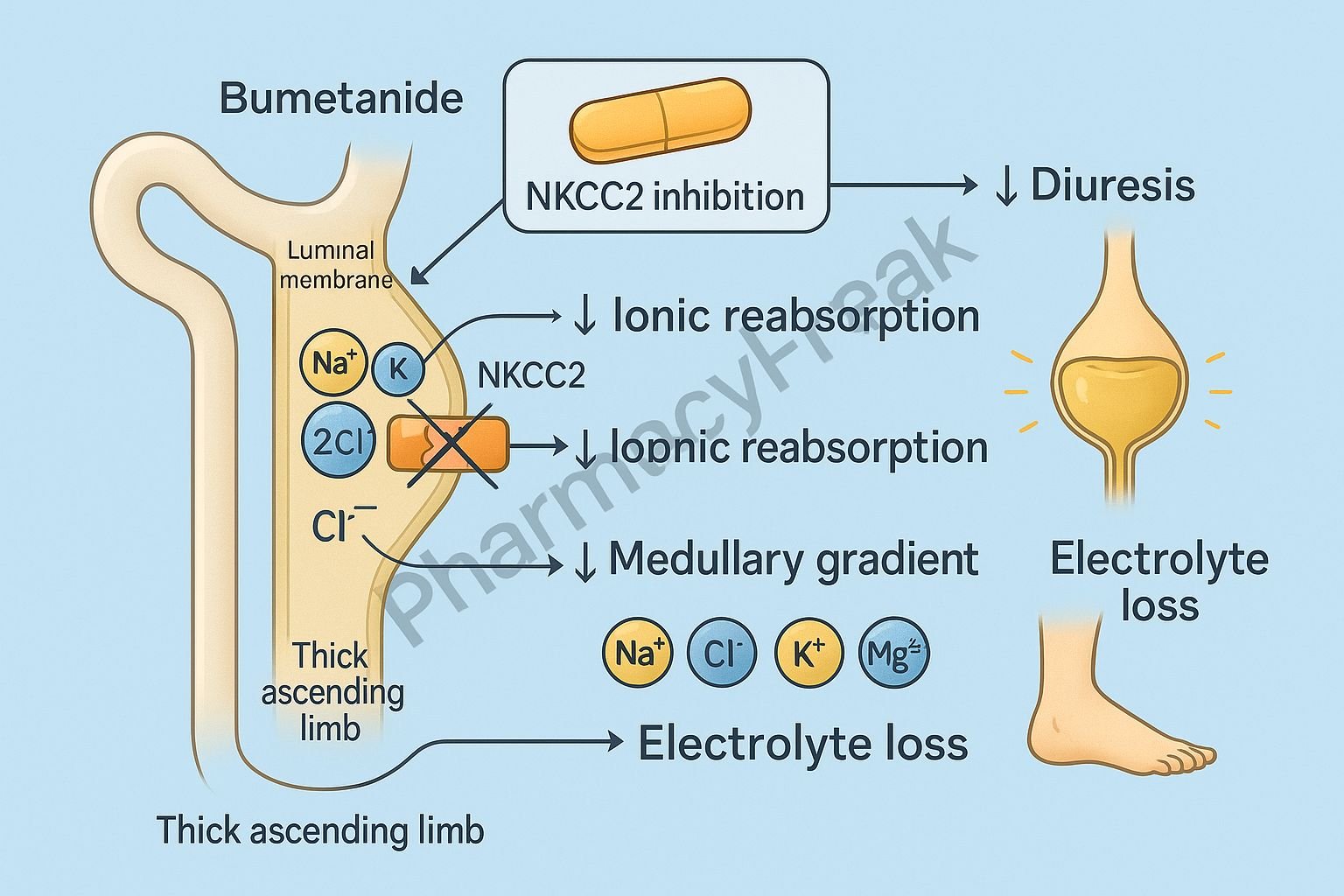
The Mechanism of Action of Bumetanide involves inhibition of sodium, potassium, and chloride reabsorption in the thick ascending limb (TAL) of the loop of Henle, leading to significant diuresis, natriuresis, and reduced extracellular fluid volume.


Mechanism of Action (Step-wise)
1. Inhibition of Na⁺/K⁺/2Cl⁻ Cotransporter (NKCC2) – Primary Mechanism
Bumetanide selectively blocks the NKCC2 transporter in the thick ascending limb.
Effects:
- ↓ Reabsorption of Na⁺, K⁺, and Cl⁻
- ↑ Delivery of NaCl to distal nephron
- ↑ Diuresis and natriuresis
This is the hallmark mechanism of loop diuretics.
2. Abolition of Medullary Concentration Gradient
The thick ascending limb normally contributes to the countercurrent multiplier system.
Bumetanide → inhibition of NKCC2 →
- ↓ Medullary hypertonicity
- ↓ Ability of kidney to concentrate urine
Effect: Production of large volumes of dilute urine.
3. Increased Mg²⁺ and Ca²⁺ Excretion
NKCC2 inhibition reduces the positive luminal potential, decreasing paracellular reabsorption of:
- Calcium
- Magnesium
Effect: Increased Ca²⁺ and Mg²⁺ loss in urine.
4. Enhanced Prostaglandin Synthesis
Loop diuretics stimulate renal PGE₂ production.
Effects:
- ↑ Renal blood flow
- ↓ Renal vascular resistance
- Augmented diuretic effect
NSAIDs blunt this effect and reduce diuretic response.
5. Potassium and Hydrogen Loss
Increased Na⁺ delivery to distal tubule →
- ↑ Na⁺ reabsorption in exchange for K⁺ and H⁺
- ↑ Potassium loss → hypokalemia
- ↑ Hydrogen loss → metabolic alkalosis
6. Summary of Mechanism
| Mechanism | Effect |
|---|---|
| NKCC2 inhibition | Massive diuresis, natriuresis |
| ↓ Medullary gradient | Inability to concentrate urine |
| ↑ Ca/Mg excretion | Potential electrolyte imbalance |
| ↑ Prostaglandins | Improved renal perfusion |
| ↑ Distal Na⁺ delivery | Hypokalemia, alkalosis |

Pharmacokinetics
- Absorption: Excellent oral absorption
- Onset: 30–60 min (oral), 5 min (IV)
- Duration: 4–6 hours
- Metabolism: Hepatic
- Excretion: Renal and biliary
- Potency: 1 mg bumetanide ≈ 40 mg furosemide
Clinical Uses
- Edema due to congestive heart failure
- Acute pulmonary edema
- Hepatic cirrhosis edema
- Renal failure (effective even at low GFR)
- Resistant hypertension (adjunct)
- Hypercalcemia
Adverse Effects
- Hypokalemia
- Hyponatremia
- Hypomagnesemia
- Hypocalcemia
- Metabolic alkalosis
- Ototoxicity (dose-dependent; higher risk IV)
- Hyperuricemia → gout
- Hypovolemia/hypotension
Contraindications
- Anuria
- Severe electrolyte depletion
- Sulfonamide allergy (rare cross-reactivity)
Comparative Analysis
| Feature | Bumetanide | Furosemide | Torsemide |
|---|---|---|---|
| Potency | Highest | Moderate | High |
| Oral bioavailability | High | Variable | High |
| Duration | 4–6 hr | 4–6 hr | 12–16 hr |
| Use at low GFR | Excellent | Good | Excellent |
MCQs
1. Bumetanide acts primarily by inhibiting:
a) Na⁺/Cl⁻ cotransporter
b) NKCC2 cotransporter
c) ENaC channels
d) Na⁺/K⁺ ATPase
Answer: b) NKCC2 cotransporter
2. Bumetanide causes loss of calcium and magnesium by:
a) Blocking aldosterone receptors
b) Reducing positive luminal potential
c) Inhibiting PGE₂ synthesis
d) Increasing ADH release
Answer: b) Reducing positive luminal potential
3. NSAIDs reduce the action of bumetanide by inhibiting:
a) Prostaglandin E₂ synthesis
b) Renin release
c) Aldosterone
d) Vasopressin
Answer: a) Prostaglandin E₂ synthesis
4. Major toxicity of bumetanide:
a) Hepatotoxicity
b) Ototoxicity
c) Severe hypoglycemia
d) Hypercalcemia
Answer: b) Ototoxicity
5. Bumetanide remains effective in:
a) Anuria
b) Low GFR states
c) Addison’s disease
d) Hyperkalemia
Answer: b) Low GFR states
FAQs
Q1. Is bumetanide stronger than furosemide?
Yes—approximately 40 times more potent.
Q2. Can bumetanide be used in renal failure?
Yes—it remains effective even when GFR is low.
Q3. Does bumetanide cause hypokalemia?
Yes, due to increased distal Na⁺ delivery.
Q4. Why monitor hearing with high-dose IV therapy?
Risk of ototoxicity, especially when combined with aminoglycosides.
Q5. Can bumetanide treat hypercalcemia?
Yes—by increasing urinary calcium excretion.
References
Goodman & Gilman’s Pharmacological Basis of Therapeutics
https://accesspharmacy.mhmedical.com/book.aspx?bookid=2189
Katzung: Basic and Clinical Pharmacology
https://accessmedicine.mhmedical.com/book.aspx?bookid=2464
Tripathi: Essentials of Medical Pharmacology
https://jaypeebrothers.com/
Harrison’s Principles of Internal Medicine
https://accessmedicine.mhmedical.com/book.aspx?bookid=2129

I am pursuing MBA in pharmaceutical management from NIPER Hyderabad with a strong academic record and proven success in national-level pharmacy entrance exams. I secured AIR 61 in NIPER 2024 (MS/M.Pharm) and AIR 27 in NIPER MBA, along with AIR 147 in GPAT 2024 and AIR 907 in GPAT 2023. I also achieved AIR 6 in AIIMS CRE-2025 for Drug Store Keeper and was selected as a Pharmacist (AIR 61) for ESIC. Additionally, I was the Runner-Up in Round 2 of the EY Case Study Competition.
At PharmacyFreak.com, I aim to guide future pharmacists through expert content, exam strategies, and insightful resources based on real experience and academic excellence.
Mail- harsh@pharmacyfreak.com