Table of Contents
Introduction
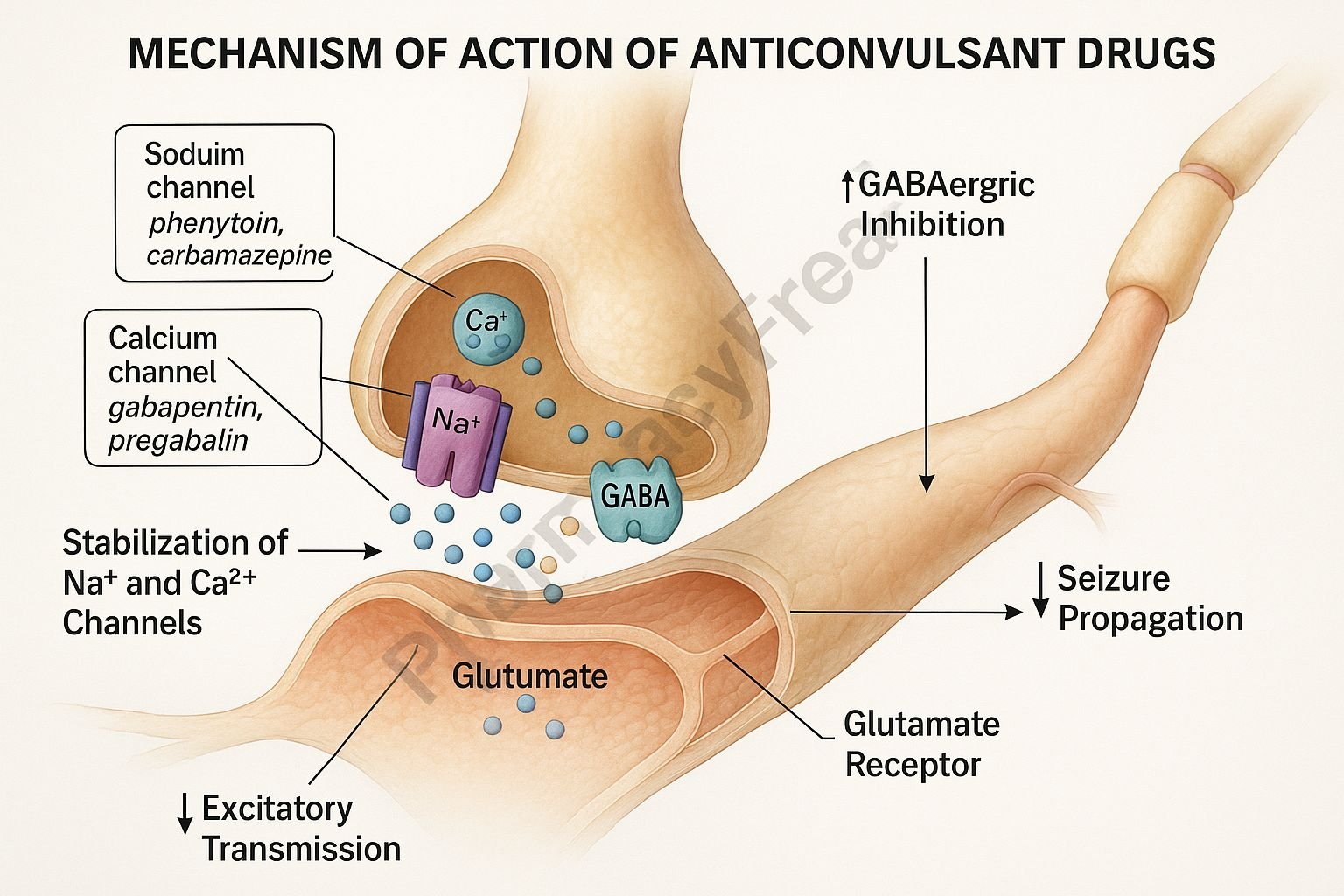
Anticonvulsant drugs, also called antiepileptic drugs (AEDs), are agents that suppress abnormal electrical discharges in the brain to prevent or reduce the frequency of seizures. Mechanism of Action of Anticonvulsant Drugs involves stabilizing neuronal membranes, modulating ion channels, and enhancing inhibitory neurotransmission (primarily GABAergic) while reducing excitatory neurotransmission (glutamatergic). These drugs are used for managing epilepsy, bipolar disorder, neuropathic pain, and migraine prophylaxis.
Mechanism of Action (Step-wise)
Anticonvulsant drugs act by targeting specific molecular mechanisms that regulate neuronal excitability.
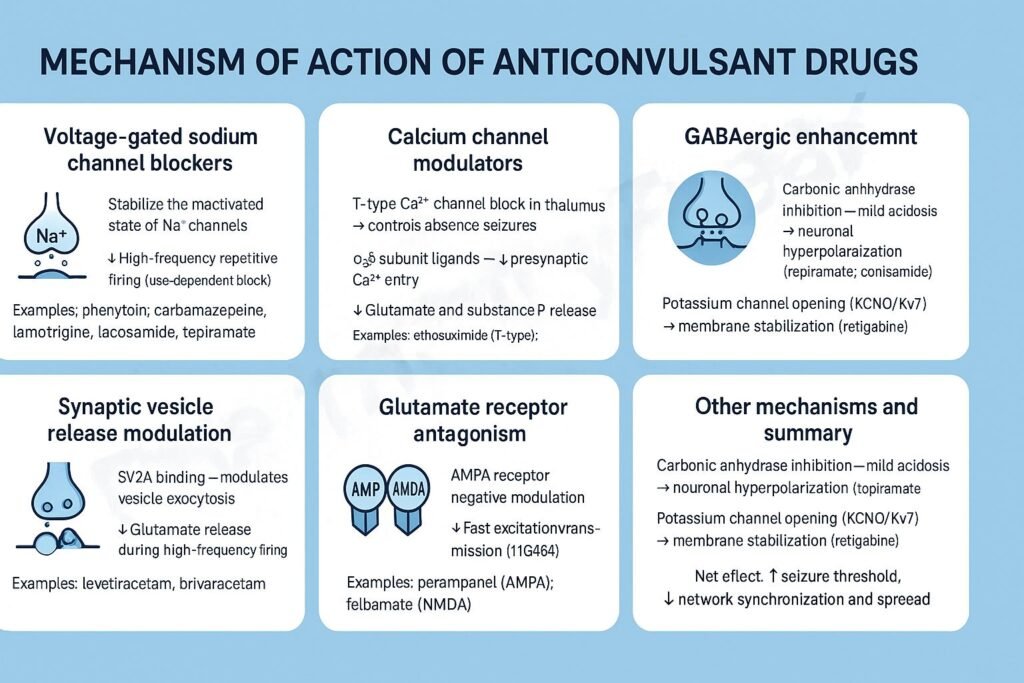
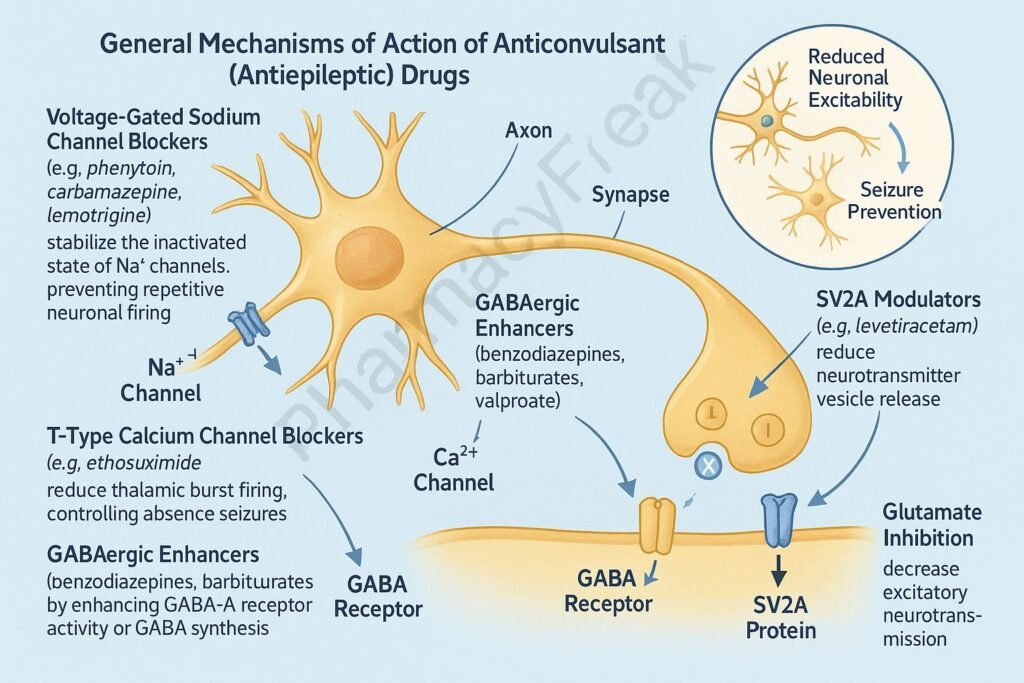
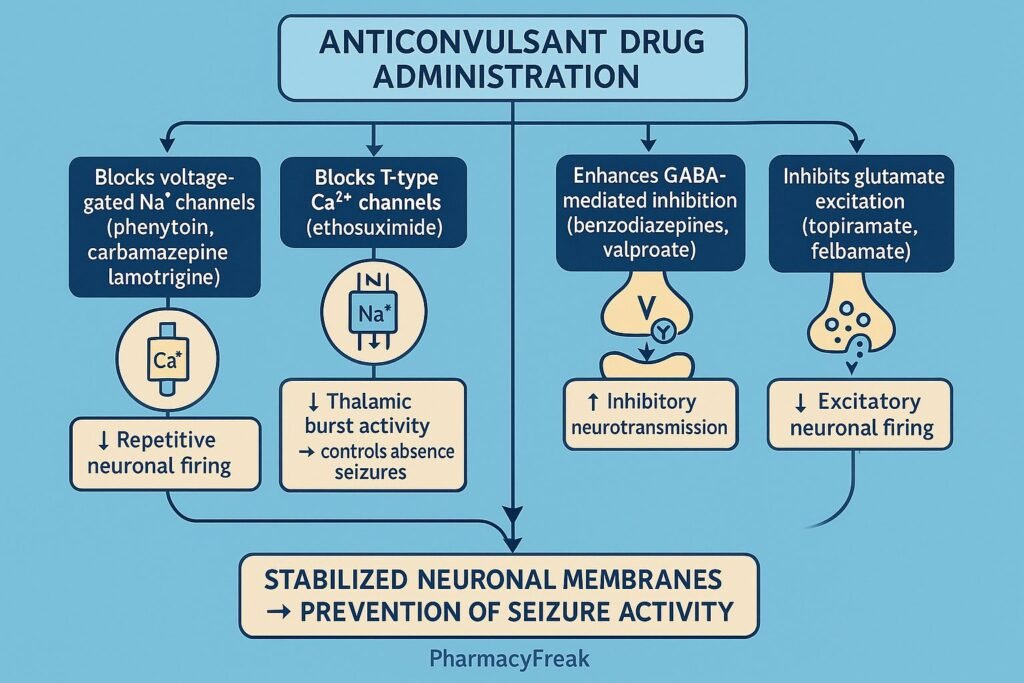
1. Modulation of Voltage-Gated Sodium Channels
- Mechanism:
- These drugs stabilize the inactive state of voltage-gated Na⁺ channels, reducing repetitive firing of neurons.
- This limits propagation of abnormal electrical discharges.
- Examples:
- Phenytoin, Carbamazepine, Lamotrigine, Valproate, Topiramate, Lacosamide.
- Effect:
- Decreased neuronal excitability and prevention of seizure spread.
2. Enhancement of GABA-Mediated Inhibition
- Mechanism:
- GABA (γ-aminobutyric acid) is the main inhibitory neurotransmitter in the CNS.
- Anticonvulsants either increase GABA concentration, enhance its receptor activity, or inhibit its degradation/reuptake.
- Examples:
- GABA enhancement: Benzodiazepines (Diazepam, Clonazepam), Barbiturates (Phenobarbital).
- GABA reuptake inhibition: Tiagabine.
- GABA transaminase inhibition: Vigabatrin.
- Effect:
- Increased inhibitory tone → reduced neuronal firing → anticonvulsant effect.
3. Inhibition of Voltage-Gated Calcium Channels
- Mechanism:
- Block T-type calcium channels in thalamic neurons (important in absence seizures).
- Reduces burst firing and thalamocortical oscillations.
- Examples:
- Ethosuximide, Valproate, Zonisamide.
- Effect:
- Suppression of spike-and-wave discharges typical of absence seizures.
4. Antagonism of Excitatory Glutamate Activity
- Mechanism:
- Inhibits excitatory neurotransmission mediated by glutamate, acting on NMDA and AMPA receptors.
- Examples:
- Topiramate, Felbamate, Perampanel.
- Effect:
- Reduces excessive excitatory activity that leads to seizure propagation.
5. Opening of Potassium Channels (Hyperpolarization)
- Mechanism:
- Enhances K⁺ efflux or opens K⁺ channels to stabilize neuronal membranes and reduce excitability.
- Examples:
- Retigabine (Ezogabine).
- Effect:
- Hyperpolarization → decreased neuronal firing.
6. Multiple Mechanisms (Broad-Spectrum Drugs)
- Valproate: Blocks Na⁺ channels, inhibits T-type Ca²⁺ channels, enhances GABA activity.
- Topiramate: Blocks Na⁺ channels, enhances GABA, and antagonizes glutamate receptors.
- Lamotrigine: Inhibits Na⁺ channels and glutamate release.
Summary Table of Mechanisms
| Mechanism | Primary Drugs | Effect |
|---|---|---|
| Sodium channel blockade | Phenytoin, Carbamazepine, Lamotrigine, Valproate | Decreased neuronal excitability |
| Calcium channel inhibition (T-type) | Ethosuximide, Valproate, Zonisamide | Control of absence seizures |
| GABA enhancement | Benzodiazepines, Barbiturates, Tiagabine, Vigabatrin | Increased inhibition |
| Glutamate antagonism | Topiramate, Felbamate, Perampanel | Reduced excitation |
| Potassium channel activation | Retigabine | Membrane hyperpolarization |
| Mixed mechanism | Valproate, Topiramate, Lamotrigine | Broad-spectrum seizure control |
MCQs
1. The main mechanism of phenytoin is:
a) Sodium channel blockade
b) Calcium channel inhibition
c) GABA receptor activation
d) Glutamate receptor blockade
Answer: a) Sodium channel blockade
2. Ethosuximide acts by blocking:
a) Na⁺ channels
b) T-type Ca²⁺ channels
c) K⁺ channels
d) NMDA receptors
Answer: b) T-type Ca²⁺ channels
3. GABA transaminase is inhibited by:
a) Tiagabine
b) Vigabatrin
c) Diazepam
d) Phenobarbital
Answer: b) Vigabatrin
4. Which drug increases GABA concentration by inhibiting reuptake?
a) Tiagabine
b) Ethosuximide
c) Carbamazepine
d) Lamotrigine
Answer: a) Tiagabine
5. Valproate acts through:
a) Single mechanism
b) Multiple mechanisms
c) Calcium channel opening
d) Glutamate stimulation
Answer: b) Multiple mechanisms
6. Which anticonvulsant enhances chloride channel opening through GABA-A receptors?
a) Diazepam
b) Phenytoin
c) Carbamazepine
d) Topiramate
Answer: a) Diazepam
7. Retigabine acts by:
a) Blocking Na⁺ channels
b) Opening K⁺ channels
c) Enhancing GABA binding
d) Blocking Ca²⁺ channels
Answer: b) Opening K⁺ channels
8. A drug effective in absence seizures is:
a) Ethosuximide
b) Phenytoin
c) Carbamazepine
d) Diazepam
Answer: a) Ethosuximide
9. Which anticonvulsant blocks glutamate receptors?
a) Topiramate
b) Phenytoin
c) Diazepam
d) Valproate
Answer: a) Topiramate
10. The mechanism of lamotrigine involves:
a) Na⁺ channel blockade and ↓ glutamate release
b) GABA inhibition
c) NMDA receptor activation
d) K⁺ channel closure
Answer: a) Na⁺ channel blockade and ↓ glutamate release
FAQs
Q1. What are anticonvulsant drugs?
They are medications that prevent or reduce seizure activity by suppressing abnormal neuronal discharges.
Q2. How do anticonvulsants prevent seizures?
By modulating ion channels, enhancing inhibitory neurotransmission, and suppressing excitatory pathways.
Q3. Which anticonvulsants act on GABA receptors?
Benzodiazepines (e.g., Diazepam) and barbiturates (e.g., Phenobarbital).
Q4. Which drug is preferred for absence seizures?
Ethosuximide and Valproate are first-line choices.
Q5. Why is monitoring required for some AEDs?
To avoid toxicity and drug interactions, especially with phenytoin, carbamazepine, and valproate.
Q6. What are common side effects of anticonvulsants?
Drowsiness, dizziness, ataxia, nausea, liver dysfunction, and teratogenicity (notably with valproate).
References
- Goodman & Gilman’s The Pharmacological Basis of Therapeutics
- Katzung’s Basic and Clinical Pharmacology
- Harrison’s Principles of Internal Medicine
- Tripathi KD, Essentials of Medical Pharmacology
Related Internal Links

I am pursuing MBA in pharmaceutical management from NIPER Hyderabad with a strong academic record and proven success in national-level pharmacy entrance exams. I secured AIR 61 in NIPER 2024 (MS/M.Pharm) and AIR 27 in NIPER MBA, along with AIR 147 in GPAT 2024 and AIR 907 in GPAT 2023. I also achieved AIR 6 in AIIMS CRE-2025 for Drug Store Keeper and was selected as a Pharmacist (AIR 61) for ESIC. Additionally, I was the Runner-Up in Round 2 of the EY Case Study Competition.
At PharmacyFreak.com, I aim to guide future pharmacists through expert content, exam strategies, and insightful resources based on real experience and academic excellence.
Mail- harsh@pharmacyfreak.com