Table of Contents
Introduction
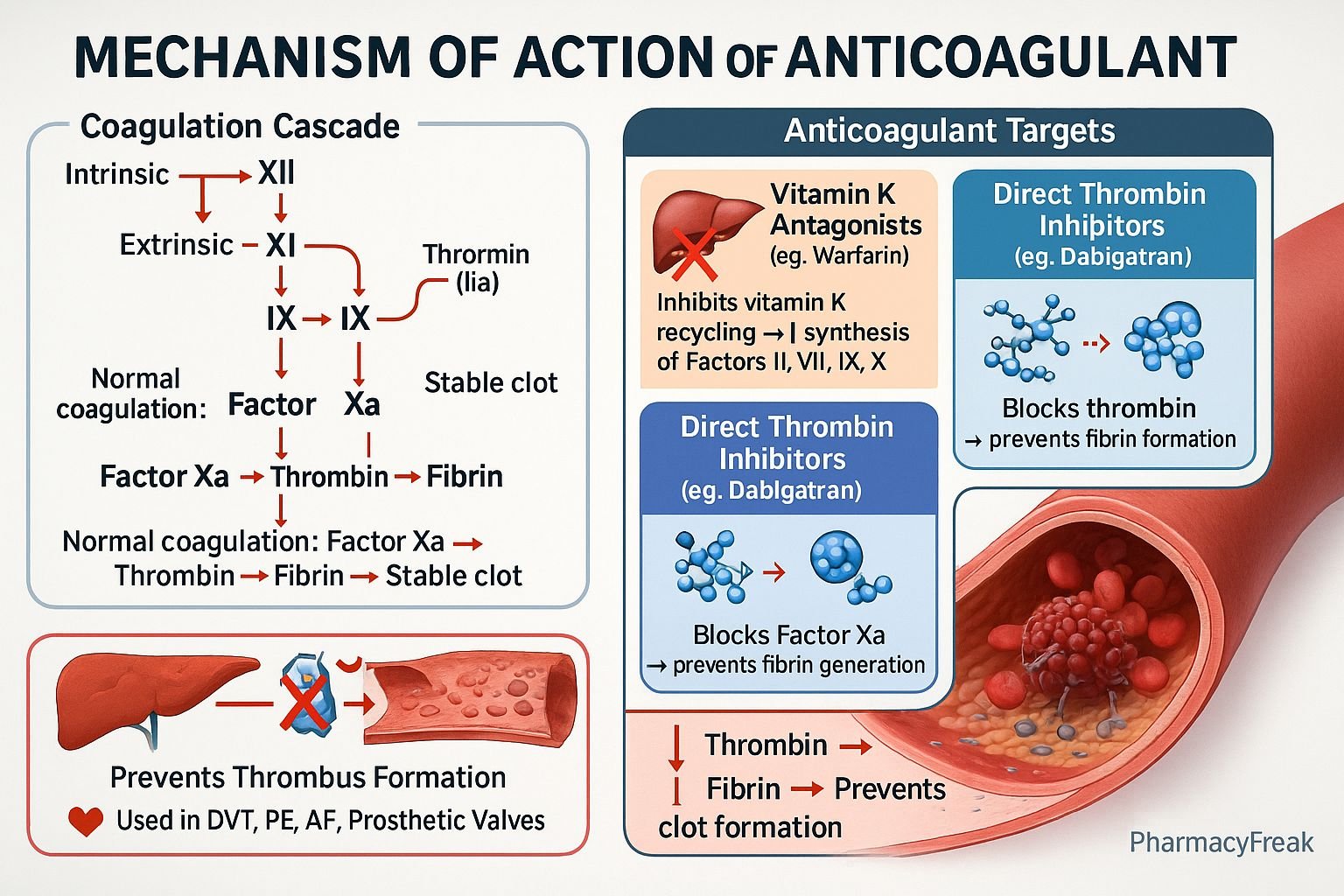
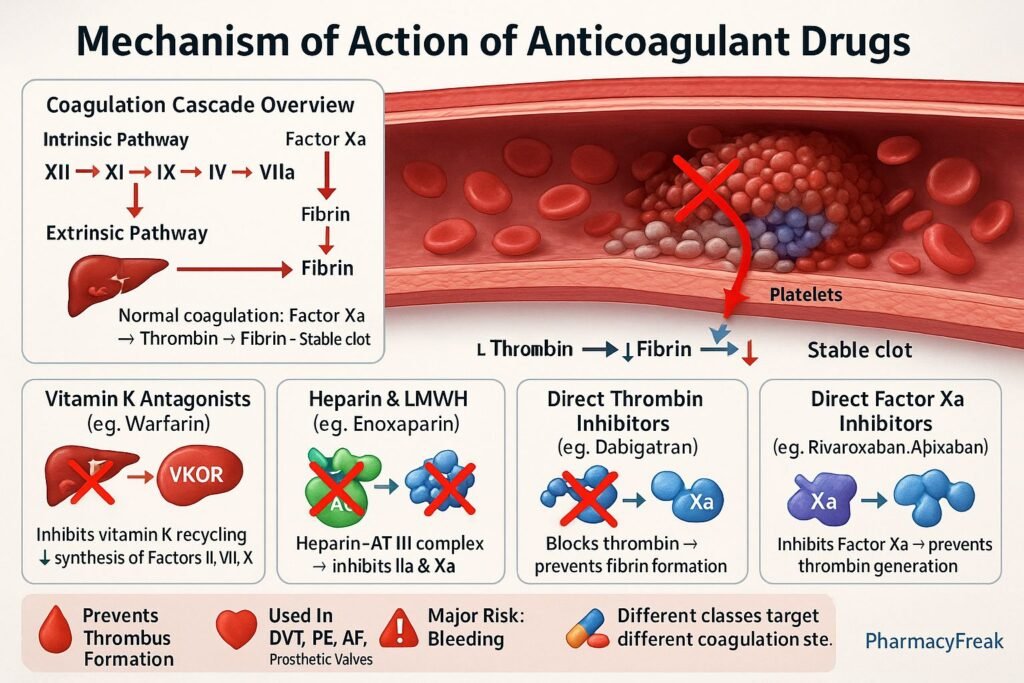
Anticoagulants are blood-thinning agents that prevent the formation and extension of blood clots (thrombi) in the vascular system. Mechanism of Action of Anticoagulant Drugs involves inhibition of key factors in the coagulation cascade, thereby interfering with fibrin clot formation. Unlike thrombolytics, which dissolve existing clots, anticoagulants prevent new clot formation and are essential in conditions such as deep vein thrombosis (DVT), pulmonary embolism (PE), atrial fibrillation, prosthetic heart valves, and myocardial infarction.
Mechanism of Action (Step-wise)
Anticoagulants work by interfering with different stages of the coagulation pathway—either by inhibiting vitamin K-dependent factors, thrombin, or factor Xa.
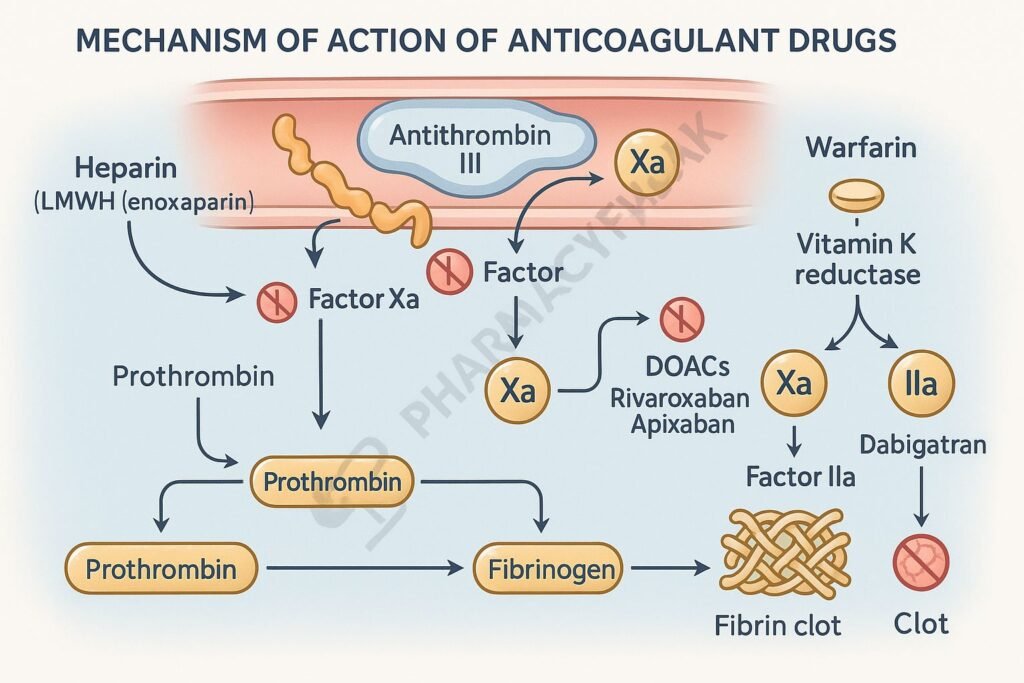
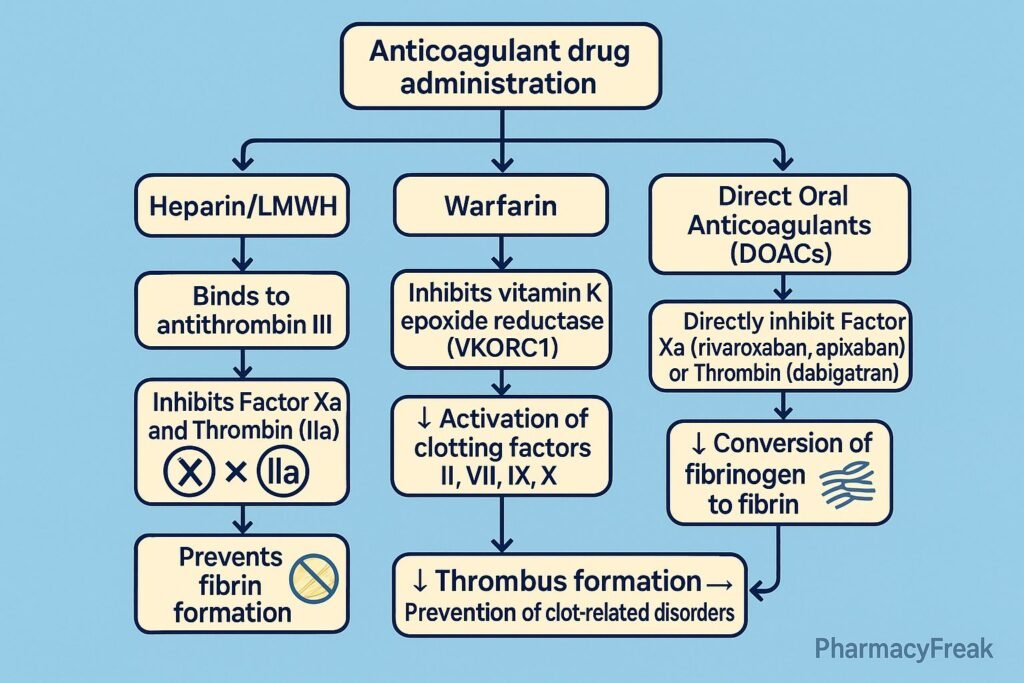
1. Inhibition of Vitamin K–Dependent Factors (Warfarin and Analogues)
- Target: Vitamin K epoxide reductase complex (VKORC1) in the liver.
- Mechanism: Warfarin inhibits VKORC1, preventing the regeneration of reduced vitamin K.
- This inhibits synthesis of vitamin K–dependent clotting factors II, VII, IX, and X, as well as protein C and S.
- Effect: Impaired γ-carboxylation → inactive clotting factors → reduced fibrin formation.
- Onset: Delayed (36–72 hours) as preformed clotting factors are degraded.
2. Potentiation of Antithrombin III (Heparin and Derivatives)
- Target: Antithrombin III (AT III).
- Mechanism: Heparin binds to AT III and enhances its inhibitory activity 1000-fold.
- This leads to inactivation of thrombin (factor IIa) and factor Xa, as well as IXa, XIa, and XIIa.
- Effect: Prevents conversion of fibrinogen to fibrin → anticoagulation.
- Unfractionated Heparin (UFH): Inhibits both Xa and IIa.
- Low-Molecular-Weight Heparins (LMWH): Preferentially inhibit factor Xa (e.g., Enoxaparin, Dalteparin).
- Fondaparinux: Synthetic pentasaccharide that selectively inhibits factor Xa through AT III activation.
3. Direct Thrombin Inhibitors (DTIs)
- Target: Thrombin (factor IIa).
- Mechanism: Directly bind to thrombin’s active site, inhibiting conversion of fibrinogen to fibrin.
- Examples: Dabigatran, Bivalirudin, Argatroban.
- Effect: Prevents fibrin clot formation and platelet activation.
- Advantages: Predictable dose-response, no monitoring needed.
4. Direct Factor Xa Inhibitors
- Target: Factor Xa (common pathway).
- Mechanism: Selectively and reversibly inhibit free and clot-bound factor Xa, blocking conversion of prothrombin (II) to thrombin (IIa).
- Examples: Rivaroxaban, Apixaban, Edoxaban.
- Effect: Reduces thrombin generation and clot formation.
- Advantages: Oral use, rapid onset, no routine coagulation monitoring.
5. Other Mechanisms
- Danaparoid: Inhibits factors Xa and IIa via antithrombin activation.
- Coumarin derivatives: Inhibit vitamin K metabolism similar to warfarin.
- Novel oral anticoagulants (NOACs/DOACs): Directly inhibit Xa or IIa without affecting vitamin K cycle.
Summary Table of Anticoagulant Mechanisms
| Class | Example Drugs | Target/Mechanism | Effect |
|---|---|---|---|
| Vitamin K antagonists | Warfarin | Inhibit VKORC1 → ↓ Factors II, VII, IX, X | Prevent fibrin formation |
| Heparins | Heparin, Enoxaparin | Potentiate AT III → inhibit IIa, Xa | Rapid anticoagulation |
| Direct thrombin inhibitors | Dabigatran, Argatroban | Block thrombin active site | Prevent fibrinogen → fibrin |
| Direct factor Xa inhibitors | Rivaroxaban, Apixaban | Inhibit factor Xa | ↓ Thrombin generation |
| Synthetic pentasaccharides | Fondaparinux | Activate AT III → inhibit Xa | Selective Xa inhibition |
MCQs
1. Warfarin inhibits which enzyme?
a) Thrombin
b) Vitamin K epoxide reductase
c) Factor Xa
d) Plasmin
Answer: b) Vitamin K epoxide reductase
2. Heparin acts by:
a) Direct inhibition of thrombin
b) Potentiating antithrombin III activity
c) Blocking vitamin K metabolism
d) Inhibiting platelet aggregation
Answer: b) Potentiating antithrombin III activity
3. The anticoagulant with the fastest onset of action is:
a) Warfarin
b) Heparin
c) Rivaroxaban
d) Dabigatran
Answer: b) Heparin
4. Low-molecular-weight heparins mainly inhibit:
a) Thrombin
b) Factor Xa
c) Factor IXa
d) Factor XIIa
Answer: b) Factor Xa
5. Which drug directly inhibits thrombin?
a) Dabigatran
b) Warfarin
c) Enoxaparin
d) Rivaroxaban
Answer: a) Dabigatran
6. The anticoagulant that requires INR monitoring is:
a) Heparin
b) Warfarin
c) Rivaroxaban
d) Dabigatran
Answer: b) Warfarin
7. The antidote for heparin overdose is:
a) Protamine sulfate
b) Vitamin K
c) Idarucizumab
d) Andexanet alfa
Answer: a) Protamine sulfate
8. The antidote for dabigatran toxicity is:
a) Andexanet alfa
b) Vitamin K
c) Idarucizumab
d) Protamine sulfate
Answer: c) Idarucizumab
9. Which drug inhibits both free and clot-bound factor Xa?
a) Apixaban
b) Warfarin
c) Dabigatran
d) Heparin
Answer: a) Apixaban
10. Warfarin is contraindicated in:
a) Pregnancy
b) Deep vein thrombosis
c) Atrial fibrillation
d) Pulmonary embolism
Answer: a) Pregnancy
FAQs
Q1. How do anticoagulants differ from antiplatelet drugs?
Anticoagulants act on the coagulation cascade, while antiplatelet drugs inhibit platelet aggregation.
Q2. Why does warfarin have a delayed onset of action?
It inhibits synthesis of new clotting factors but does not affect pre-existing ones, which must degrade first.
Q3. Can anticoagulants dissolve clots?
No, they prevent further clot formation; fibrinolytic agents like alteplase are needed to dissolve clots.
Q4. What lab test is used to monitor heparin therapy?
Activated Partial Thromboplastin Time (aPTT).
Q5. What lab test monitors warfarin therapy?
Prothrombin Time (PT)/INR.
Q6. Which anticoagulants do not require regular monitoring?
Direct oral anticoagulants (DOACs) like Apixaban and Dabigatran.
References
- Goodman & Gilman’s The Pharmacological Basis of Therapeutics
- Katzung’s Basic and Clinical Pharmacology
- Harrison’s Principles of Internal Medicine
- Tripathi KD, Essentials of Medical Pharmacology

I am pursuing MBA in pharmaceutical management from NIPER Hyderabad with a strong academic record and proven success in national-level pharmacy entrance exams. I secured AIR 61 in NIPER 2024 (MS/M.Pharm) and AIR 27 in NIPER MBA, along with AIR 147 in GPAT 2024 and AIR 907 in GPAT 2023. I also achieved AIR 6 in AIIMS CRE-2025 for Drug Store Keeper and was selected as a Pharmacist (AIR 61) for ESIC. Additionally, I was the Runner-Up in Round 2 of the EY Case Study Competition.
At PharmacyFreak.com, I aim to guide future pharmacists through expert content, exam strategies, and insightful resources based on real experience and academic excellence.
Mail- harsh@pharmacyfreak.com