Table of Contents
Introduction
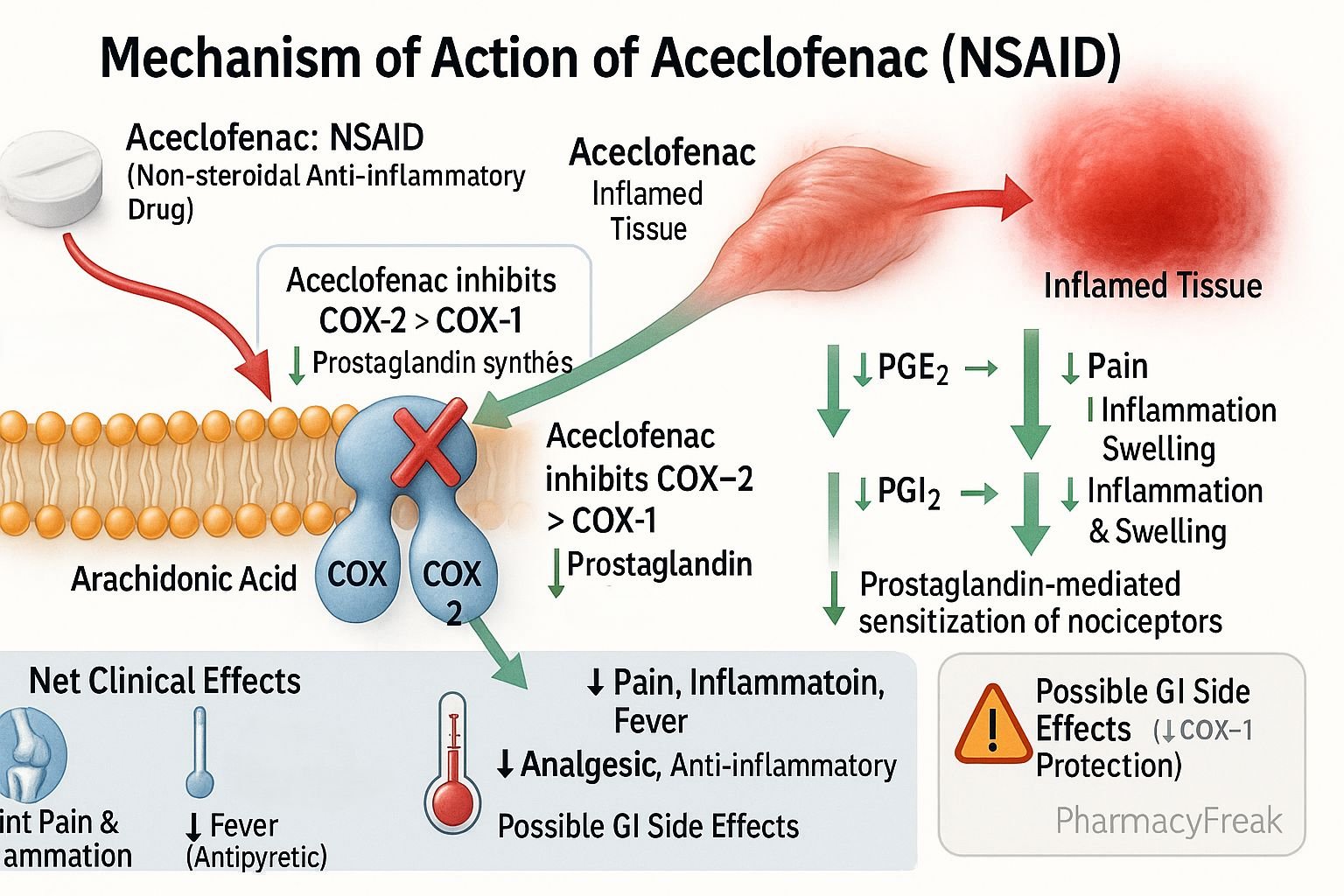
Aceclofenac is a widely used nonsteroidal anti-inflammatory drug (NSAID) indicated for pain relief and reduction of inflammation in musculoskeletal and joint disorders. Mechanism of Action of Aceclofenac primarily involves inhibition of cyclooxygenase (COX) enzymes, leading to reduced prostaglandin synthesis. It is often preferred for its relatively better gastrointestinal tolerability compared to some older NSAIDs. Clinically, aceclofenac is used in osteoarthritis, rheumatoid arthritis, and ankylosing spondylitis, offering effective pain management and anti-inflammatory benefits.
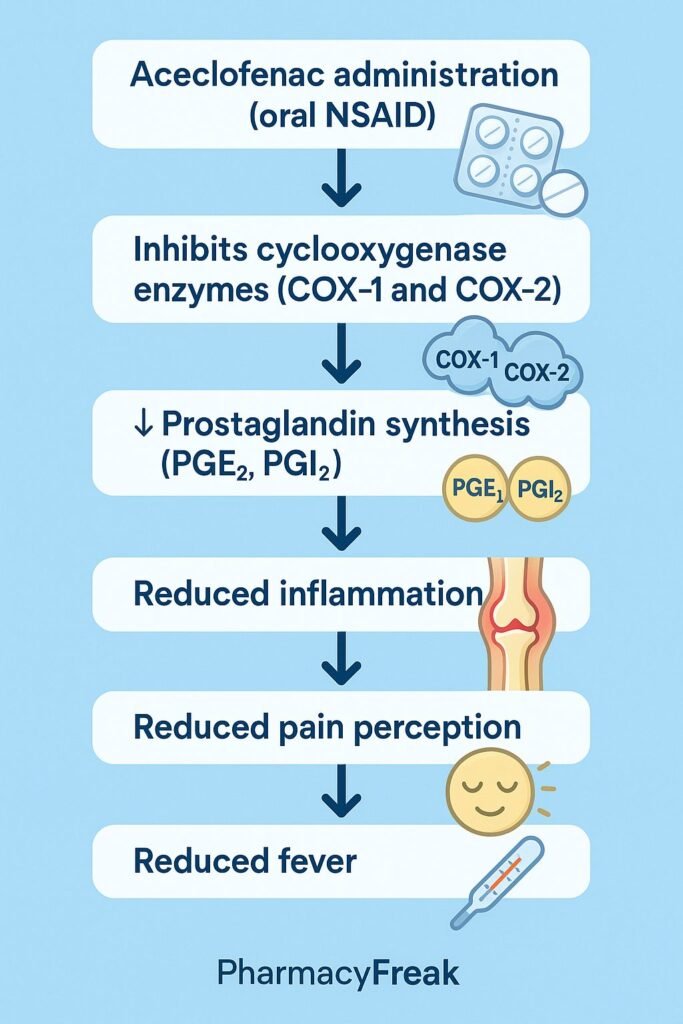
Mechanism of Action (Step-wise)
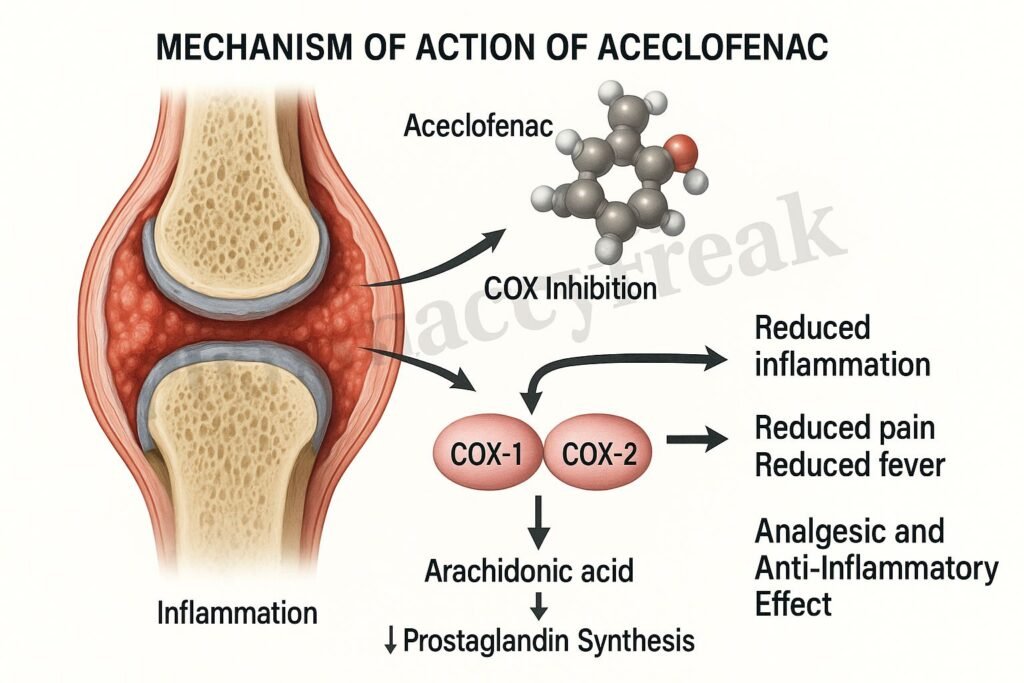
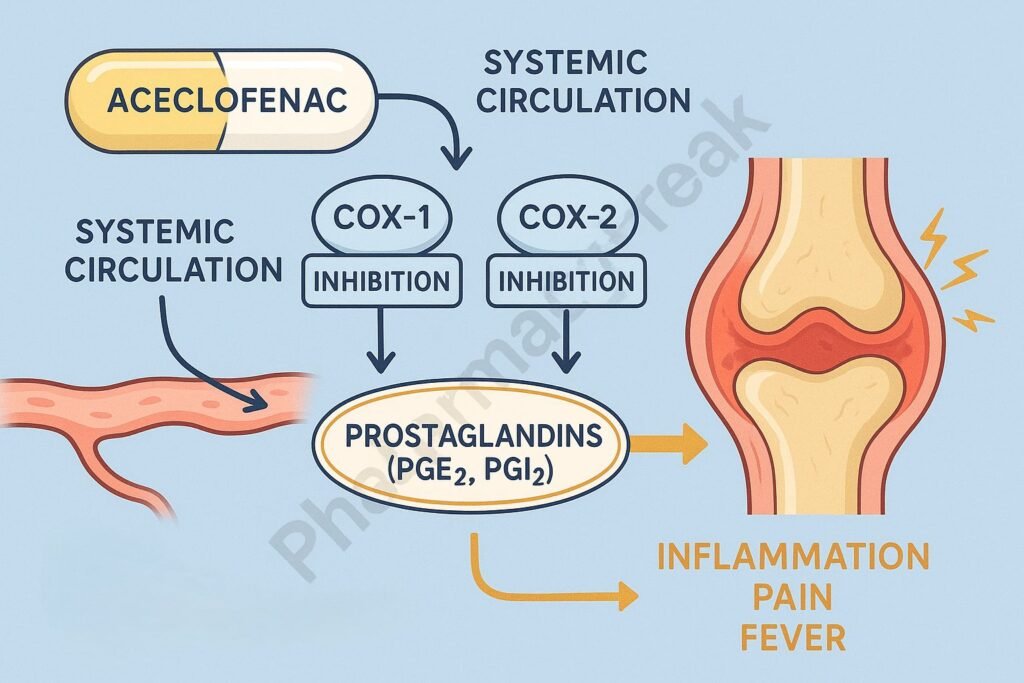
- Inhibition of Cyclooxygenase (COX) Enzymes
- Aceclofenac inhibits cyclooxygenase-2 (COX-2) more selectively than cyclooxygenase-1 (COX-1).
- This reduces production of pro-inflammatory prostaglandins at sites of inflammation.
- Reduced Prostaglandin Synthesis
- Prostaglandins are mediators responsible for pain, swelling, and fever.
- Lower prostaglandin levels result in reduced inflammation and analgesia.
- Stabilization of Inflammatory Cells
- Aceclofenac reduces the release of inflammatory cytokines such as TNF-α and IL-1β.
- Helps control joint inflammation in rheumatoid arthritis and other inflammatory disorders.
- Chondroprotective Action
- Unlike some NSAIDs, aceclofenac may slow down cartilage degeneration.
- Evidence suggests it stimulates synthesis of extracellular matrix components in cartilage.
- Overall Effect
- Analgesic (pain relief).
- Anti-inflammatory (reduces swelling and redness).
- Antipyretic (lowers fever).
Pharmacokinetics
- Absorption: Well absorbed orally; peak plasma concentration within 1–3 hours.
- Distribution: Highly plasma protein bound (~99%).
- Metabolism: Extensively metabolized in the liver to diclofenac (active metabolite).
- Excretion: Excreted mainly in urine as metabolites.
- Half-life: 4–4.5 hours.
Clinical Uses
- Osteoarthritis (pain and stiffness).
- Rheumatoid arthritis.
- Ankylosing spondylitis.
- Musculoskeletal pain and inflammatory conditions.
- Dental pain, postoperative pain, and soft tissue injuries.
Adverse Effects
- Common: Dyspepsia, abdominal pain, nausea, diarrhea.
- Less common: Dizziness, skin rash, edema.
- Serious: Gastrointestinal bleeding, peptic ulcers, hepatotoxicity, nephrotoxicity, cardiovascular risk (hypertension, stroke).
- Contraindications: Peptic ulcer disease, severe hepatic/renal impairment, history of NSAID allergy, pregnancy (especially third trimester).
Comparative Analysis
| Feature | Aceclofenac | Diclofenac | Ibuprofen |
|---|---|---|---|
| COX selectivity | More COX-2 selective | Moderate COX-1/COX-2 | Non-selective |
| GI safety profile | Better than diclofenac | Higher risk of GI irritation | Moderate risk |
| Half-life | 4–4.5 hours | 1–2 hours | 2 hours |
| Chondroprotective effect | Yes (supports cartilage) | Limited | No |
| Common uses | Arthritis, musculoskeletal pain | Arthritis, inflammation | Pain, fever, inflammation |
MCQs
1. Aceclofenac belongs to which class of drugs?
a) Corticosteroid
b) NSAID
c) DMARD
d) Opioid
Answer: b) NSAID
2. The primary mechanism of action of aceclofenac is:
a) Blocking TNF-α receptors
b) Inhibiting cyclooxygenase enzymes
c) Activating serotonin receptors
d) Enhancing opioid receptors
Answer: b) Inhibiting cyclooxygenase enzymes
3. Aceclofenac is metabolized mainly to:
a) Paracetamol
b) Diclofenac
c) Ibuprofen
d) Naproxen
Answer: b) Diclofenac
4. Which condition is aceclofenac most commonly prescribed for?
a) Hypertension
b) Osteoarthritis
c) Diabetes
d) Tuberculosis
Answer: b) Osteoarthritis
5. Which is a serious side effect of aceclofenac?
a) Constipation
b) Gastrointestinal bleeding
c) Drowsiness
d) Weight gain
Answer: b) Gastrointestinal bleeding
6. Aceclofenac shows partial selectivity for which COX isoform?
a) COX-1
b) COX-2
c) Both equally
d) Neither
Answer: b) COX-2
7. What is the elimination half-life of aceclofenac?
a) 1–2 hours
b) 4–4.5 hours
c) 10 hours
d) 24 hours
Answer: b) 4–4.5 hours
8. Which cytokine is reduced by aceclofenac?
a) IL-6
b) TNF-α
c) Interferon-γ
d) IL-12
Answer: b) TNF-α
9. Aceclofenac is contraindicated in:
a) Diabetes mellitus
b) Peptic ulcer disease
c) Hypothyroidism
d) Asthma (always)
Answer: b) Peptic ulcer disease
10. Which feature makes aceclofenac different from many NSAIDs?
a) It is opioid-sparing
b) It has chondroprotective effects
c) It is not protein-bound
d) It acts on opioid receptors
Answer: b) It has chondroprotective effects
FAQs
Q1. Is aceclofenac safer than diclofenac?
Yes, aceclofenac has better gastrointestinal tolerability than diclofenac.
Q2. Can aceclofenac be taken with food?
Yes, it is usually recommended with food to reduce gastric irritation.
Q3. Is aceclofenac safe in pregnancy?
No, especially contraindicated in the third trimester.
Q4. Does aceclofenac affect cartilage?
Yes, it has mild chondroprotective effects compared to other NSAIDs.
Q5. Can aceclofenac cause kidney damage?
Yes, long-term or high-dose use may impair renal function.
Q6. What is the typical dose of aceclofenac?
Usually 100 mg twice daily (oral).
References
- Goodman & Gilman’s The Pharmacological Basis of Therapeutics
- Katzung Basic and Clinical Pharmacology
- Harrison’s Principles of Internal Medicine
- Clinical NSAID safety guidelines
Related Internal Links

I am pursuing MBA in pharmaceutical management from NIPER Hyderabad with a strong academic record and proven success in national-level pharmacy entrance exams. I secured AIR 61 in NIPER 2024 (MS/M.Pharm) and AIR 27 in NIPER MBA, along with AIR 147 in GPAT 2024 and AIR 907 in GPAT 2023. I also achieved AIR 6 in AIIMS CRE-2025 for Drug Store Keeper and was selected as a Pharmacist (AIR 61) for ESIC. Additionally, I was the Runner-Up in Round 2 of the EY Case Study Competition.
At PharmacyFreak.com, I aim to guide future pharmacists through expert content, exam strategies, and insightful resources based on real experience and academic excellence.
Mail- harsh@pharmacyfreak.com