Fungal infections, also known as mycoses, range from superficial skin infections to life-threatening systemic diseases. They are especially problematic in immunocompromised individuals such as those undergoing chemotherapy, organ transplant, or prolonged antibiotic therapy. Antifungal drugs are used to treat these infections and are classified based on their mechanism and site of action.
This blog from Pharmacy Freak outlines the classification of Antifungal Drugs, uses, drug of choice highlights, side effects, and clinical pearls of antifungal therapy based on established pharmacology texts.
Table of Contents
What is Antifungal Drug
Antifungal drugs are agents that kill or inhibit the growth of fungi. They act on fungal cell membranes, cell walls, or nucleic acid synthesis, thereby interfering with fungal survival and replication.
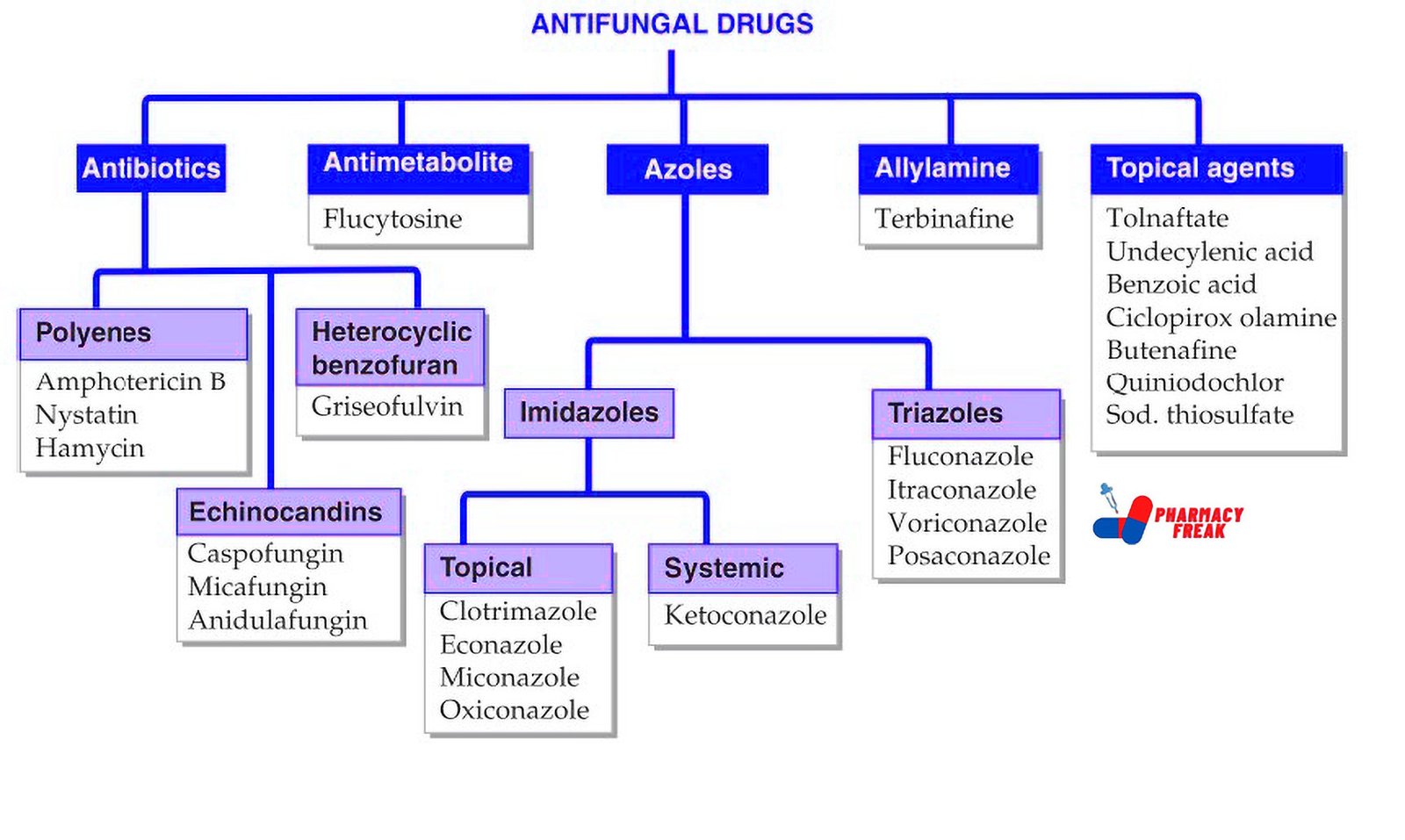
Classification of Antifungal Drug (KD Tripathi)
- Antibiotics –
- Polyenes: Amphotericin B, Nystatin, Hamycin
- Heterocyclic benzofuran: Griseofulvin
- Echinocandins: Caspofungin, Micafungin, Anidulafungin
- Antimetabolite: Flucytosine
- Azoles –
- Imidazoles –
- Topical: Clotrimazole, Econazole, Miconazole, Oxiconazole
- Systemic: Ketoconazole
- Triazoles: Fluconazole, Itraconazole, Voriconazole, Posaconazole
- Imidazoles –
- Allylamine: Terbinafine
- Topical agents: Tolnaftate, Undecylenic acid, Benzoic acid, Ciclopirox olamine, Butenafine, Quiniodochlor, Sodium thiosulfate
Classification of Antifungal Drugs (General)
Antifungal drugs are classified as follows:
- Polyene Antibiotics
Mechanism: Bind to ergosterol in fungal cell membranes, causing leakage of cell contents
Drugs: Amphotericin B, Nystatin, Natamycin
Use:
- Amphotericin B – Systemic mycoses
- Nystatin – Oral and cutaneous candidiasis
- Natamycin – Fungal keratitis
Note: Amphotericin B is fungicidal and considered the most broad-spectrum antifungal
- Azoles
Mechanism: Inhibit fungal cytochrome P450 enzyme, blocking ergosterol synthesis
Subclasses:
a. Imidazoles – Ketoconazole, Clotrimazole, Miconazole
b. Triazoles – Fluconazole, Itraconazole, Voriconazole, Posaconazole
Use:
- Fluconazole – Cryptococcal meningitis, candidiasis
- Itraconazole – Dermatophytosis, histoplasmosis
- Voriconazole – Invasive aspergillosis
- Posaconazole – Mucormycosis, prophylaxis in neutropenic patients
Note: Triazoles have broader activity and better pharmacokinetics than imidazoles
- Echinocandins
Mechanism: Inhibit synthesis of β-1,3-glucan in fungal cell wall
Drugs: Caspofungin, Micafungin, Anidulafungin
Use: Invasive candidiasis, refractory aspergillosis
Note: Reserved for resistant fungal infections - Allylamines
Mechanism: Inhibit squalene epoxidase, interfering with ergosterol synthesis
Drug: Terbinafine
Use: Onychomycosis, dermatophytosis (tinea corporis, tinea cruris)
Note: Oral terbinafine is fungicidal against dermatophytes - Antimetabolite
Mechanism: Inhibits DNA and RNA synthesis
Drug: Flucytosine (5-FC)
Use: Used in combination with Amphotericin B for cryptococcal meningitis
Note: Rapid resistance develops if used alone - Griseofulvin
Mechanism: Inhibits fungal mitosis by disrupting microtubule function
Use: Dermatophytosis of skin, hair, and nails
Note: Replaced by terbinafine and azoles due to better efficacy - Topical Antifungals
Includes drugs acting locally for superficial mycoses
Examples: Clotrimazole, Miconazole, Econazole, Sertaconazole
Use: Tinea infections, candidiasis, pityriasis versicolor
Uses
Antifungal drugs are used in the treatment of:
- Superficial fungal infections (dermatophytosis, oral and vaginal candidiasis)
- Systemic mycoses (histoplasmosis, blastomycosis, cryptococcosis)
- Opportunistic infections in immunocompromised patients (aspergillosis, mucormycosis)
- Fungal keratitis, onychomycosis
- Prophylaxis in neutropenic patients or transplant recipients
Drug of Choice Highlights
- Candidemia (non-neutropenic) – Echinocandins
- Candidiasis (oral/vaginal) – Fluconazole
- Cryptococcal meningitis – Amphotericin B + Flucytosine
- Aspergillosis – Voriconazole
- Mucormycosis – Liposomal Amphotericin B
- Dermatophytosis – Terbinafine (oral)
- Onychomycosis – Terbinafine or Itraconazole
- Tinea versicolor – Topical clotrimazole or oral fluconazole
- Fungal keratitis – Natamycin (topical)
Side Effects
- Amphotericin B – Nephrotoxicity, fever, chills, hypokalemia, anemia
- Azoles – Hepatotoxicity, QT prolongation, GI upset, drug interactions
- Echinocandins – Infusion reactions, elevated liver enzymes
- Flucytosine – Bone marrow suppression, GI toxicity
- Terbinafine – Taste disturbances, hepatotoxicity, rash
- Griseofulvin – Headache, hepatotoxicity, photosensitivity
- Topical agents – Local irritation, contact dermatitis
Updated Clinical Pearls
- Liposomal Amphotericin B has less nephrotoxicity and is preferred in high-risk patients.
- Echinocandins are first-line in invasive candidiasis, especially in critically ill or azole-resistant cases.
- Fluconazole has excellent CNS penetration and is ideal for cryptococcal meningitis.
- Voriconazole should be monitored for visual disturbances and hepatotoxicity.
- Terbinafine is superior to griseofulvin for onychomycosis and tinea infections due to shorter duration and higher cure rate.
- Azoles have significant drug interactions due to CYP450 inhibition and should be used cautiously with other hepatically metabolized drugs.
References
- Tripathi KD. Essentials of Medical Pharmacology. 7th ed. New Delhi: Jaypee Brothers Medical Publishers; 2013. p. 877–887
- Gupta S, Garg A. Review of Pharmacology. 15th ed. New Delhi: Jaypee Brothers Medical Publishers; 2023. p. 300–303
- Brunton LL, Chabner BA, Knollmann BC, editors. Goodman and Gilman’s The Pharmacological Basis of Therapeutics. 12th ed. New York: McGraw-Hill Education; 2011. p. 1579–1588
Related Links

I am a Registered Pharmacist under the Pharmacy Act, 1948, and the founder of PharmacyFreak.com. I hold a Bachelor of Pharmacy degree from Rungta College of Pharmaceutical Science and Research. With a strong academic foundation and practical knowledge, I am committed to providing accurate, easy-to-understand content to support pharmacy students and professionals. My aim is to make complex pharmaceutical concepts accessible and useful for real-world application.
Mail- Sachin@pharmacyfreak.com

thanks for this great information