Table of Contents
Introduction
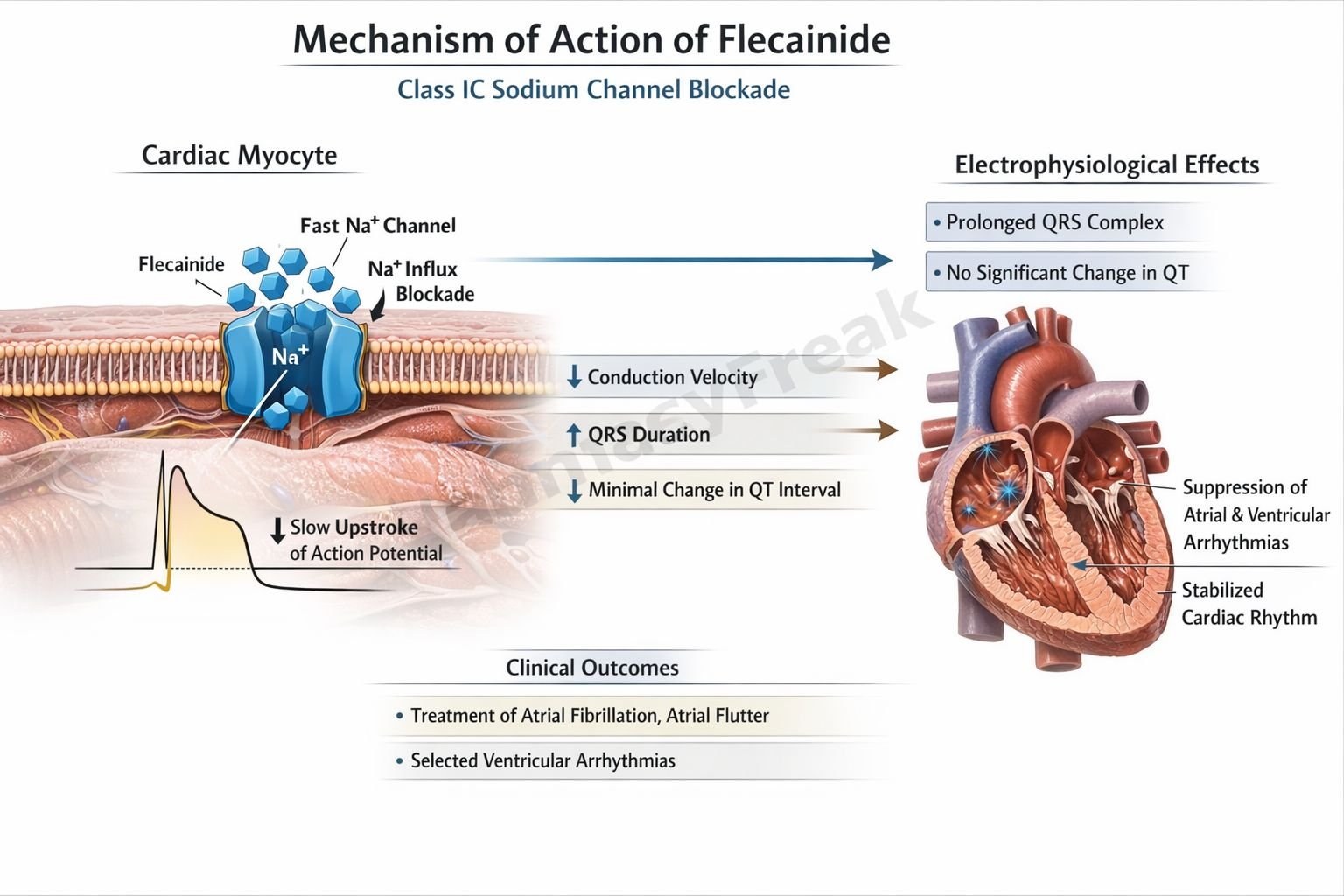
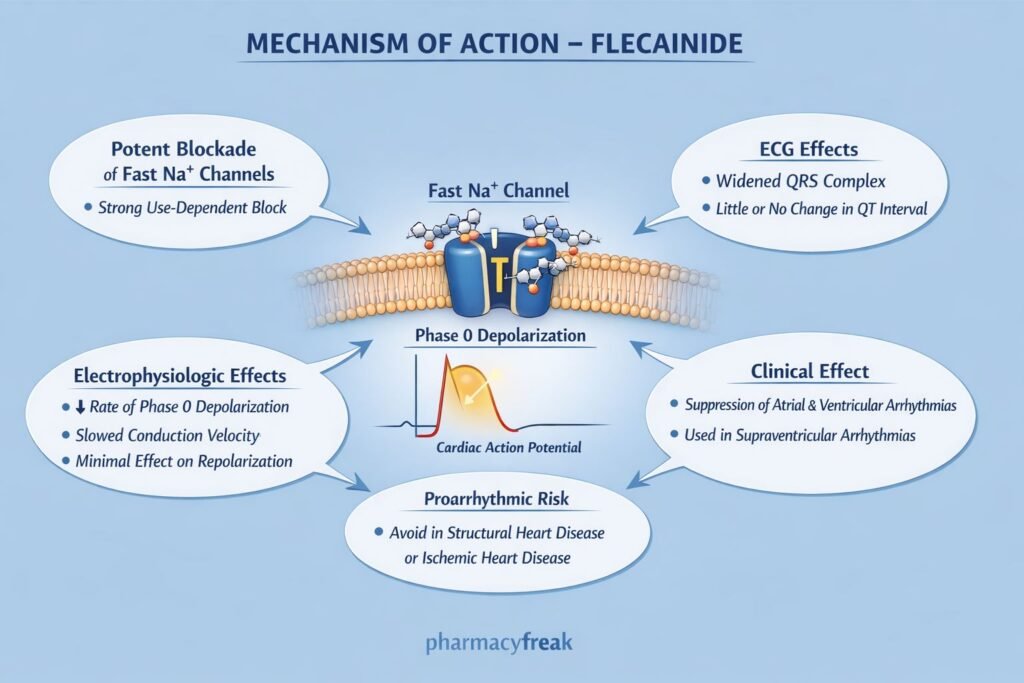
Flecainide is a Class IC antiarrhythmic drug used in the management of supraventricular and selected ventricular arrhythmias. It is a potent sodium channel blocker with strong effects on cardiac conduction velocity and minimal effect on action potential duration. Flecainide is high-yield for pharmacology and cardiology examinations because of its distinctive electrophysiological profile, proarrhythmic risk, and contraindication in structural heart disease.
Mechanism of Action (Step-wise)
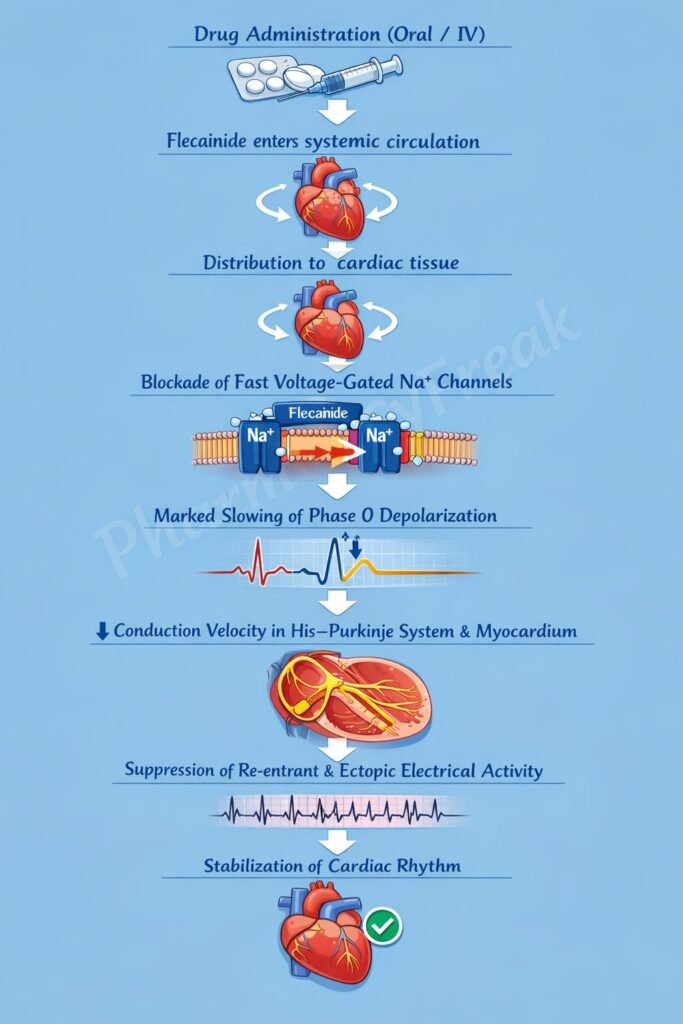
Flecainide suppresses arrhythmias by markedly slowing cardiac impulse conduction.
Step 1: Targeting fast sodium channels
Flecainide binds to fast voltage-gated sodium (Na⁺) channels in cardiac myocytes.
Step 2: Use-dependent sodium channel blockade
It preferentially blocks sodium channels in their open state, especially during rapid heart rates.
Step 3: Marked reduction in phase 0 depolarization
Inhibition of Na⁺ influx significantly decreases the slope of phase 0 of the cardiac action potential.
Step 4: Slowing of conduction velocity
Reduced phase 0 depolarization leads to profound slowing of impulse conduction in atrial, ventricular, and His–Purkinje tissues.
Step 5: Minimal effect on repolarization
Flecainide has little effect on potassium channels, so action potential duration and QT interval are minimally changed.
ECG changes (exam favorite):
- ↑ PR interval
- ↑ QRS duration
- Minimal change in QT interval
Pharmacokinetics
- Route of administration: Oral
- Bioavailability: ~90%
- Protein binding: ~40%
- Distribution: Extensive cardiac tissue penetration
- Metabolism: Hepatic (CYP2D6)
- Half-life: 12–27 hours
- Excretion: Renal and hepatic
- Dose adjustment: Required in renal and hepatic impairment
Clinical Uses
- Paroxysmal atrial fibrillation (rhythm control)
- Paroxysmal supraventricular tachycardia (PSVT)
- Atrial flutter
- Life-threatening ventricular arrhythmias (selected patients)
Important note:
Flecainide is used only in patients without structural heart disease.
Adverse Effects
Cardiac (most important):
- Proarrhythmia
- Ventricular tachycardia
- Ventricular fibrillation
- Worsening heart failure (negative inotropy)
Central nervous system:
- Dizziness
- Blurred vision
- Headache
Gastrointestinal:
- Nausea
- Constipation
Exam warning:
Contraindicated after myocardial infarction due to increased mortality (CAST trial).
Comparative Analysis
Flecainide vs Propafenone vs Amiodarone
| Feature | Flecainide | Propafenone | Amiodarone |
|---|---|---|---|
| Vaughan–Williams class | IC | IC | III (multiple) |
| Na⁺ channel block | Very strong | Strong | Moderate |
| Effect on QRS | Marked ↑ | Moderate ↑ | Mild ↑ |
| QT prolongation | Minimal | Minimal | Marked |
| Proarrhythmic risk | High | Moderate | Low |
| Use in structural heart disease | Contraindicated | Contraindicated | Preferred |
Explanation:
Flecainide produces profound sodium channel blockade, leading to significant conduction slowing and a high proarrhythmic risk in diseased myocardium. Amiodarone, despite multiple toxicities, is safer in structural heart disease.
MCQs
- Flecainide belongs to which antiarrhythmic class?
a) Class IA
b) Class IB
c) Class IC
d) Class III
Answer: c) Class IC
- Flecainide primarily blocks:
a) Potassium channels
b) Calcium channels
c) Sodium channels
d) Chloride channels
Answer: c) Sodium channels
- Main electrophysiological effect of flecainide is:
a) Prolonged repolarization
b) Slowed conduction velocity
c) Increased refractoriness
d) Increased automaticity
Answer: b) Slowed conduction velocity
- Flecainide causes which ECG change?
a) Prolonged QT
b) Narrow QRS
c) Widened QRS
d) Shortened PR
Answer: c) Widened QRS
- Flecainide is contraindicated in:
a) Atrial fibrillation without heart disease
b) Young patients
c) Structural heart disease
d) PSVT
Answer: c) Structural heart disease
- Flecainide shows use-dependence, meaning it:
a) Acts only at rest
b) Blocks channels more at high heart rates
c) Is effective only orally
d) Requires IV loading
Answer: b) Blocks channels more at high heart rates
- Major risk associated with flecainide is:
a) Hepatotoxicity
b) Nephrotoxicity
c) Proarrhythmia
d) Pulmonary fibrosis
Answer: c) Proarrhythmia
- Flecainide metabolism mainly involves:
a) CYP3A4
b) CYP2C9
c) CYP2D6
d) MAO
Answer: c) CYP2D6
- Flecainide has minimal effect on:
a) Phase 0
b) Sodium influx
c) Conduction velocity
d) Repolarization
Answer: d) Repolarization
- Trial that demonstrated increased mortality with flecainide is:
a) SOLVD
b) CAST
c) AFFIRM
d) DIG
Answer: b) CAST
FAQs
1. Why is flecainide dangerous in ischemic heart disease?
Because it increases the risk of fatal ventricular arrhythmias.
2. Does flecainide prolong QT interval?
No, it mainly widens the QRS complex.
3. Is flecainide effective in atrial fibrillation?
Yes, in patients without structural heart disease.
4. Why is flecainide called a strong sodium channel blocker?
Because it markedly suppresses phase 0 depolarization.
5. Can flecainide worsen heart failure?
Yes, due to its negative inotropic effect.
References
- Goodman & Gilman’s The Pharmacological Basis of Therapeutics
https://accesspharmacy.mhmedical.com - Katzung BG. Basic and Clinical Pharmacology
https://accessmedicine.mhmedical.com - Tripathi KD. Essentials of Medical Pharmacology
- Harrison’s Principles of Internal Medicine
https://accessmedicine.mhmedical.com

I am pursuing MBA in pharmaceutical management from NIPER Hyderabad with a strong academic record and proven success in national-level pharmacy entrance exams. I secured AIR 61 in NIPER 2024 (MS/M.Pharm) and AIR 27 in NIPER MBA, along with AIR 147 in GPAT 2024 and AIR 907 in GPAT 2023. I also achieved AIR 6 in AIIMS CRE-2025 for Drug Store Keeper and was selected as a Pharmacist (AIR 61) for ESIC. Additionally, I was the Runner-Up in Round 2 of the EY Case Study Competition.
At PharmacyFreak.com, I aim to guide future pharmacists through expert content, exam strategies, and insightful resources based on real experience and academic excellence.
Mail- harsh@pharmacyfreak.com