Table of Contents
Introduction
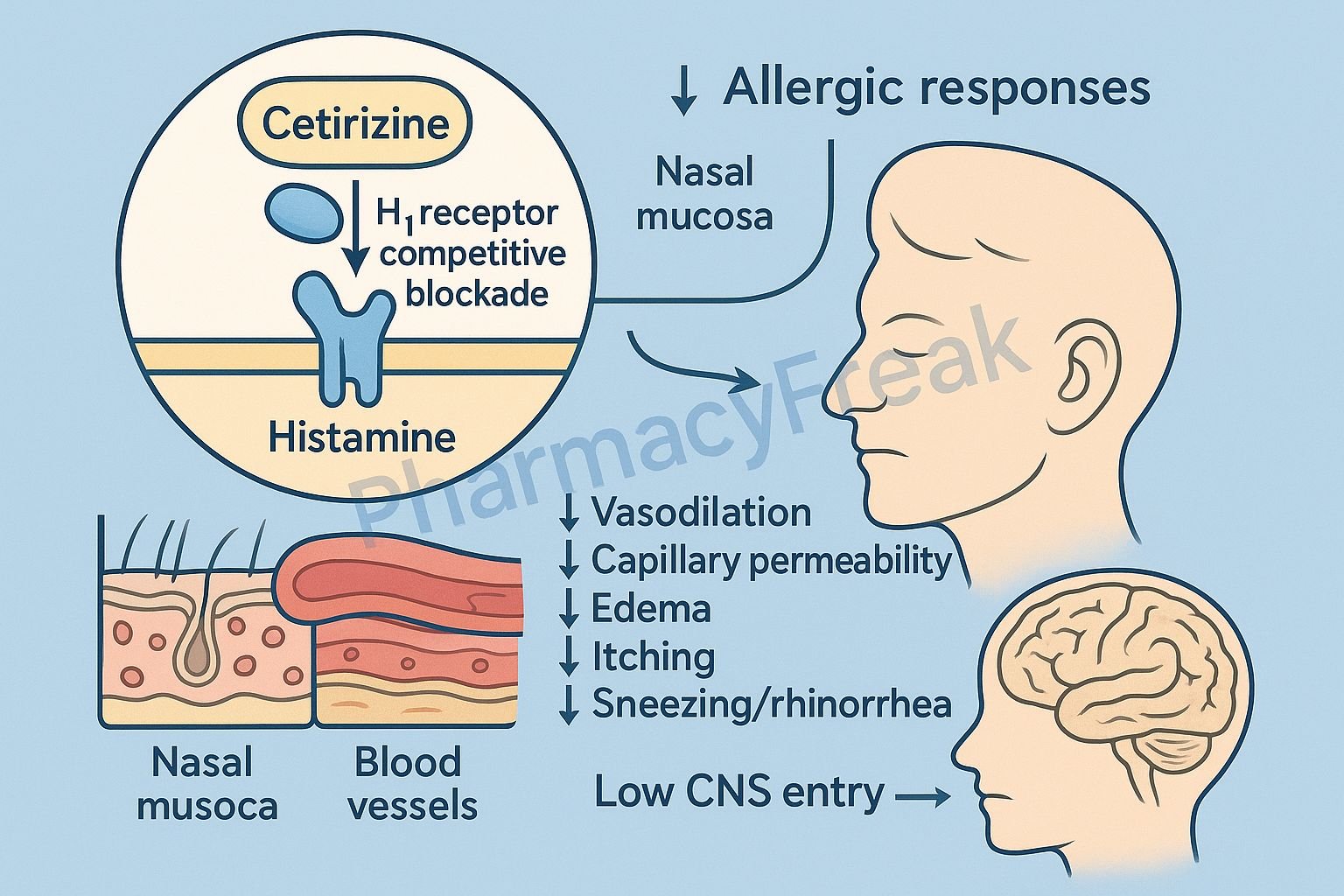
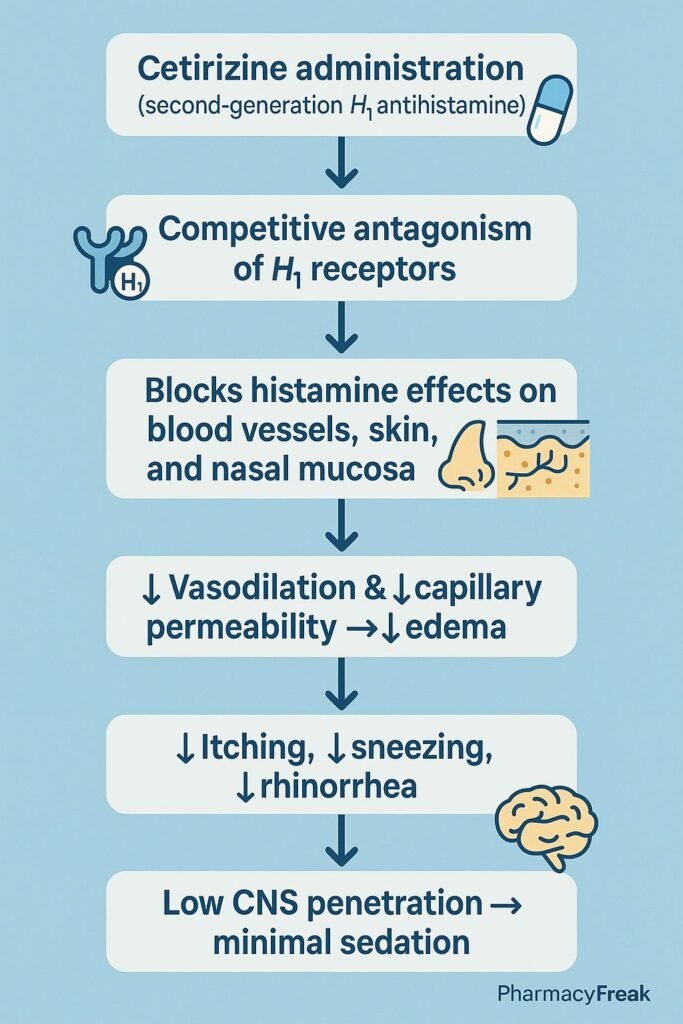
Cetirizine is a second-generation antihistamine widely used for the management of allergic rhinitis, urticaria, and other allergic disorders. It is favored for its minimal sedative effects, long duration of action, and excellent safety profile.
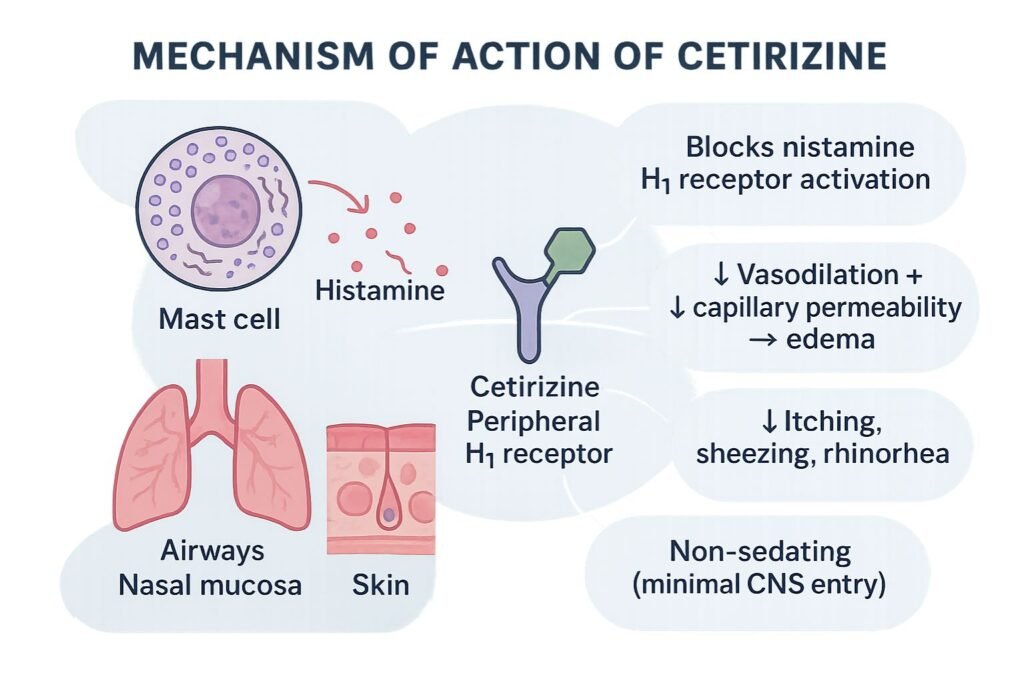
The Mechanism of Action of Cetirizine involves selective antagonism of peripheral H1 histamine receptors, reducing allergic symptoms such as itching, sneezing, rhinorrhea, and urticaria without significant central nervous system penetration.
Mechanism of Action (Step-wise)
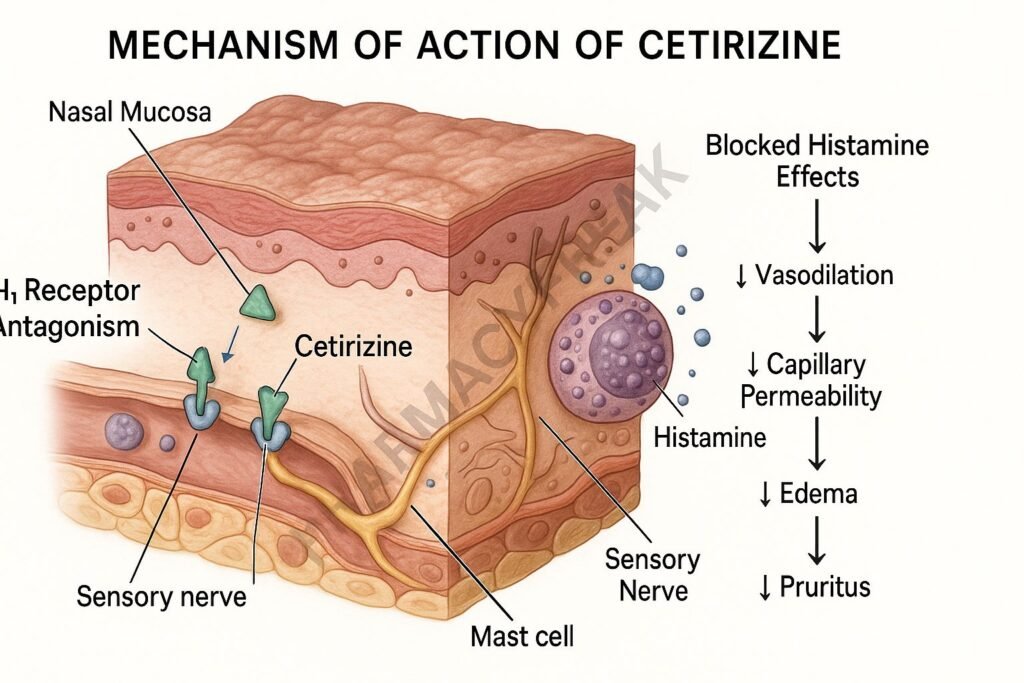
1. Selective H1 Receptor Antagonism – Primary Mechanism
Cetirizine is a potent and selective antagonist of H1 histamine receptors, especially in:
- Respiratory tract
- Vascular endothelium
- Sensory nerves
- Skin
Histamine normally causes:
- Vasodilation
- Increased vascular permeability
- Itching and sneezing
- Flare and wheal response
By blocking H1 receptors, cetirizine:
- ↓ Vasodilation
- ↓ Capillary permeability
- ↓ Edema
- ↓ Pruritus
- ↓ Nasal secretions
2. Peripheral Selectivity
Cetirizine is a second-generation antihistamine, meaning:
- Minimal penetration across the blood–brain barrier
- Less sedation compared to first-generation drugs (diphenhydramine, chlorpheniramine)
This is due to:
- High polarity
- P-glycoprotein efflux
- Low lipid solubility
3. Inhibition of Eosinophil Chemotaxis
Cetirizine decreases inflammatory cell migration in allergic responses.
Effects:
- ↓ Late-phase allergic reaction
- ↓ Chronic inflammation in allergic rhinitis
This provides prolonged symptom control.
4. Stabilization of Vascular Endothelium
Cetirizine reduces vascular leakage, thereby decreasing:
- Swelling
- Redness
- Urticaria lesions
5. Summary of Mechanism
| Mechanism | Effect |
|---|---|
| H1 blockade | ↓ Allergic symptoms |
| Peripheral selectivity | Minimal sedation |
| ↓ Eosinophil recruitment | ↓ Late-phase response |
| Stabilizes endothelium | ↓ Edema and urticaria |
Pharmacokinetics
- Route: Oral
- Onset: 1 hour
- Duration: 24 hours
- Protein binding: 93%
- Metabolism: Minimal hepatic metabolism
- Excretion: Mostly renal
Cetirizine is the active metabolite of hydroxyzine.
Clinical Uses
- Allergic rhinitis (seasonal and perennial)
- Urticaria (acute and chronic)
- Atopic dermatitis (symptomatic relief)
- Allergic conjunctivitis
- Angioedema (adjunct)
Adverse Effects
Common
- Mild sedation (less than first-generation antihistamines)
- Dry mouth
- Headache
- Fatigue
- GI discomfort
Rare
- Hypersensitivity reactions
- Tachycardia
- Hepatic dysfunction
Contraindications
- Severe renal impairment
- Hypersensitivity to cetirizine or hydroxyzine
- Caution in pregnancy and breastfeeding
Comparative Analysis
| Feature | Cetirizine | Loratadine | Diphenhydramine |
|---|---|---|---|
| Generation | Second | Second | First |
| Sedation | Low | Very low | High |
| Onset | Fast | Moderate | Fast |
| Drowsiness risk | Mild | Minimal | High |
| Anticholinergic effects | Minimal | Minimal | High |
MCQs
1. The primary mechanism of cetirizine is:
a) H2 receptor blockade
b) H1 receptor blockade
c) Leukotriene inhibition
d) Mast cell stabilization
Answer: b) H1 receptor blockade
2. Cetirizine causes minimal sedation because it:
a) Strongly blocks H2 receptors
b) Has poor blood–brain barrier penetration
c) Enhances serotonin levels
d) Has a short half-life
Answer: b) Has poor blood–brain barrier penetration
3. Cetirizine reduces late-phase allergic response by:
a) Blocking 5-LOX
b) Decreasing eosinophil chemotaxis
c) Blocking T-cell receptors
d) Inhibiting prostaglandin synthesis
Answer: b) Decreasing eosinophil chemotaxis
4. Cetirizine is the active metabolite of:
a) Loratadine
b) Diphenhydramine
c) Hydroxyzine
d) Fexofenadine
Answer: c) Hydroxyzine
5. Cetirizine is primarily excreted through the:
a) Liver
b) Lungs
c) Skin
d) Kidneys
Answer: d) Kidneys
FAQs
Q1. Does cetirizine cause drowsiness?
Yes, but significantly less than first-generation antihistamines.
Q2. Can cetirizine be taken daily?
Yes—commonly taken once daily for allergies.
Q3. Is cetirizine safe in children?
Yes—approved for pediatric use in age-appropriate doses.
Q4. How long does cetirizine take to work?
Onset begins within 1 hour.
Q5. Can it treat chronic urticaria?
Yes—it is a first-line therapy.
References
Goodman & Gilman’s Pharmacological Basis of Therapeutics
https://accesspharmacy.mhmedical.com/book.aspx?bookid=2189
Katzung: Basic and Clinical Pharmacology
https://accessmedicine.mhmedical.com/book.aspx?bookid=2464
Tripathi: Essentials of Medical Pharmacology
https://jaypeebrothers.com/
Harrison’s Principles of Internal Medicine
https://accessmedicine.mhmedical.com/book.aspx?bookid=2129

I am pursuing MBA in pharmaceutical management from NIPER Hyderabad with a strong academic record and proven success in national-level pharmacy entrance exams. I secured AIR 61 in NIPER 2024 (MS/M.Pharm) and AIR 27 in NIPER MBA, along with AIR 147 in GPAT 2024 and AIR 907 in GPAT 2023. I also achieved AIR 6 in AIIMS CRE-2025 for Drug Store Keeper and was selected as a Pharmacist (AIR 61) for ESIC. Additionally, I was the Runner-Up in Round 2 of the EY Case Study Competition.
At PharmacyFreak.com, I aim to guide future pharmacists through expert content, exam strategies, and insightful resources based on real experience and academic excellence.
Mail- harsh@pharmacyfreak.com