Table of Contents
Introduction
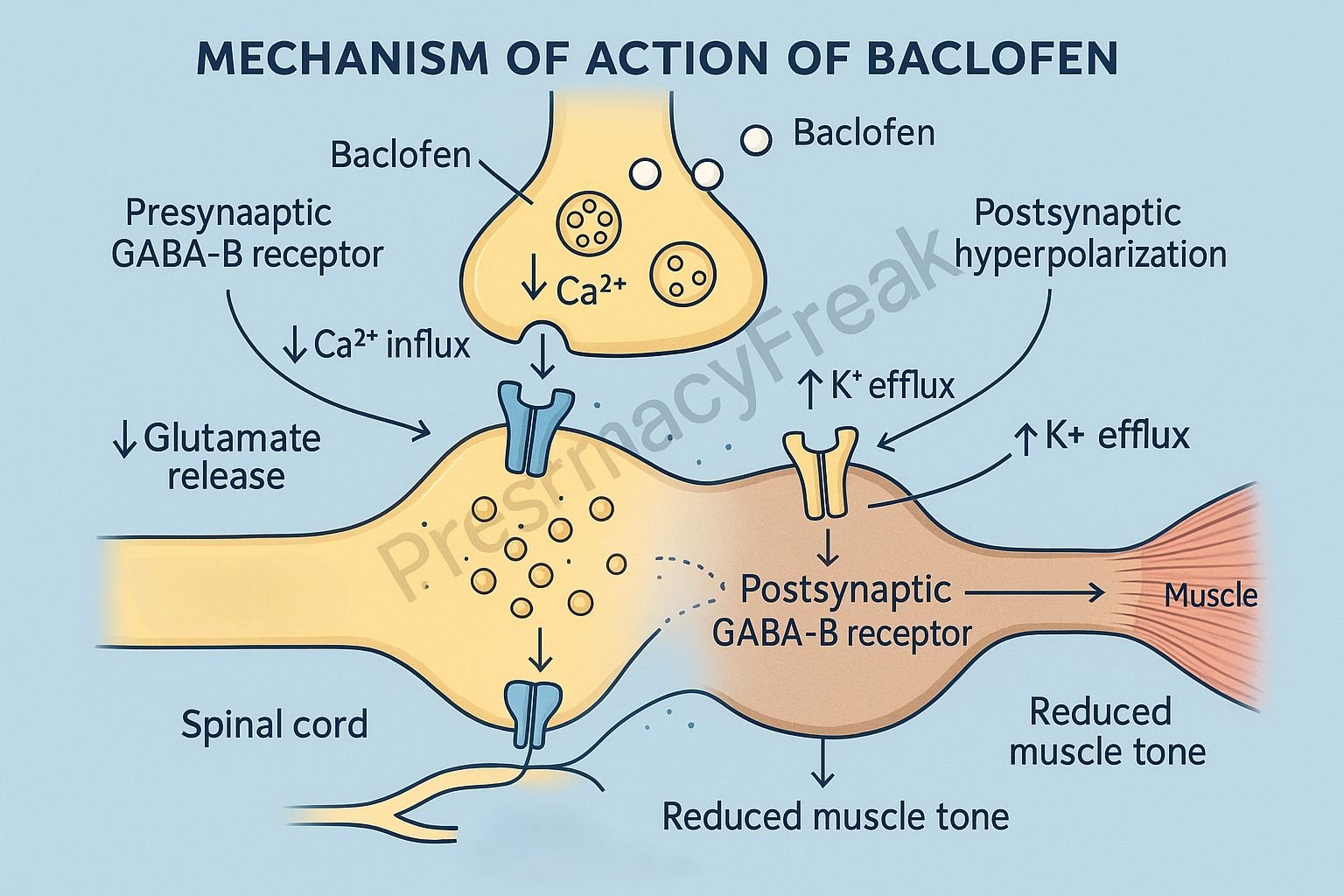
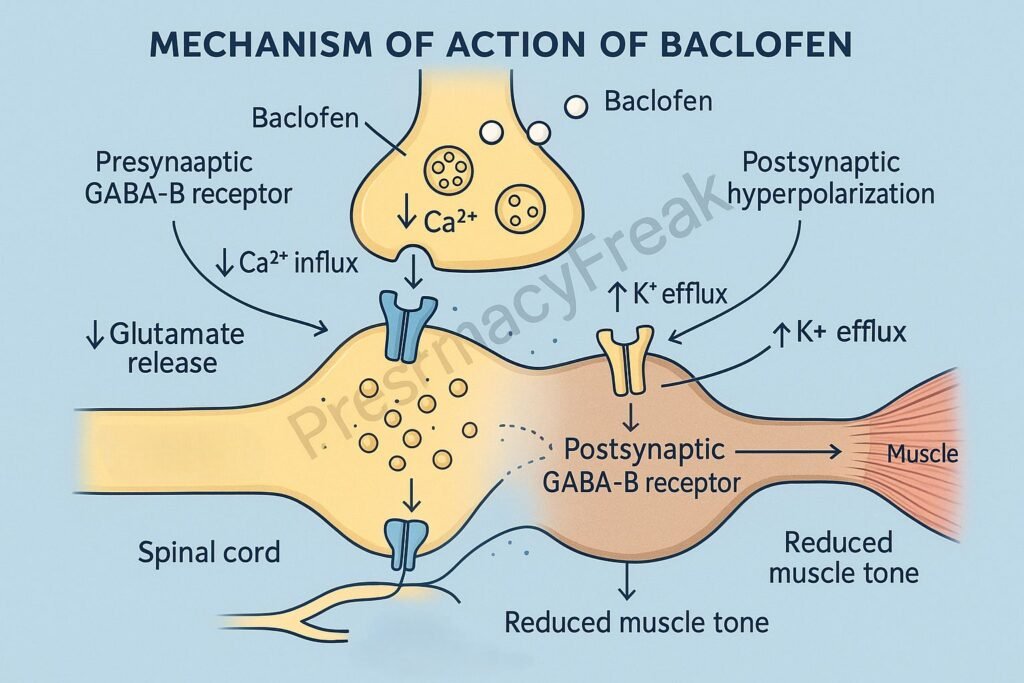
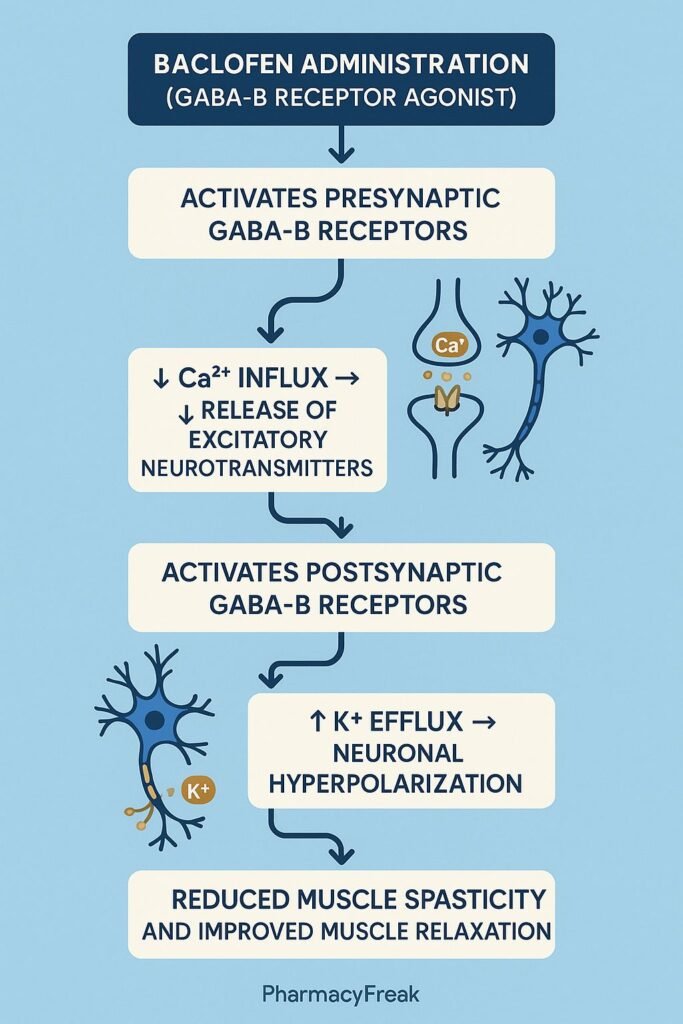
Baclofen is a centrally acting skeletal muscle relaxant primarily used for the management of spasticity associated with multiple sclerosis, spinal cord injury, and cerebral palsy. It acts as a selective GABA<sub>B</sub> receptor agonist, exerting inhibitory effects on both spinal and supraspinal pathways.
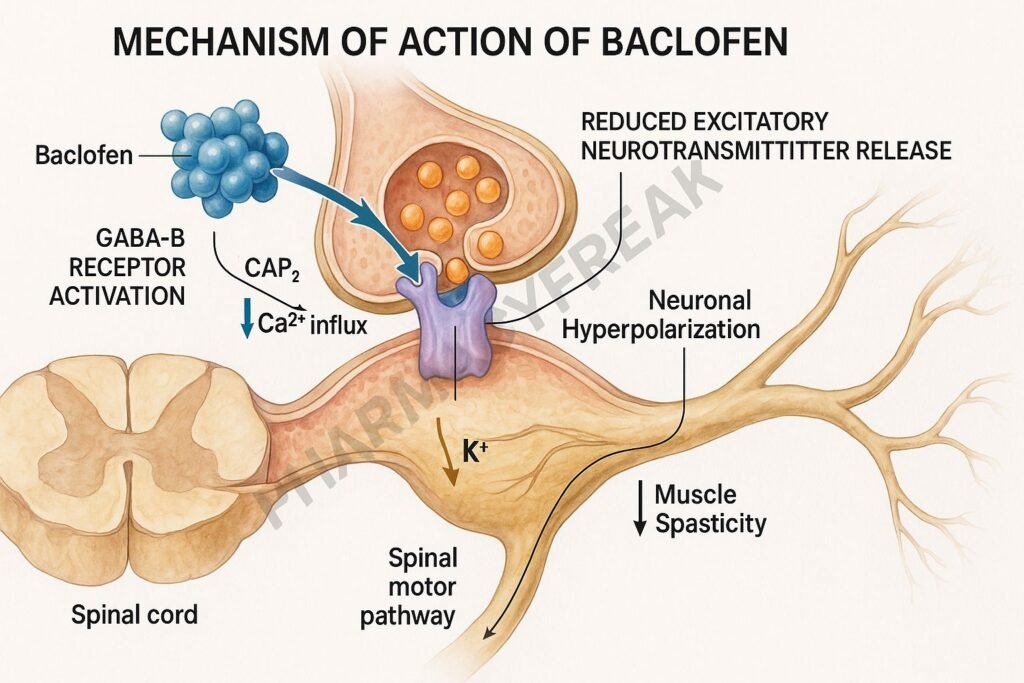
Mechanism of Action of Baclofen involves enhancing inhibitory neurotransmission through activation of GABA<sub>B</sub> receptors, resulting in hyperpolarization of motor neurons and decreased release of excitatory neurotransmitters like glutamate and aspartate. This leads to reduced muscle tone and suppression of spastic reflexes.
Mechanism of Action (Step-wise)
1. Activation of GABA<sub>B</sub> Receptors
- Mechanism:
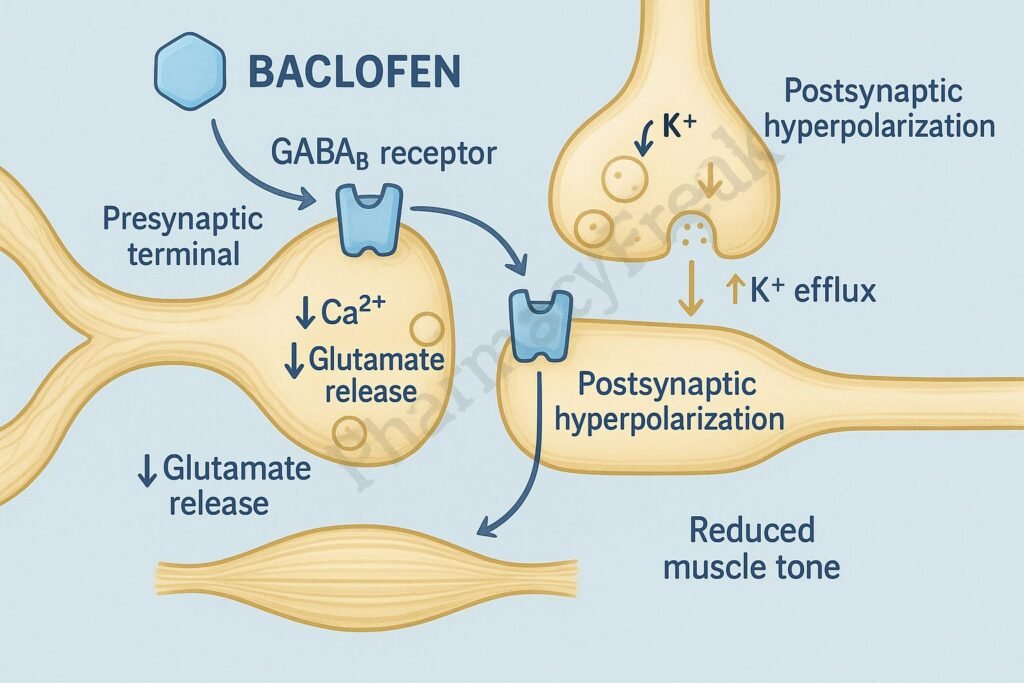
- Baclofen acts as a selective agonist at GABA<sub>B</sub> (metabotropic) receptors located both presynaptically and postsynaptically in the spinal cord.
- GABA<sub>B</sub> receptors are G-protein-coupled receptors (GPCRs) that modulate ion channels through second messengers.
2. Presynaptic Action – Inhibition of Excitatory Neurotransmitter Release
- Mechanism:
- On presynaptic terminals, baclofen activates GABA<sub>B</sub> receptors coupled to Gi proteins, which inhibit adenylyl cyclase activity, reducing cAMP formation.
- This leads to closure of voltage-gated calcium (Ca²⁺) channels, preventing Ca²⁺ influx into nerve terminals.
- As a result, the release of excitatory neurotransmitters such as glutamate, aspartate, and substance P is reduced.
- Effect:
- ↓ Excitatory neurotransmission → ↓ motor neuron stimulation → ↓ spasticity.
3. Postsynaptic Action – Hyperpolarization of Motor Neurons
- Mechanism:
- On postsynaptic neurons, baclofen increases potassium (K⁺) conductance, leading to efflux of K⁺ ions and membrane hyperpolarization.
- This inhibits postsynaptic depolarization and reduces the firing of alpha motor neurons.
- Effect:
- ↓ Neuronal excitability → ↓ muscle spasm and tone.
4. Overall Neural Effects
| Site of Action | Receptor Type | Effect of Baclofen |
|---|---|---|
| Presynaptic terminal | GABA<sub>B</sub> | ↓ Ca²⁺ influx → ↓ glutamate & aspartate release |
| Postsynaptic motor neuron | GABA<sub>B</sub> | ↑ K⁺ efflux → hyperpolarization |
| Spinal interneurons | GABA<sub>B</sub> | ↓ Reflex activity |
| Net Effect | — | ↓ Spasticity, ↓ muscle tone |
5. Key Summary of Actions
- Reduces monosynaptic and polysynaptic reflex transmission.
- Decreases excitatory neurotransmitter release.
- Hyperpolarizes motor neurons.
- Relieves skeletal muscle spasticity without significant reduction in voluntary strength.
Pharmacokinetics
- Absorption: Rapid and complete oral absorption.
- Onset: Within hours; maximum effect in 3–4 days.
- Distribution: Crosses the blood-brain barrier slowly; lipophilic analogs like intrathecal baclofen act faster.
- Metabolism: Limited hepatic metabolism (~15%).
- Elimination: Primarily renal (unchanged drug).
- Half-life: 3–4 hours (oral), 4–6 hours (intrathecal).
Clinical Uses
- Spasticity: Due to spinal cord injury, multiple sclerosis, cerebral palsy, stroke.
- Trigeminal neuralgia: Adjunct to carbamazepine in refractory cases.
- Hiccups: Persistent or intractable cases unresponsive to other treatments.
- Alcohol withdrawal: Off-label use for reduction of cravings and anxiety.
- Intrathecal therapy: Used in severe chronic spasticity unresponsive to oral therapy.
Adverse Effects
- Common: Drowsiness, dizziness, weakness, fatigue.
- Neurological: Confusion, ataxia, hallucinations (high doses).
- Cardiovascular: Hypotension, bradycardia (rare).
- Gastrointestinal: Nausea, constipation.
- Withdrawal (abrupt discontinuation): Seizures, hallucinations, rebound spasticity, hyperthermia, rhabdomyolysis.
Contraindications and Cautions
- Hypersensitivity to baclofen.
- Caution in renal impairment (dose adjustment required).
- Avoid abrupt withdrawal, especially with intrathecal administration.
Comparative Table: Baclofen vs Diazepam vs Tizanidine
| Feature | Baclofen | Diazepam | Tizanidine |
|---|---|---|---|
| Mechanism | GABA<sub>B</sub> agonist | GABA<sub>A</sub> facilitator | α₂-adrenergic agonist |
| Primary Action | Spinal inhibition | CNS sedation & muscle relaxation | Presynaptic inhibition |
| Sedation | Mild | High | Moderate |
| Withdrawal risk | Moderate | Mild | Moderate |
| Use | Spasticity (MS, SCI) | Spasm, anxiety | Spasticity, migraine |
MCQs
1. Baclofen acts primarily as an agonist at which receptor type?
a) GABA<sub>A</sub>
b) GABA<sub>B</sub>
c) NMDA
d) Glycine
Answer: b) GABA<sub>B</sub>
2. The presynaptic effect of baclofen involves:
a) Inhibition of K⁺ channels
b) Inhibition of Ca²⁺ influx and neurotransmitter release
c) Increased glutamate release
d) Activation of NMDA receptors
Answer: b) Inhibition of Ca²⁺ influx and neurotransmitter release
3. Baclofen reduces muscle spasticity mainly by:
a) Enhancing excitatory neurotransmission
b) Inhibiting excitatory neurotransmitter release
c) Stimulating nicotinic receptors
d) Blocking dopamine receptors
Answer: b) Inhibiting excitatory neurotransmitter release
4. The postsynaptic action of baclofen results in:
a) Depolarization
b) Hyperpolarization due to K⁺ efflux
c) Na⁺ influx
d) Ca²⁺ entry
Answer: b) Hyperpolarization due to K⁺ efflux
5. Baclofen is used primarily to treat:
a) Parkinson’s disease
b) Spasticity due to spinal cord lesions
c) Schizophrenia
d) Epilepsy
Answer: b) Spasticity due to spinal cord lesions
6. Sudden withdrawal of baclofen may lead to:
a) Respiratory depression
b) Rebound spasticity and hallucinations
c) Hypertension
d) Diarrhea
Answer: b) Rebound spasticity and hallucinations
7. Baclofen differs from diazepam because it:
a) Acts on GABA<sub>B</sub> receptors
b) Has more sedative effects
c) Is a benzodiazepine
d) Inhibits GABA metabolism
Answer: a) Acts on GABA<sub>B</sub> receptors
8. The main site of baclofen action is:
a) Neuromuscular junction
b) Spinal cord (dorsal horn and ventral horn)
c) Cerebral cortex
d) Peripheral nerves
Answer: b) Spinal cord (dorsal horn and ventral horn)
9. The intrathecal route of baclofen is preferred when:
a) Spasticity is mild
b) Oral baclofen is ineffective or poorly tolerated
c) Patient has seizures
d) In combination with benzodiazepines
Answer: b) Oral baclofen is ineffective or poorly tolerated
10. Baclofen decreases the release of which neurotransmitter?
a) GABA
b) Glutamate
c) Dopamine
d) Acetylcholine
Answer: b) Glutamate
FAQs
Q1. What makes baclofen different from benzodiazepines as a muscle relaxant?
Baclofen acts on GABA<sub>B</sub> receptors (metabotropic), while benzodiazepines act on GABA<sub>A</sub> receptors (ionotropic). Baclofen causes less sedation.
Q2. Why is intrathecal baclofen used in severe spasticity?
It allows direct delivery into the cerebrospinal fluid, achieving high spinal concentrations with minimal systemic effects.
Q3. Can baclofen cause withdrawal symptoms?
Yes, abrupt discontinuation can cause severe withdrawal reactions such as seizures, hallucinations, and rebound spasticity.
Q4. How does baclofen affect voluntary muscle strength?
At therapeutic doses, baclofen reduces spasticity without significantly impairing voluntary muscle strength.
Q5. What are the major contraindications for baclofen use?
Caution in renal impairment and epilepsy; avoid abrupt withdrawal.
References

I am pursuing MBA in pharmaceutical management from NIPER Hyderabad with a strong academic record and proven success in national-level pharmacy entrance exams. I secured AIR 61 in NIPER 2024 (MS/M.Pharm) and AIR 27 in NIPER MBA, along with AIR 147 in GPAT 2024 and AIR 907 in GPAT 2023. I also achieved AIR 6 in AIIMS CRE-2025 for Drug Store Keeper and was selected as a Pharmacist (AIR 61) for ESIC. Additionally, I was the Runner-Up in Round 2 of the EY Case Study Competition.
At PharmacyFreak.com, I aim to guide future pharmacists through expert content, exam strategies, and insightful resources based on real experience and academic excellence.
Mail- harsh@pharmacyfreak.com