Table of Contents
Introduction
Ketamine is a unique anesthetic agent known for its dissociative anesthesia and analgesic properties. It is widely used in emergency medicine, anesthesia, and pain management. Unlike conventional GABAergic sedatives, ketamine works primarily by antagonizing the NMDA receptor, resulting in a trance-like state with preserved airway reflexes and spontaneous respiration.
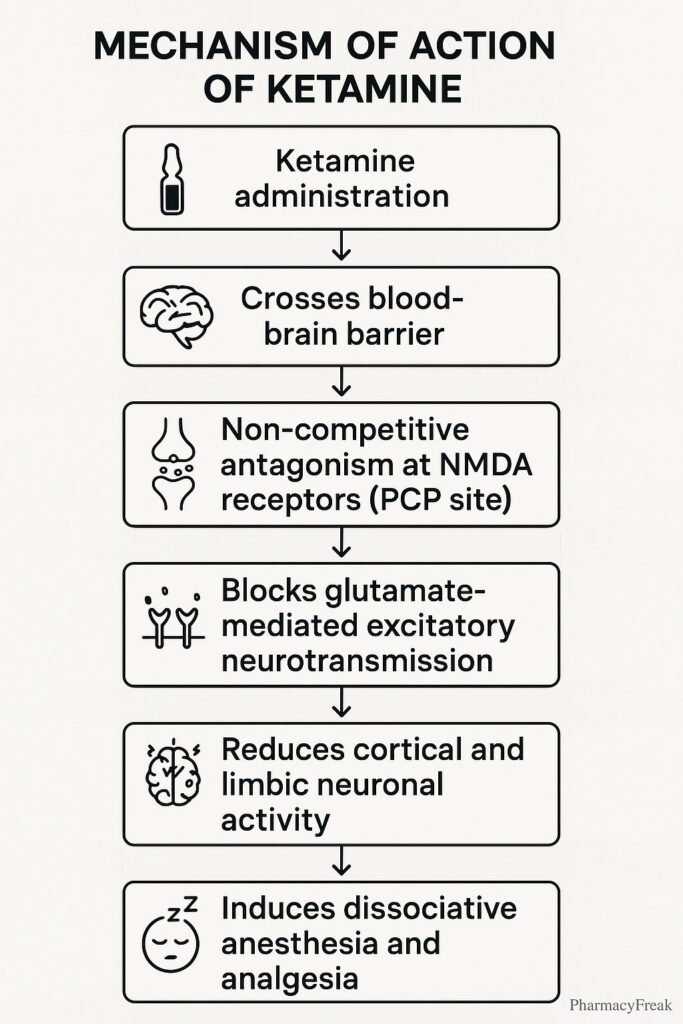
Mechanism of Action (Step-wise)
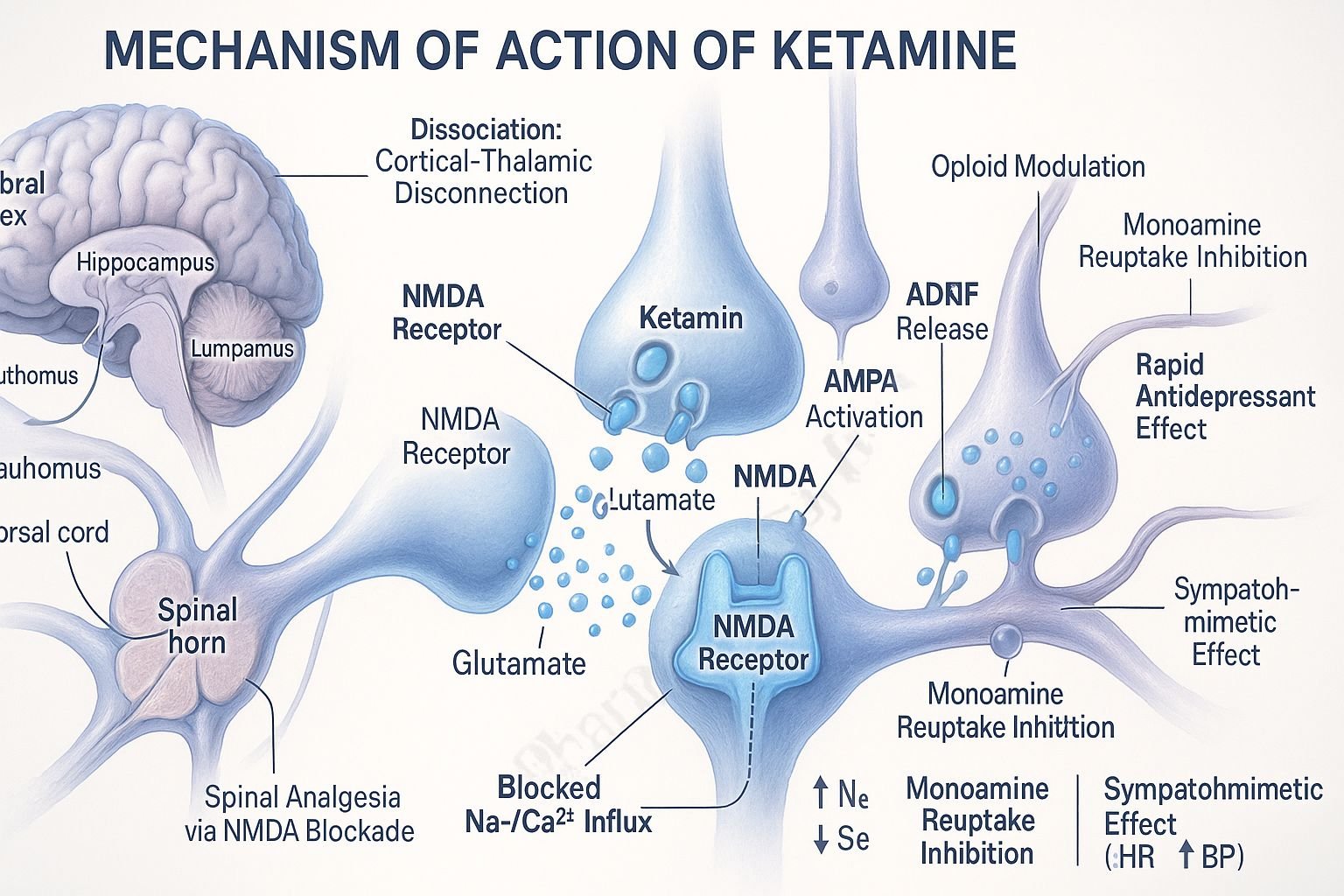
1. NMDA Receptor Antagonism
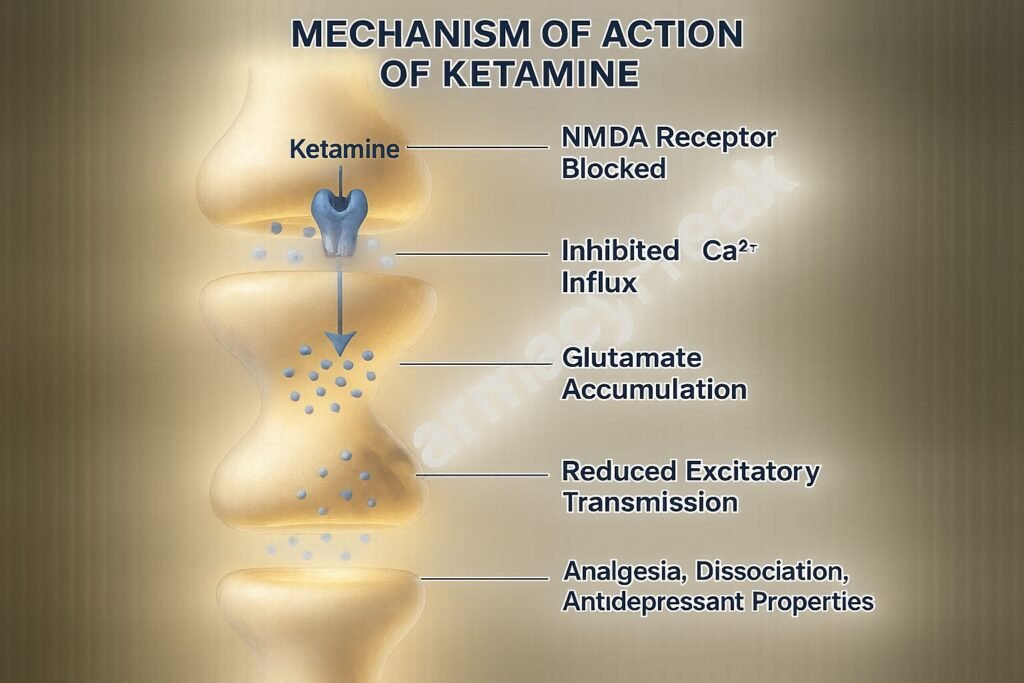
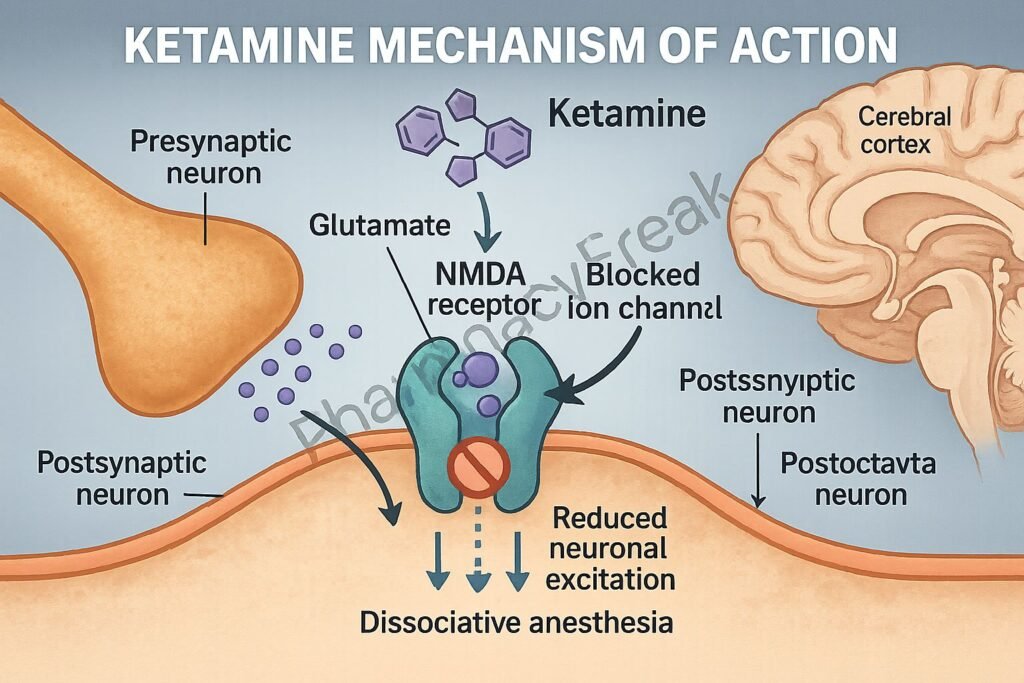
Ketamine noncompetitively inhibits the N-methyl-D-aspartate (NMDA) receptor by binding to the phencyclidine (PCP) site inside the receptor channel.
2. Reduction in Excitatory Neurotransmission
By blocking NMDA receptors, ketamine decreases glutamate-mediated excitatory neurotransmission in the central nervous system.
3. Dissociative Anesthesia
The blockade of NMDA receptors in the thalamocortical and limbic systems leads to a functional disconnection between sensory input and conscious perception—this is the basis of dissociative anesthesia.
4. Interaction with Opioid Receptors
Ketamine has partial agonistic effects at mu and kappa opioid receptors, contributing to its analgesic properties.
5. Modulation of Monoaminergic Pathways
It inhibits the reuptake of serotonin, dopamine, and norepinephrine, which may explain its antidepressant and mood-enhancing effects.
6. Stimulation of Sympathetic Nervous System
Ketamine indirectly stimulates the sympathetic nervous system, leading to increased heart rate, blood pressure, and cardiac output.
Pharmacokinetics
- Routes: IV, IM, intranasal, oral, subcutaneous, rectal
- Onset of Action: IV (30 seconds), IM (3–5 minutes)
- Duration of Action: IV (5–10 minutes), IM (12–25 minutes)
- Bioavailability: IV (100%), IM (93%), oral (17–24%)
- Metabolism: Hepatic via CYP3A4, CYP2B6, and CYP2C9 to active metabolite norketamine
- Excretion: Renal, primarily as conjugated metabolites
Clinical Uses
- Anesthesia: Induction and maintenance of anesthesia in various settings
- Analgesia: Acute and chronic pain management, particularly for opioid-resistant pain
- Procedural Sedation: In emergency and pediatric settings
- Treatment-Resistant Depression: Emerging use in low-dose formulations
- Status Asthmaticus: Due to bronchodilatory effects
- Burn Dressing Changes and Trauma: Where short-acting analgesia is required
Adverse Effects
- Psychomimetic Reactions: Hallucinations, emergence delirium
- Cardiovascular: Hypertension, tachycardia (due to sympathetic stimulation)
- Neurological: Increased intracranial and intraocular pressure
- Gastrointestinal: Nausea, vomiting, hypersalivation
- Abuse Potential: Risk of dependency and misuse due to euphoric effects
Comparative Analysis
| Feature | Ketamine | Propofol |
|---|---|---|
| Receptor Target | NMDA antagonist | GABA-A agonist |
| Respiratory Depression | Minimal | Significant |
| Cardiovascular Effects | Sympathomimetic (↑ HR, BP) | Hypotension, bradycardia |
| Onset (IV) | 30 seconds | 15–30 seconds |
| Duration | 5–10 minutes (IV) | 5–10 minutes (IV) |
| Use in Asthma | Yes (bronchodilator) | No |
Multiple Choice Questions (MCQs)
1. What is the primary mechanism of action of ketamine?
a) GABA-A receptor agonism
b) NMDA receptor antagonism
c) Serotonin receptor agonism
d) Acetylcholine receptor blockade
Answer: b) NMDA receptor antagonism
2. Ketamine is known to produce which type of anesthesia?
a) General anesthesia
b) Conscious sedation
c) Dissociative anesthesia
d) Regional anesthesia
Answer: c) Dissociative anesthesia
3. Which of the following is an advantage of ketamine over other anesthetics?
a) Causes hypotension
b) Suppresses sympathetic tone
c) Preserves airway reflexes
d) Causes respiratory depression
Answer: c) Preserves airway reflexes
4. Which active metabolite contributes to ketamine’s pharmacological effects?
a) Morphine
b) Norketamine
c) Lidocaine
d) Noradrenaline
Answer: b) Norketamine
5. A common psychological side effect of ketamine is:
a) Mania
b) Hallucinations
c) Depression
d) Cognitive dulling
Answer: b) Hallucinations
FAQs
Q1. Why is ketamine considered unique among anesthetics?
Because it produces dissociative anesthesia while preserving respiratory drive and airway reflexes.
Q2. Can ketamine be used in patients with asthma?
Yes, it has bronchodilatory properties and is beneficial in status asthmaticus.
Q3. What limits the oral bioavailability of ketamine?
Extensive first-pass hepatic metabolism significantly reduces its oral bioavailability.
Q4. Is ketamine suitable for patients with traumatic brain injury?
Use with caution due to potential elevation in intracranial pressure.
Q5. What is the role of ketamine in depression?
Low-dose ketamine is being explored for rapid-acting antidepressant effects in treatment-resistant depression.
References
- Goodman & Gilman’s The Pharmacological Basis of Therapeutics, 12th Edition
- KD Tripathi, Essentials of Medical Pharmacology, 7th Edition
- Clinical studies on ketamine’s NMDA antagonism and psychiatric effects
- Anesthesiology and Pain Management reviews
Related Internal Links

I am pursuing MBA in pharmaceutical management from NIPER Hyderabad with a strong academic record and proven success in national-level pharmacy entrance exams. I secured AIR 61 in NIPER 2024 (MS/M.Pharm) and AIR 27 in NIPER MBA, along with AIR 147 in GPAT 2024 and AIR 907 in GPAT 2023. I also achieved AIR 6 in AIIMS CRE-2025 for Drug Store Keeper and was selected as a Pharmacist (AIR 61) for ESIC. Additionally, I was the Runner-Up in Round 2 of the EY Case Study Competition.
At PharmacyFreak.com, I aim to guide future pharmacists through expert content, exam strategies, and insightful resources based on real experience and academic excellence.
Mail- harsh@pharmacyfreak.com