Mounting evidence of pharmacist burnout and increasing reports of suicides within the profession are fueling urgent calls for reform across the pharmacy industry, highlighting a crisis that threatens both practitioner well-being and patient safety. A growing number of pharmacists nationwide are facing overwhelming workloads, long hours, and pressure to meet strict performance metrics—factors now being linked to rising mental health risks and, in extreme cases, suicide.
Recent national data indicate that pharmacists are experiencing higher rates of burnout compared to many other healthcare professionals. Burnout, which the World Health Organization defines as chronic workplace stress that has not been successfully managed, manifests as emotional exhaustion, detachment, and reduced job satisfaction. In the pharmacy world, this often results from understaffed workplaces, long shifts, and increasing prescription volumes, leaving pharmacists with little time for breaks or self-care.
The alarming trend has drawn attention from advocacy groups, regulatory agencies, and pharmacy organizations alike. The American Pharmacists Association recently emphasized that unaddressed stress and exhaustion not only impact the mental health of pharmacists but also pose a direct threat to patient safety. Burned-out pharmacists are more prone to errors, which can have serious or even life-threatening consequences for patients receiving prescription medications.
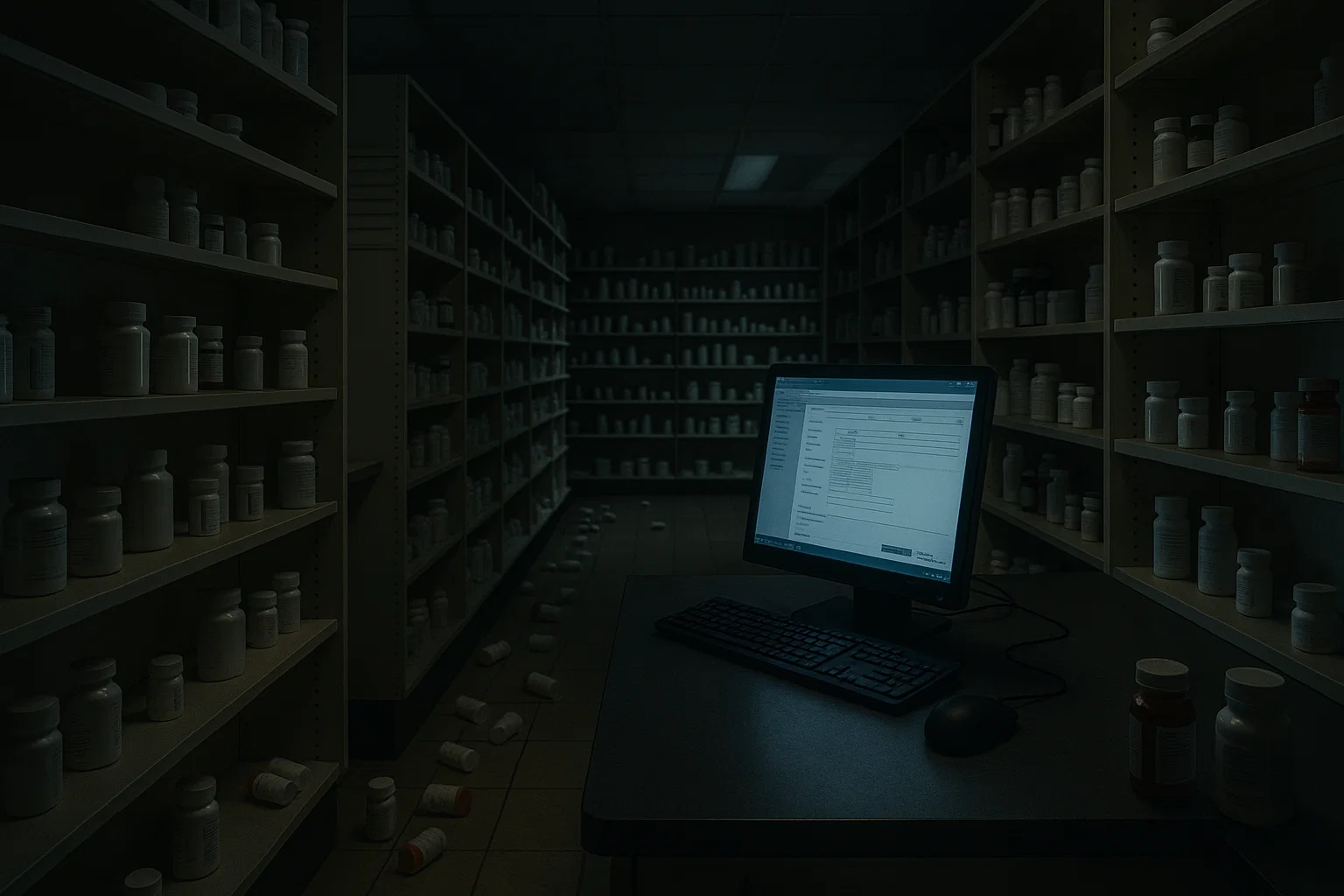
High-profile suicides and testimonies from pharmacists have cast a spotlight on the urgent need for systemic changes. Many practitioners describe feeling caught between corporate expectations and professional ethics, forced to balance speed and efficiency against the need for thoroughness and care. This pressure is particularly acute in chain pharmacies and high-volume retail settings, where strict quotas and reduced staffing levels are common.
Workplace stressors have also triggered broader conversations about the culture of pharmacy practice. Industry experts are calling for measures such as increased staffing, better access to mental health resources, and the establishment of safer, more supportive work environments. Some states have taken steps to require minimum staffing ratios or mandatory breaks, while others are urging pharmacy boards to strengthen oversight and hold employers accountable for unsafe working conditions.
Several pharmacy organizations are encouraging practitioners to seek support and counseling, emphasizing that mental health resources are available but often underused due to stigma or time constraints. Calls for reform are also being echoed by patient safety advocates, who warn that unaddressed burnout in pharmacy staff could undermine trust in the healthcare system as a whole.
The growing crisis is driving momentum for changes that could include regulatory reforms, better workplace standards, and a renewed focus on the well-being of those entrusted with patient care. As the pharmacy profession confronts these challenges, the message is clear: supporting pharmacists’ mental health is essential to ensuring safe and effective care for every patient.
The urgent issue of pharmacist burnout and suicide is not only a matter of practitioner well-being but also a critical concern for patient safety, driving the pharmacy profession toward meaningful change.

I am a Registered Pharmacist under the Pharmacy Act, 1948, and the founder of PharmacyFreak.com. I hold a Bachelor of Pharmacy degree from Rungta College of Pharmaceutical Science and Research. With a strong academic foundation and practical knowledge, I am committed to providing accurate, easy-to-understand content to support pharmacy students and professionals. My aim is to make complex pharmaceutical concepts accessible and useful for real-world application.
Mail- Sachin@pharmacyfreak.com